- Health Conditions A-Z
- Health & Wellness
- Nutrition
- Fitness
- Health News
- Ayurveda
- Videos
- Medicine A-Z
- Parenting
- Web Stories
Your Brain May Have Aged During The Pandemic, Even Without Getting COVID

Credits: Canva
Even if you never tested positive for COVID-19, the pandemic may have still left a trace in your brain. A new study published in Nature Communications by scientists at the University of Nottingham has revealed that living through the pandemic—even without infection—has biologically “aged” our brains. Using MRI brain scans and machine learning models, the research found signs of accelerated brain aging in people who endured the pandemic years, a change most notable in older adults, men, and socioeconomically disadvantaged individuals.
This isn’t just about stress or feeling low—researchers observed measurable structural changes in the brain, especially in white and grey matter. The findings also suggest that these changes may have accelerated brain aging by as much as five and a half months.
The research team, led by Dr. Ali-Reza Mohammadi-Nejad and supported by the UK Biobank, National Institute for Health and Care Research (NIHR), and the MRC DEMISTIFI programme, examined MRI brain scans of nearly 1,000 healthy adults. These scans were taken both before and after the pandemic. Using artificial intelligence and data from over 15,000 individuals, researchers trained a model to estimate “brain age”—a biological estimate of how old a brain appears structurally compared to the person’s actual age.
When comparing scans of people taken pre-pandemic to those taken after, the team observed notable structural changes associated with brain aging, particularly in those who had not contracted COVID-19. These findings raise the question: how could the mere experience of living through a pandemic affect our brains?
While the virus itself has been linked to cognitive decline and neurological damage, this study shows that just the psychological burden of the pandemic—lockdowns, isolation, anxiety about health and jobs may have had its own impact on brain health.
The researchers propose that the observed changes could stem from a mix of stress-induced neurobiological responses, decreased physical activity, disrupted sleep, dietary changes, increased alcohol use, or reduced social interaction. Brain regions affected by these factors overlap with those involved in memory, emotional regulation, and sensory processing functions often impaired in aging.
Professor Dorothee Auer, senior author on the study, noted, “This study reminds us that brain health is shaped not only by illness, but by our everyday environment.” And during the pandemic, that environment was far from ordinary.
Another striking aspect of the findings is who was most affected. The research found that men and individuals from socioeconomically disadvantaged backgrounds showed the greatest signs of accelerated brain aging.
People with fewer resources may have faced greater challenges—job loss, lack of healthcare access, limited social support—heightening the toll of pandemic-related stress. Additionally, male brains may respond differently to stress-related changes in white matter and inflammation, a hypothesis researchers continue to explore.
Still, it's worth noting that UK Biobank participants skew wealthier and healthier than the general UK population. In that sense, these findings may actually underestimate the brain-health toll on more vulnerable communities globally.
Does Brain Aging Translate to Cognitive Decline?
Interestingly, only participants who had been infected with COVID-19 showed clear declines in cognitive function, such as processing speed and mental flexibility. This suggests that the structural changes seen in uninfected individuals may not yet produce symptoms—or at least not obvious ones.
That said, the concept of “brain age” does matter. A brain that looks older than its actual age is associated with higher risk for diseases like Alzheimer’s and can affect emotional regulation and memory over time. It’s not a definitive diagnosis, but it’s a warning light.
Encouragingly, the study's authors believe the effects may be reversible. The brain has remarkable plasticity, its ability to adapt and recover from stress or injury. Lifestyle improvements, mental health support, exercise, sleep, and meaningful social connection may help restore cognitive resilience.
Are There Additional Neurological Concerns For People Who Had COVID?
Separately, a study conducted by NIMHANS (National Institute of Mental Health and Neurosciences, India) during the early months of the pandemic observed neurological complications in COVID-positive patients. Among 3,200 cases, 120 individuals developed conditions like stroke, encephalopathy, meningoencephalitis, and Guillain-Barré syndrome.
According to Dr. Netravathi M, professor of neurology at NIMHANS, COVID may impact both the central and peripheral nervous systems. These findings further underline how deeply the virus—and the environment it created—has influenced neurological health worldwide. Dr. Netravathi recommends a national registry to track long-term neurological outcomes from both COVID-19 infection and vaccination, underscoring the need for better monitoring and follow-up care.
This research serves as a wake-up call: even without physical illness, collective trauma has tangible effects on our brains. Mental and cognitive health must become a bigger part of post-pandemic recovery plans, not just in hospitals, but in homes, schools, and workplaces.
Governments and healthcare systems should support ongoing research into cognitive recovery, fund wellness programs, and make mental health care more accessible—especially for marginalized groups hit hardest by the pandemic.
For individuals, this means paying attention to brain health the same way we do blood pressure or weight. Regular exercise, meaningful social contact, cognitive stimulation, sleep, and stress management are not just good habits—they’re protective factors against premature brain aging.
Even if you escaped infection, your brain likely didn’t come through the pandemic unscathed. Structural aging linked to prolonged stress, social isolation, and lifestyle disruption is now being measured with hard data. But there’s hope: these changes may be reversible, and we now have an opportunity to prioritize brain health more consciously.
As Dr. Mohammadi-Nejad put it, “It really shows how much the experience of the pandemic itself—everything from isolation to uncertainty—may have affected our brain health.” Now, it’s up to us to invest in that recovery, not just physically, but mentally too.
NHS Pushes To Vaccinate 400,000+ Youths To Eliminated Cervical Cancer By 2040

Credits: Canva
The UK’s National Health Service (NHS) is launching a renewed and urgent call to vaccinate hundreds of thousands of young people against the human papillomavirus (HPV)—a virus linked to cervical and multiple other cancers. Despite robust efforts in schools, data from the last three years reveals that more than 418,000 children in the UK left school without receiving the HPV vaccine, prompting a national outreach initiative targeting those now aged 16 to 25.
This large-scale effort is not just about catching up; it’s part of a far-reaching goal- eliminating cervical cancer in the UK by 2040. With HPV responsible for 99.7% of cervical cancer cases and also linked to cancers of the throat, anus, penis, vagina, and mouth, the campaign reflects a bold public health strategy rooted in decades of scientific progress.
Also Read: New Parkinson's Treatment Is Like A Pacemaker To The Brain
HPV is one of the most common sexually transmitted infections globally. By age 45, about 80% of people—both men and women—will have contracted some form of HPV. While most of these infections are harmless and cleared naturally by the immune system, high-risk strains can linger and mutate healthy cells, leading to cancer.
In the cervix, HPV causes a gradual change in skin cells—a process called cervical dysplasia. This is where the transformation zone (the meeting point of squamous and glandular cells in the cervix) becomes the site of potential cancerous growth. If left unchecked, these abnormal cells can progress from CIN1 (mild dysplasia) to CIN2 or CIN3 (moderate to severe), and eventually become malignant.
What makes HPV particularly dangerous is its ability to evade apoptosis, the normal process where damaged cells self-destruct. Instead, it integrates its own genetic material into cervical cells, making them immortal and prone to uncontrollable growth.
In 2022 alone, 130,000 women across the European Economic Area (EEA)—which includes the EU, Iceland, Liechtenstein, and Norway—were newly diagnosed with cervical cancer, and 14,000 died. Even more alarming are the HPV-related head and neck cancers, which impacted 86,000 people in the region, 74% of them men, causing about 26,000 deaths.
The World Health Organization (WHO) defines cervical cancer elimination as fewer than four cases per 100,000 women. Current rates in the EEA sit at 56 per 100,000. Europe may reach the WHO's goal by 2050—but only if vaccination and screening efforts scale up dramatically.
The NHS is using every tool available to close this immunization gap. GP practices across England are now contacting unvaccinated individuals aged 16–25 through letters, emails, texts, and even the NHS App. The message is clear: one dose can save your life.
According to Dr. Amanda Doyle, NHS National Director of Primary Care and Community Services, "Too many lives are lost to cervical cancer… this vaccine is hugely important—not just for girls and women, but for boys and men too."
Previously, the vaccine required two doses, but as of 2023, a single dose is now recommended for most. This simplifies logistics and removes a barrier for many. National data from the 2023/24 academic year reveals progress, but also stark disparities. Among Year 10 students (ages 14–15):
- 76.7% of girls and 71.2% of boys were vaccinated.
- In Year 8 (ages 12–13), uptake was slightly lower: 72.9% of girls, 67.7% of boys.
Yet coverage varies dramatically by region:
- In London, Year 10 uptake for girls is just 64.9%, and only 58.9% for boys.
- In contrast, the South East boasts 82.7% (girls) and 77.3% (boys).
- At a hyperlocal level, places like Lambeth in London saw just 38.7% of girls vaccinated, compared to 97.6% in Northumberland.
- For boys, rates ranged from 28.2% (Lambeth) to 92.2% (West Berkshire).
This patchwork points to deep-rooted health inequalities—a challenge public health officials must address to ensure the vaccine’s promise reaches all communities.
Why It Is Important To Reinforce the Safety and Efficacy of the New Vaccine?
Since 2021, the UK has been administering an updated HPV vaccine that research shows is significantly more effective than earlier versions. Compared to the previous vaccine, the current one is expected to reduce women’s cancer cases by 16% and lower HPV-related deaths by 9%. What makes this advancement even more compelling is real-world data from England, which indicates the vaccine prevents up to 90% of cervical cancer cases. In practical terms, this means that for individuals who receive the vaccine before being exposed to the virus, the risk of developing cervical cancer is not just lowered—it’s almost entirely eliminated.
While cervical cancer remains the primary concern, the HPV vaccine offers protection against a wider range of serious health issues, including genital warts, anal cancer, penile cancer, and head and neck cancers—particularly those affecting the mouth and throat. This broader protection underscores the importance of vaccinating not just girls and women, but also boys and men. They face direct risks and also play a significant role in transmitting the virus to sexual partners, potentially putting others at risk for HPV-related cancers.
To accelerate progress, the NHS has outlined a clear roadmap in its 10-Year Health Plan. Key goals include achieving 90% HPV vaccine coverage among girls by 2040 and increasing participation in cervical screening programs. In a move to streamline access and engagement, the NHS recently rolled out a ‘ping and book’ system through its App, allowing eligible individuals to receive digital invitations and reminders for cervical screening appointments. Public health minister Ashley Dalton called the HPV vaccine “our most powerful tool” in eliminating cervical cancer but acknowledged that “there is still a long way to go” in reaching full coverage and equity.
And that’s the real message here: the science is ready. The infrastructure exists. What’s missing is participation—from parents, from young adults, and from the health systems that must ensure equitable access.
The effort to eliminate cervical cancer is no longer a medical fantasy—it’s a public health reality within reach. But it will take collective action, clear messaging, and targeted strategies to overcome gaps in access and awareness.
If you're between 16 and 25 in England and missed the jab in school, this is your moment. If you're a parent, ask your child’s GP. If you're a policymaker, look at your region’s numbers because the truth is simple: a single vaccine dose today could save a life tomorrow.
New Parkinson's Treatment Is Like A Pacemaker To The Brain

Credits: Canva
In a major leap for Parkinson’s disease treatment, a new form of brain implant is transforming the way patients experience relief from symptoms like tremors, stiffness, and slowness of movement. Often likened to a “pacemaker for the brain,” this breakthrough, known as adaptive deep brain stimulation (aDBS), is being hailed as a personalized, real-time therapy that adjusts to the brain's needs moment by moment.
From Reluctance to Relief: One Patient’s Journey
As the Scientific American reports, Keith Krehbiel had lived with Parkinson’s disease for nearly 25 years before agreeing to undergo a surgery he had long avoided. In 2020, as his symptoms worsened, he reluctantly said yes to a deep brain stimulation (DBS) implant, unaware he’d soon be part of a historic medical trial.
Just as he was preparing for surgery, neurologist Helen Bronte-Stewart of Stanford University received approval to launch a new trial testing an upgraded form of DBS. She offered Krehbiel the chance to be the first participant. His response: “Boy, do I!”
Five years on, the clinical trial, known as ADAPT-PD, involving 68 participants is now under review for publication. But the initial results have already been powerful enough to earn regulatory approval in both the U.S. and Europe.
What Makes Adaptive DBS Different?
As per the American Parkinson Disease Association (APDA), traditional DBS works by sending electrical impulses to parts of the brain that control movement, helping correct abnormal brain activity. But until now, it operated on fixed settings, adjusted manually by doctors based on patient feedback during clinic visits. That’s where adaptive DBS is changing the game.
This next-generation implant not only stimulates the brain but also listens to it. Using Medtronic’s BrainSense™ technology, the system continuously reads brain signals called local field potentials (LFPs), particularly in the beta-band frequency range, which has been linked to motor symptoms in Parkinson’s patients.
When the system detects brainwave patterns that suggest tremor, stiffness, or slowness, it automatically tweaks the stimulation levels in real-time.
“It’s like a smart pacemaker for the brain,” Bronte-Stewart explained. The goal is simple but revolutionary: deliver just the right amount of stimulation when it’s needed most, and ease off when it’s not.
A New Era for Parkinson’s Care
The implications of this adaptive technology are wide-reaching. APDA notes, over one million people in the U.S. and 1.2 million in Europe live with Parkinson’s, a progressive neurological disorder that often grows resistant to medications over time. While traditional DBS has helped around 200,000 patients worldwide, only 40,000 devices implanted since 2020 are equipped with the adaptive capability, and many of them haven’t even activated the feature yet.
With the ADAPT-PD trial results clearing regulatory hurdles, that’s poised to change. Krehbiel’s own experience is one reason why: after his surgery, his symptoms significantly improved, and his quality of life followed suit.
The benefits of adaptive DBS extend beyond Parkinson’s. Neurologists believe this “closed-loop” approach could also be effective for other movement disorders like Tourette’s syndrome, and even psychiatric conditions such as obsessive-compulsive disorder (OCD) and depression — though more trials are needed.
Experts believe the evolution of adaptive DBS is just beginning. Next on the horizon is the integration of artificial intelligence. By learning individual brain patterns, AI could help predict when symptoms are about to worsen, and adjust stimulation preemptively.
Rakesh Roshan Undergoes Angioplasty, Shares Health Update And Asks People Over 40 To Get Regular CT Scan
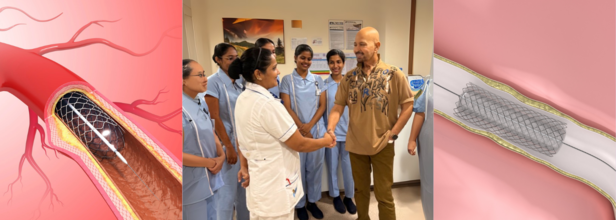
Credits: Canva and Instagram
Veteran filmmaker Rakesh Roshan, known for hits like Kaho Naa... Pyaar Hai and Krrish, opened up on Tuesday about his recent health scare that led to an urgent angioplasty procedure.
In a heartfelt Instagram post, the 74-year-old shared a photo from his hospital room, shaking hands with a nurse and thanking the medical team who cared for him.
While the photo appeared reassuring, his caption revealed a critical diagnosis that had, until recently, gone unnoticed.
Why Routine Checkups Are Important?
Roshan wrote that during a routine full-body check-up, a cardiologist recommended a sonography of the neck. This suggestion proved to be a turning point. “By chance, we found out that although asymptomatic, both my carotid arteries to the brain were above 75% blocked,” he shared. “Which, if ignored, could be potentially dangerous.”
Also Read: New Parkinson's Treatment Is Like A Pacemaker To The Brain
Without any outward symptoms, the condition could have led to a stroke or other serious complications. He immediately checked into the hospital to undergo “preventative procedures,” including angioplasty.
Now safely back home, Roshan says he feels well and is eager to resume his workouts. “I hope this inspires others to stay on top of their health, especially where the heart and brain is concerned,” he wrote.
A Reminder for Preventive Care Over Cure
The filmmaker urged everyone over the age of 45–50 to consider a CT scan for the heart and a carotid artery sonography as part of their annual health screenings. These tests, often overlooked, can detect hidden arterial blockages that may not present symptoms until it’s too late.
“I think it’s important to remember that prevention is always better than cure. I wish a healthy and aware year to you all,” he added.
His message was met with an outpouring of support from friends and well-wishers across the industry. Actors, including Anil Kapoor, Suniel Shetty, Tiger Shroff, and others left supportive comments and emojis. Roshan’s daughter Sunaina had also earlier confirmed to the media that her father had undergone an angioplasty “in his neck” and assured fans that he was “perfectly fine.”
What Is Angioplasty?
According to Johns Hopkins Medicine, angioplasty is a medical procedure used to restore blood flow through narrowed or blocked arteries. It is most commonly done to treat coronary artery disease but can also be used in other parts of the body, such as the carotid arteries leading to the brain.
The procedure involves inserting a thin, flexible tube called a catheter into a blood vessel. The catheter is guided to the blocked area, where a small balloon is inflated to compress plaque against the artery wall, thus opening the vessel and improving blood flow. In some cases, an atherectomy may also be performed to shave or remove the plaque.
The Role of Stents in Preventing Re-Narrowing
In nearly all modern angioplasty procedures, a stent is inserted to help keep the artery open. A stent is a tiny, mesh-like metal coil that is expanded at the site of blockage. Once placed, it prevents the artery from narrowing again.
There are two types of stents:
- Drug-eluting stents, which release medication to prevent scar tissue buildup
- Bare metal stents, which don’t have a drug coating but are used in patients who may be at higher risk of bleeding
Post-procedure, patients are typically prescribed antiplatelet medications to reduce the risk of blood clots and to ensure the stent remains open.
Risks and Follow-Up Care
While angioplasty is a relatively safe procedure, there can be complications if the stent becomes blocked or scar tissue develops. Some patients may require a repeat procedure or even radiation therapy (brachytherapy) to clear the narrowing.
That’s why ongoing medical supervision and lifestyle changes—such as regular exercise, a balanced diet, and avoiding tobacco—are key to long-term heart and brain health.
© 2024 Bennett, Coleman & Company Limited

