- Health Conditions A-Z
- Health & Wellness
- Nutrition
- Fitness
- Health News
- Ayurveda
- Videos
- Medicine A-Z
- Parenting
A Simple Blood Test Could Detect Signs Of Ovarian Cancer

Credits: Canva
A simple blood test may soon transform the way ovarian cancer is diagnosed. Researchers say this new tool, which relies on advanced machine learning, can identify the disease in its earliest stages with remarkable accuracy. If approved, experts believe the test could be integrated into the UK’s National Health Service (NHS), offering hope for thousands of women.
Ovarian cancer is often dubbed the “silent killer” because its early symptoms, such as bloating, pelvic pain, or frequent urination, can be vague and easily mistaken for less serious conditions. According to Cancer Research UK, more than 7,500 women are diagnosed with ovarian cancer annually, most commonly after the age of 50. Unfortunately, many cases are discovered late, when treatment options are limited and outcomes less favorable.
What is Ovarian Cancer?
Ovarian cancer develops when abnormal cells in the ovaries grow uncontrollably, sometimes spreading to other parts of the body. It is one of the deadliest gynaecological cancers because of late detection. The survival rate is significantly higher if the disease is caught in its early stages, around 93% of women diagnosed at stage one survive at least five years compared to just 13% for those diagnosed at stage four, according to the American Cancer Society.
Currently, diagnosis usually involves a combination of ultrasound scans, existing blood tests, and sometimes biopsies. Yet, these methods often fail to catch the disease soon enough. This is where the new blood test could be a game-changer.
How the Test Works
Developed by AOA Dx, the test looks for what cancer cells shed into the bloodstream. Cancerous cells release tiny fragments containing lipids (fat-like molecules) and proteins, which together act like a biological fingerprint for ovarian cancer.
The test then uses a machine-learning algorithm trained on thousands of patient samples to analyse these biomarkers. This allows it to detect patterns invisible to the human eye and to distinguish ovarian cancer from other conditions with much greater accuracy than current tools.
Alex Fisher, chief operating officer and co-founder of AOA Dx, explained: “The test can detect the disease at early stages and with greater accuracy than current tools.”
Dr Abigail McElhinny, the company’s chief science officer, added that combining multiple biomarker types into one platform allows the detection of ovarian cancer across different subtypes and stages.
Study Findings Show Strong Accuracy
The potential of this test has been highlighted by research published in the journal Cancer Research Communications, led by teams at the University of Manchester and the University of Colorado.
Testing 832 samples, the results were striking:
- In samples from Colorado, the test detected ovarian cancer correctly in 93% of all stages and 91% of early stages.
- In Manchester samples, accuracy stood at 92% across all stages and 88% in early stages.
Professor Emma Crosbie, gynaecological oncology expert at the University of Manchester, said: “AOA Dx’s platform has the potential to significantly improve patient care and outcomes for women diagnosed with ovarian cancer. We are eager to continue advancing this research through additional trials.”
Hope for the Future
If larger trials confirm these findings, the blood test could become a routine diagnostic tool, helping identify ovarian cancer earlier than ever before. This would not only save lives but also reduce healthcare costs by allowing treatment when the disease is most manageable.
For women, particularly those over 50 or with a family history of ovarian or breast cancer, this breakthrough could provide reassurance and a better chance at survival. While the test still awaits regulatory approval, experts are hopeful that it marks a turning point in the fight against ovarian cancer.
Five Essential Health Tests to Consider This Winter, According To A Doctor

Credits: iStock
Winter in India is often associated with sardio ke laddoo, but also with increasingly sedentary lifestyle, worsening air pollution, all of which leads to more time spending home than to going out, taking a stroll, working out and more. This is why as winter sets in, India also sees a quiet but consistent rise in non communicable diseases, or NCDs, conditions that now account for nearly two thirds of all deaths in the country. Heart disease, diabetes, thyroid disorders, fatty liver disease and arthritis continue to rise across age groups, driven by sedentary lifestyles, dietary excess and delayed diagnosis.
Winter can further aggravate these risks. Physical activity drops, calorie dense foods become routine, sunlight exposure reduces and metabolism changes. Studies and hospital data in India have repeatedly shown that heart attacks and strokes tend to spike during colder months. Blood vessels constrict, blood viscosity increases and cholesterol levels often rise. Blood sugar control also becomes more challenging, while joint pain and stiffness worsen for many.
Dr. Mayanka Lodha Seth, Chief Pathologist at Redcliffe Labs, says the problem is not seasonal food but seasonal neglect. “Traditional winter foods are not harmful on their own. The real risk comes from consuming them without understanding what is happening inside the body,” she explains. “Winter tends to mask symptoms while quietly worsening internal imbalances.”
With India already home to over 100 million people living with diabetes and a similar number estimated to be prediabetic, preventive testing becomes crucial. Doctors recommend five key tests that can offer a clearer picture of health before winter indulgence begins.
Blood Sugar Levels
Diabetes is one of the fastest growing NCDs in India, and a large proportion of cases remain undiagnosed. Winter diets high in sugar and fat can trigger frequent glucose spikes. Testing fasting blood sugar and HbA1c helps identify early risk and prevents long term complications affecting nerves, kidneys and the heart.
Lipid Profile
High cholesterol is a major contributor to cardiovascular disease, which remains India’s leading cause of death. Reduced activity in winter often pushes lipid levels higher. A lipid profile helps assess heart risk and guides dietary and lifestyle moderation before damage sets in.
Liver Function Test
Non alcoholic fatty liver disease is increasingly common in India, even among younger adults. Excess sugar and fat intake during winter can worsen liver fat accumulation. Early liver testing can flag reversible changes before they progress to chronic liver disease.
Thyroid Function Test
Thyroid disorders affect millions in India, especially women, and often go unnoticed. Symptoms like weight gain, fatigue and cold intolerance are frequently brushed off as winter sluggishness. A simple thyroid test helps distinguish seasonal lethargy from hormonal imbalance.
Vitamin D and Vitamin B12 Levels
Vitamin D deficiency is widespread due to limited sun exposure in winter, while Vitamin B12 deficiency remains common because of dietary patterns. Both deficiencies are linked to low immunity, muscle pain, bone weakness and worsening joint discomfort.
Dr. Seth adds, “Preventive diagnostic testing allows people to make informed choices. It helps them enjoy winter foods in moderation without unknowingly worsening an underlying condition.”
As NCD related healthcare costs continue to rise in India, early testing offers both health and financial protection. Winter comfort does not have to come at the cost of long term health. Staying informed may be the most effective preventive step this season.
Tamiflu Isn't The Only Flu Medicine, Expert Shares Other Alternative
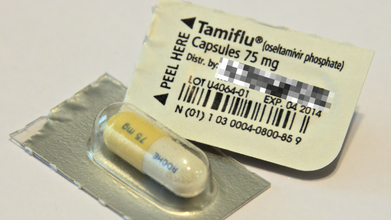
Credits: iStock
Flu season is hitting hard this year, and the symptoms could feel relentless. People are suffering from rising fever, hacking cough, blocked and stuffy nose and sore throat. While many people get relief from Tamiflu, which is a prescribed antiviral medication that is used to treat or even to prevent illness, there are other alternatives available too.
Dr Ari Brown, a Texas based pediatrician and the author of Baby411 book series told CNN health that one of the most common complaints that she gets to hear from Tamiflu is vomiting. A 2023 study published in the Pediatric Infectious Disease Journal notes that 18% of people experienced vomiting with Tamiflu, as compared to 5% with Xofluza, an alternative.
“I’ve also had a few pediatric patients experience moodiness with Tamiflu, which is reported in the literature,” she said.
Read: Adenovirus Cases Rise In UK, Health Authorities On Alert
Tamiflu is usually gives to treat flu in people ages 2 weeks and older and to reduce the chance of getting the flu in people 1 year and older. The medicine could be administered in both form, liquid and capsules and usually taken twice daily for five days straight. This is prescribed for when flu is to be treated. However, when used for prevention, it is typically taken once for 10 days.
What Are The Other Alternatives Available For Flu Treatment?
Xofluza: It is administered as a single dose tablet and is approved for ages 5 and older. This medicine can also be used to treat or to prevent the flu. While it costs nearly $200 for those without insurance, eligible patients can use coupons to lessen costs. Dr Brown points out that this medicine could have side effects like diarrhea and vomiting. However, the study aforementioned notes that for this, only 5% patients had vomiting symptoms, when compared with Tamiflu.
Dr Brown also said that Xofluza can stop viral shedding in one day, while Tamiflu could take up to three days. "Both antivirals will help reduce the duration of misery by couple of days," she pointed out.
Dr Brown also pointed out that overall, "Xofluza is rising in popularity over Tamiflu." “One dose. Fewer side effects. More insurances are covering the cost of it now and manufacturer coupon makes it less expensive than in previous years," she said.
Rapivab: This is another prescribed medication that is approved to treat flu. This could be administered for people ages 6 months and older. It has to be given by a health care provider, as it is given once as an intravenous infusion. It could cost up to $1,000 without insurance and most common reaction in adults is diarrhea.
Relenza: This flu medication is inhaled in powder form. It is administered through an inhaler device, which is to be used twice a day for five days straight. The prescribed drug is approved to treat flu in ages 7 and older and for preventative use, in ages 5 and older. It could cost about $90 without insurance.
It may have side effects like dizziness, allergic reaction, or irritation of the nose. It is not recommended for people who have breathing issues or have asthma.
How To Cure Hangover Headache At Home?

Credits: Canva
Hangover headaches are miserable. Most people know that drinking too much alcohol can leave you with a long list of next-day problems, and a headache is one of the most common. You will find no shortage of so-called hangover headache “fixes” online, in home remedies, and even on store shelves. The problem is that very few of them are backed by solid scientific evidence. The surest way to prevent a hangover headache is to watch how much alcohol you drink at one time. That said, there are a few simple, home-based steps that may lower your risk of waking up with a headache, and some practical ways to manage the pain if it has already set in.
What Is A Hangover?
A hangover refers to the uncomfortable physical and mental effects you experience after drinking too much alcohol the night before. According to the Cleveland Clinic, hangovers are extremely common among people who overdrink. One study found that nearly 75% of people who consumed excessive alcohol reported hangover symptoms the following day. The same research suggested that about 25% to 30% of drinkers may not experience hangovers at all.
How Much Alcohol Does It Take To Get A Hangover?
Drinking more than one alcoholic beverage per hour can lead to a hangover. Your body generally needs about an hour to break down and process a single drink. As explained by the Cleveland Clinic, one drink is roughly equal to:
- One 12-ounce can of regular or light beer (5% alcohol).
- Half a pint, or about 8 to 9 ounces, of malt liquor or many craft beers (7% alcohol).
- One 5-ounce glass of table wine (12% alcohol).
- One shot, or 1.5 ounces, of liquor (40% alcohol).
How To Cure Hangover Headache At Home?
Many products and home remedies claim they can cure a hangover, but most are not supported by science, and some may even do harm. For instance, having more alcohol the next morning does not fix a hangover. It simply adds more toxins to your system.
Instead, consider these self-care measures for hangover relief:
- Eat simple foods with complex carbohydrates, such as toast or crackers. These can help raise low blood sugar levels and ease nausea.
- Drink plenty of fluids. Water, electrolyte drinks like Gatorade® or Pedialyte®, broth, and other non-alcoholic beverages can help counter dehydration. A good sign you are rehydrated is when your urine becomes clear.
- Get adequate sleep to help your body recover from fatigue.
- Use antacids to calm stomach discomfort.
Consider aspirin or other nonsteroidal anti-inflammatory drugs (NSAIDs) such as ibuprofen or naproxen to relieve aches and pains. NSAIDs are generally the most effective medications for hangover-related pain, but they should be used cautiously because they can irritate your stomach. Avoid acetaminophen (Tylenol), as combining it with alcohol can damage your liver.
Give it time. Hangover symptoms usually improve within eight to 24 hours. During this period, your body works to eliminate alcohol toxins, restore hydration, repair tissues, and return normal body functions to baseline.
© 2024 Bennett, Coleman & Company Limited

