- Health Conditions A-Z
- Health & Wellness
- Nutrition
- Fitness
- Health News
- Ayurveda
- Videos
- Medicine A-Z
- Parenting
A Commonly Prescribed Gout Drug Could Lower Risk Of Heart Attack, Reveals Study

Credits: Canva
A low-dose of a cheap drug widely used to treat gout could reduce the risk of heart attack and stroke in people already living with heart disease, finds a to a new analysis. The findings are based on a major Cochrane review, which suggests that colchicine, a long-established medication for treating inflammation and pain could have a powerful role beyond its traditional use.
What Did The Study Find?
Colchicine is one of the first-line treatments for gout on the NHS, commonly prescribed to ease the sudden and severe joint pain associated with the condition. But researchers have long suspected that its anti-inflammatory properties may benefit people with cardiovascular disease as well. The new Cochrane review strengthens that theory.
The review analyzed 12 clinical trials involving 22,983 participants with a history of heart disease, previous heart attacks, or stroke. Out of these, 11,524 individuals were assigned a low daily dose of colchicine, typically 0.5 mg taken once or twice a day, and were monitored for cardiovascular outcomes over several months.
According to the findings, people with existing cardiovascular disease who took colchicine for at least six months were less likely to experience major cardiovascular events such as heart attacks or strokes. Researchers noted that inflammation plays a key role in plaque buildup and instability in the arteries, and colchicine’s ability to dampen inflammation may help reduce these risks.
Significant Reduction in Heart Attacks and Strokes
The review’s authors highlighted that the protective effect was clear and consistent across the trials. For every 1,000 people treated with low-dose colchicine, there were nine fewer heart attacks and eight fewer strokes compared with those who did not take the medication. While these numbers may appear modest, experts point out that at a population level, such reductions can translate into thousands of prevented events.
“Reductions like this can make a real difference for patients who live with ongoing, lifelong cardiovascular risk,” said Dr Ramin Ebrahimi, co-lead author from University Medicine Greifswald in Germany. The findings suggest that colchicine could become an accessible addition to current heart-disease prevention strategies, especially given its low cost and widespread availability.
Mild Side Effects Noted
Despite its potential benefits, colchicine is not risk-free. Participants taking the drug reported a higher incidence of gastrointestinal side effects, such as stomach discomfort or mild digestive issues. These reactions, however, were generally not severe enough to require discontinuing the medication.
Dr Lars Hemkens, senior author from the University of Bern in Switzerland, emphasized the importance of the findings, noting: “These results come from publicly funded trials repurposing a very old, low-cost drug for an entirely new use. It shows the power of academic research to reveal treatment opportunities that traditional drug development often overlooks,” as reported by Independent.
How Colchicine Works
According to the NHS, colchicine works by reducing inflammation triggered by the buildup of uric acid crystals in the joints, a hallmark of gout. Its anti-inflammatory action helps ease pain flare-ups. The medication is typically supplied in 500-microgram tablets, although the exact dosage varies depending on the individual's condition and treatment plan.
With growing evidence pointing toward its cardiovascular benefits, researchers say colchicine may soon be considered not just a gout medication, but a valuable tool in heart-disease prevention.
Can Alzheimer's Disease Be Fully Reversed? Here's What The New Study Says

Credits: iStock
Can Alzheimer's be completely reversed? This is not just about preventing it or ensuring it that the disease slow down, but can it be reversed to achieve full neurological recovery? For the longest, we have known that Alzheimer's is a progressive, degenerative brain disease, which destroys memory, thinking, and eventually the ability to perform simple tasks, but now a team of researchers from Case Western Reserve University, University Hospitals (UH), and Louis Stokes Cleveland VA Medical Center has challenged this belief. They may have found out something that could reverse it, at least so says the animal model.
Instead of targeting plaques or tangles alone, the team looked at something more fundamental: the brain’s energy system.
Their findings, published in Cell Reports Medicine, suggest that restoring the brain’s energy balance may not just slow Alzheimer’s but potentially reverse key features of the disease, at least in animal models.
What Did The Study Find?
The study is led by Kalyani Chaubey from the Pieper Laboratory, and at the center of the study is NAD+, a molecule essential for cellular energy and repair.
NAD+ levels naturally decline with age across the body, including in the brain. When levels drop too low, cells struggle to perform basic functions and eventually fail.
The researchers found that this decline is far more severe in the brains of people with Alzheimer’s. The same sharp drop was also seen in mouse models of the disease, pointing to a shared biological problem.
How the study was conducted
While Alzheimer’s is uniquely human, scientists use specially engineered mice to study it. In this study, two types of mice were used. One model carried human mutations linked to amyloid buildup, while the other carried a mutation affecting the tau protein.
Both amyloid and tau are central to Alzheimer’s pathology. Over time, these mice developed symptoms similar to human Alzheimer’s, including brain inflammation, damage to nerve fibers, breakdown of the blood-brain barrier, reduced formation of new neurons, and severe memory and learning problems.
Restoring energy balance in diseased brains
After confirming that NAD+ levels were dramatically reduced, the researchers tested whether restoring this balance could help. They used a drug called P7C3-A20, developed in the Pieper Laboratory, which supports cells in maintaining healthy NAD+ levels under stress.
Remarkably, the results went beyond prevention. Even when treatment began after significant disease progression, the mice showed reversal of major brain damage. Cognitive function fully recovered in both mouse models, despite their different genetic causes.
Biomarkers and what they signal
The recovery was not just behavioral. Blood levels of phosphorylated tau 217, a biomarker now used clinically in humans to detect Alzheimer’s, returned to normal in treated mice. This provided objective evidence that disease processes had been reversed, not merely masked.
Why this matters for people
The findings suggest a possible paradigm shift. Alzheimer’s damage may not always be permanent. Under certain conditions, the brain appears capable of repairing itself and regaining function.
However, the researchers caution against self-medicating with over-the-counter NAD+ supplements. Some have been shown in animal studies to raise NAD+ to unsafe levels that may increase cancer risk. The drug used in this study works differently, supporting balance rather than excess.
What Is Type 5 Diabetes? All You Need To Know About The Newly Identified Condition
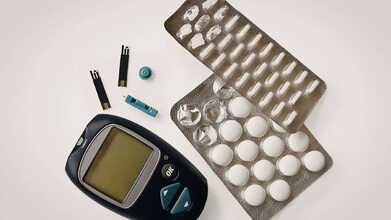
Credits: Canva
A newly recognised form of diabetes is reshaping how scientists and doctors view the condition, particularly in countries like India. In 2025, global health authorities officially acknowledged Type 5 diabetes as a separate and distinct form of the disease.
This recognition ended decades of confusion around a type of diabetes that did not fit neatly into the existing categories of Type 1 or Type 2 diabetes. The formal classification, backed by the International Diabetes Federation and supported by research published in The Lancet Global Health, is expected to transform diagnosis, treatment, and long-term care for millions of people worldwide.
But what exactly is Type 5 diabetes, and how does it differ from the types of diabetes that are more widely known?
What Is Type 5 Diabetes?
Type 5 diabetes is now recognised as a distinct form of the disease caused primarily by severe, long-term malnutrition, often experienced during childhood. This undernutrition can lead to profound insulin deficiency and an underdeveloped pancreas, resulting in significantly reduced insulin production.
Unlike Type 1 diabetes, which is autoimmune, or Type 2 diabetes, which is linked to insulin resistance, Type 5 diabetes arises from nutritional deficiencies that impair the pancreas’s ability to function properly.
It most commonly affects lean young adults in low-income regions. For years, people with this condition were misdiagnosed as having Type 1 diabetes or an unusual form of Type 2, often leading to inappropriate treatments that failed to address the root cause.
Type 5 Diabetes Symptoms
Symptoms of type 5 diabetes can resemble those seen in other forms of diabetes, such as excessive thirst, frequent urination, persistent tiredness, unexplained weight loss, blurred vision, and slow-healing wounds. However, they are often paired with indications of malnutrition, including a lean physique, delayed growth or puberty in young people, anemia, and recurring infections.
These arise from nutritional deficiencies during early life rather than solely from insulin resistance or autoimmune causes, and they usually present before the age of 30, according to the International Diabetes Federation.
Type 5 Diabetes: Scientists Demand Recognition
Researchers have been studying this condition for decades, particularly in parts of Asia and Africa. Yet, without official recognition, the disease remained poorly understood, and patients were rarely diagnosed correctly. Experts argued that grouping these patients under existing categories obscured the true cause of their illness.
The 2025 classification now formally separates Type 5 diabetes from other types, making it easier to study, identify, and manage. In India, where diabetes prevalence is already high, this recognition is particularly relevant. Tens of millions of people live with diabetes in the country, many of whom remain undiagnosed. Type 5 diabetes highlights a different pattern: it develops not from excess calories, but from too little nutrition during childhood, creating a double burden in regions where obesity and undernutrition coexist.
Implications for Diagnosis and Care
Although there is no new treatment specifically for Type 5 diabetes yet, official recognition marks a major step forward. Doctors can now approach lean patients with a history of malnutrition more carefully, avoiding a “one-size-fits-all” approach. Clearer classification could lead to better guidelines, more personalised care, fewer complications, and improved long-term outcomes.
Experts believe that understanding the role of childhood undernutrition in diabetes could eventually reshape how we prevent, monitor, and manage the condition—something countries like India urgently need as diabetes numbers continue to rise.
This Common Cold Like Symptom Might Actually Be An Early Sign Of Dementia

Credits: Canva
An early sign of dementia can sometimes look like a common winter-related issue. When this symptom appears along with other warning signals, it may be wise to speak to a doctor. Dementia is a syndrome marked by a collection of related symptoms that point to a gradual decline in brain function. Over time, this can affect memory, behaviour, thinking, and even movement. In its early phase, however, dementia often shows up through subtle changes that are easy to overlook or mistake for something less serious.
This Common Cold Like Symptom Might Actually Be An Early Sign of Dementia
Dementia UK notes that one possible early indicator of dementia is “low mood, anxiety or depression”. Its specialists explain: “In the early stages of dementia, people often begin to notice symptoms that interfere with day-to-day life.” The difficulty is that low mood or depression can also be linked to seasonal affective disorder (SAD), a form of depression that tends to appear during winter and ease as the days become longer and brighter.
Symptoms of Seasonal Affective Disorder (SAD)
The NHS lists the following possible symptoms of SAD:
- Low mood
- Loss of interest in activities you usually enjoy
- Feelings of guilt, hopelessness or worthlessness
- Feeling restless, tense or easily irritated
- Problems with concentration
- Increased appetite and eating more than usual
- Feeling very tired and sleeping more than usual
- Thoughts of suicide or self-harm
Dementia Early Symptoms
Dementia UK also highlights other possible early signs of dementia, including:- Problems with memory and concentration
- Difficulties with language and communication, such as struggling to find words or follow conversations
- Difficulties with planning, problem-solving and making decisions
- Getting lost in familiar places because of problems with orientation and reduced ability to recognise usual cues, such as signs or landmarks
- Changes in behaviour and personality, such as becoming more withdrawn or less patient
How Early Symptoms May Differ Between Dementia Types
The organisation explains: “A person experiencing early symptoms of dementia may notice these changes themselves, or they may be picked up first by family members, friends or colleagues. Memory problems are not always obvious in the early stages of some types of dementia, such as frontotemporal dementia, where changes in behaviour and personality may appear first.
“People with young onset dementia, where symptoms begin before the age of 65, are also less likely to have memory loss as an early symptom.”
Emotional Changes Linked To Specific Forms Of Dementia
The charity also points out that emotional changes can be linked to two specific types of dementia. In vascular dementia, a person may experience “changes in mood, behaviour and personality”, while Lewy body dementia can cause “mood changes, including anxiety and depression”.
Dementia: Why These Symptoms Can Be Hard To Identify
That said, it is often difficult to know at first whether dementia is the cause of these warning signs. Dementia UK advises: “Many symptoms associated with dementia can also be caused by other physical or mental health conditions, such as thyroid disorders, menopause, vitamin B12 deficiency, depression, anxiety, work-related stress or relationship difficulties.
“This means that experiencing symptoms linked to dementia does not automatically mean someone has the condition. However, if you or someone close to you is showing signs or symptoms of dementia, it is important to visit a GP to understand what might be causing them.”
When To Seek Medical Advice
If you or someone you know is showing symptoms that resemble dementia, seeking advice from your GP is an important first step.
© 2024 Bennett, Coleman & Company Limited

