- Health Conditions A-Z
- Health & Wellness
- Nutrition
- Fitness
- Health News
- Ayurveda
- Videos
- Medicine A-Z
- Parenting
- Web Stories
Credits: Northwestern Medicine
Breathlessness During Pregnancy? Cough Turned Out To Be Stage 3 Melanoma For This Woman; Doctors Share Details
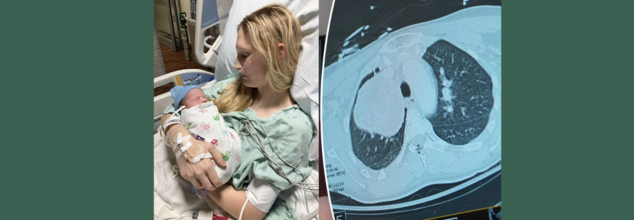
What started out as a persistent cough while pregnant almost turned into a tragedy for 26-year-old Illinois' MaKenna Lauterbach. At 36 weeks' pregnancy, the would-be mom thought that her symptoms were normal for pregnancy exhaustion in late stages—until she started gasping for air from doing minor chores. What ensued was a time-sensitive, life-saving battle of wits between world-class experts, state-of-the-art medical treatments, and an outcome against all odds.
Pregnancy tends to be accompanied by fatigue, shortness of breath, and changing physical needs. So when MaKenna began feeling breathless and having a persistent cough while caring for her horses, she attributed it to third-trimester exertion. Walking to the barn made her breathless—as if she'd run a marathon. But her symptoms did not get better, and by the time she was full term, her condition had progressed dramatically.
Even with her deteriorating symptoms, imaging tests were initially shunned. Medical staff are naturally averse to putting pregnant women through the stress of radiation exposure, particularly when in the late stages of pregnancy. But MaKenna's condition rapidly worsened—coughing gave way to vomiting and intense respiratory distress, prompting emergency admission to hospital.
Just a few days from her due date, imaging at last showed the devastating discovery—a grapefruit-sized tumor wedged in her chest, obstructing the artery to her right lung. The tumor was suffocating her airway and threateningly restricting oxygen delivery, placing mother and baby alike in danger.
MaKenna was flown to Northwestern Memorial Hospital in Chicago, where she was admitted to the intensive care unit. Within a short time after arrival, she went into labor. Her blood pressure rose, the baby became distressed, and physicians realized that they had only hours—possibly minutes—to move.
"Her lungs were impaired because of the tumor, and labor was also slowing her down to breathe. The danger of respiratory failure and cardiac arrest was very real," said Dr. Lynn Yee, a maternal-fetal medicine specialist at Northwestern Medicine.
MaKenna was put on extracorporeal life support (ECMO)—a life-supporting device that circulates oxygenated blood outside of the body—and received an emergency C-section. Her baby boy, Colter, was delivered safely, healthy in spite of the wild ride he had getting here.
For MaKenna, there was a mix of joy and fear. "Because of the tumor, the delivery came so rapidly. I was mourning the birth plan I had been planning for months, while also coping with the news of my surprise diagnosis," she explained.
What is Rare and Aggressive Melanoma?
After the birth, physicians initiated additional tests. A bronchoscopy test showed the tumor was stage 3 melanoma—a skin cancer that had somehow traveled and developed inside her chest.
This posed a singular challenge. "There isn't much written about or a lot of published cases on how to treat melanoma that comes in this way," said Dr. Kalvin Lung, a thoracic surgeon at Northwestern Medicine. "We had to fall back on the knowledge our team has gained from years of taking care of complex thoracic cases."
Prior to surgery, doctors gave three doses of immunotherapy to shrink the tumor. The therapy was effective in diminishing its size from 13 centimeters to 9 centimeters, thus enabling the subsequent action—surgery.
The procedure itself was extremely complicated. Dr. Lung and Dr. Chris Mehta, a cardiac surgeon with Northwestern Medicine, were required to remove MaKenna's right lung entirely, part of the pulmonary artery, and related lymph nodes. The tumor had invaded large blood vessels and spread throughout all three lobes of the right lung. "We may have a case like this every few years," said Dr. Mehta.
Now 27, MaKenna is stable and continues her immunotherapy treatments. Her scans show no new signs of metastatic cancer, and the tumor site remains inactive. She’s focusing on motherhood, recovery, and gratitude.
“Colter is the best baby—always smiling and sleeping through the night,” she said. “I can’t say enough about the incredible medical team that saved my life. Because of them, I’m here today.”
Dr. Yee continued, "To see MaKenna doing so well, and Colter thriving, brings tears to my eyes. It demonstrates what coordinated, compassionate medical care can do."
Can Pregnancy Shadow Life-Threatening Illnesses?
Pregnancy is commonly accompanied by a variety of physical changes—fatigue, shortness of breath, backaches, nausea, and swelling. Although these symptoms are typically harmless, they sometimes mask the signs of serious underlying medical conditions. This crossover between normal pregnancy pains and signs of potentially fatal diseases can mean that the illnesses are not diagnosed until late, as in the recent case of MaKenna Lauterbach—a 26-year-old woman whose relentless cough and shortness of breath throughout her pregnancy proved to be stage 3 melanoma in her chest.
Shared Symptoms of Pregnancy and Illness Mimic One Another
Most life-threatening conditions have symptoms that are identical to those of pregnancy. Diseases such as heart disease, blood clots, infections, and even cancer may appear with fatigue, chest pain, shortness of breath, or swelling—commonly attributed to normal pregnancy complaints. This similarity results in a diagnostic blind spot.
For example:
- Shortness of breath can be due to increased oxygen demand during pregnancy but can also result from lung disease or heart failure.
- Swelling in late pregnancy is normal but may indicate preeclampsia, kidney disease, or a tumor compressing veins.
- Nausea and vomiting are usual in the first trimester but may also obscure gastrointestinal cancers or liver disease.
Hesitation With Diagnostic Imaging in Pregnancy
One of the greatest difficulties is that physicians tend to shun some diagnostic tests such as X-rays, CT scans, or MRIs during pregnancy in order to avoid exposing the fetus to radiation. Although this prudence is necessary, it can lead to life-threatening delays if a critical condition is suspected but not diagnosed. In MaKenna's situation, imaging was delayed until her symptoms became critical—by that time, a tumor had obstructed large lung arteries.
Immune and Hormonal Alterations Can Speed Up Underlying Disorders
Pregnancy dampens some immune reactions to shield the developing fetus. Yet, this changed immune environment can give rise to or speed up latent diseases like cancer, autoimmune disorders, or infections. Hormonal spikes can also nourish hormone-sensitive tumors, elevating the risk of complications.
Fetal Over Maternal Prioritization in Emergency Situations
During emergencies, choices are frequently made to safeguard the baby—even at the expense of delaying the mother's treatment. This preference can make cases more complex when the mother's declining health impacts fetal welfare directly. Delayed diagnosis or treatment of maternal illness can put both lives at increased risk.
Emotional and Cognitive Biases
Numerous pregnant women—such as MaKenna—will minimize their symptoms, assuming they are just a result of pregnancy demands. There is also a cultural pressure to suffer through pregnancy, and this can cause women not to speak up or seek second opinions when something does not feel right.
Pregnant patients with severe medical issues frequently need treatment from several specialists: obstetricians, oncologists, cardiologists, or pulmonologists. Without an integrated and coordinated effort, important warning signs can be overlooked or insufficiently explored. MaKenna's survival was partly because of the rapid collaboration between maternal-fetal medicine, thoracic surgery, oncology, and intensive care specialists.
Pregnancy never needs to stand in the way of diagnosing and treating potentially life-threatening diseases. Awareness, early investigation, and multidisciplinary care are critical in distinguishing normal pregnancy symptoms from red flags. Pregnant women must always feel confident enough to voice their concerns, clarify the situation, and stand up for their well-being—because, as MaKenna's experience demonstrates, an early diagnosis can save not just one, but two lives.

Credit: Canva
What Happens When You Apply Raw Apple On Your Face?
Honey, oats, curd, berries...no I am not talking about foods to eat but things people apply on their face to keep to glowing and fighting anti-ageing. But there is one fruit that is less talked about when it comes to skincare-Apple. But why is Apple gaining popularity in skincare?
Several potential benefits come from applying apple-based products to the skin, including:
Prevents Premature Skin Ageing
Many skincare brands now use apple extract in their formulations.
As per dermatologists, highlight that apple extract contains phenolic acids and flavonoids, two essential components commonly found in fruits. A 2019 study emphasised the role of phenolic acids in a balanced diet, attributing their powerful antioxidant properties to various health benefits. Additionally, a 2016 review noted that flavonoids possess antioxidant, anti-inflammatory, antimutagenic, and anticarcinogenic properties.
Many anti-ageing skincare products also feature these compounds. As a 2019 study demonstrated, both phenolic acids and flavonoids help shield the skin from pollution-related damage. Apple fruit extract is a valuable skincare ingredient due to its rich composition of phytochemicals. Flavonoids act as antioxidants, protecting the skin from free radical damage caused by UV exposure, pollution, and environmental stressors.
Apple fruit extract contains flavonoids such as:
Catechins
Flavanols
Quercetin
May Give a Dewy Glow
Some believe that applying apple cider vinegar to the skin can improve dullness. Apple cider vinegar, derived from apples, contains acetic acid and citric acid.
A 2021 study found that acetic acid has antioxidant properties that protect the skin from infections. However, improper usage can cause skin irritation.
Citric acid, an alpha hydroxy acid (AHA), acts as an exfoliant. A 2018 study suggested that citric acid can help remove dull outer layers of skin, revealing a fresher, more radiant complexion.
Joyce Carslaw, founder of SmartAss Beauty, explains, “Unlike physical exfoliants with scrubbing particles, apple fruit water gently exfoliates dead skin without breaking the proteins that hold skin cells together.”
May Help Reduce Acne
Apples may also aid in acne management.
A 2018 study indicated that citric acid in apple cider vinegar can help reduce acne-related inflammation. However, excessive use may harm the skin barrier. Apple fruit extract (Pyrus malus) is an excellent addition to skincare formulations. It contains vitamins A and C, as well as zinc—compounds known to support clear, healthy skin.
Keeps Skin Hydrated
Apples are rich in vitamin E, a crucial nutrient for skin hydration. Older studies from 1998 and 2006 revealed that apple has water-binding properties that help maintain skin moisture and nourishment.
Using Apples in DIY Skincare
Expert dermatologists widely acknowledge the skincare benefits of apples and apple fruit extract when properly formulated.”
Shafer suggests applying apple slices directly to the face for a quick hydration boost. The vitamin E in apples helps keep the skin soft and hydrated, while the juice firms up the skin and maintains its natural pH balance.
For acne-prone skin, try mashed apple mixed with heavy cream or coconut milk. Mashed apple combined with milk cream soothes acne. Regular application can help fade dark spots and prevent future breakouts.

Credits: Canva
Is There A Limit To How Far Female Fertility Can Be Extended?
Over the past century, social progress has greatly altered the age at which women opt to have children. Whereas most women in the past gave birth in their early twenties or teens, the trend has since dramatically changed. Women in nations such as the U.S., South Korea, and in Europe are now delaying motherhood to well into their 30s. Indeed, the average age of first-time mothers in most OECD countries now stands at about 30.
But biology has not kept pace with society. Women's fertility is still tied to the natural aging of a woman's reproductive apparatus – something that modern medicine is always trying to get around. With career aspirations, education, and individual choice rewriting the schedules of motherhood, an urgent question presents itself: how far can we push back female fertility?
How Does The Biological Clock Work?
At the very center of female fertility is a game of numbers – one that is decided even before a girl is born. Women are born with a limited number of eggs, usually one million. By the time they reach puberty, this count drops to about 300,000. Of these, only some 300 to 400 will ever develop and get released during ovulation.
By age 37, egg stores decrease to around 25,000, and by age 51 – the average age of menopause in the United States – only 1,000 are left. Yet, ovulation and fertility do not necessarily persist up to menopause. In the majority of women, natural fertility declines sharply 7 to 10 years before, typically by the early 40s.
Though this fall has been around for some time, its raw statistics still stun: natural conception chances fall from about 25% per cycle during a woman's 20s to less than 5% per cycle by her 40s.
What Does the Egg Supply Do at Each Age?
More important than the declining egg quantity is the sharp decline in egg quality with advancing age. Each egg contains chromosomes that make up the DNA map for a new life. When egg quality falls, so does the chance for a successful pregnancy.
By age 30, nearly 25–30% of a woman’s eggs may carry chromosomal abnormalities. By 35, this rises to 40%, and after 40, it spikes dramatically. Studies show that beyond age 40, up to 75% of eggs may have abnormalities. Such eggs are less likely to fertilize, implant, or lead to a healthy baby.
The dangers posed by low quality of eggs are miscarriage, unsuccessful fertility treatment, and chromosomal abnormalities such as Down syndrome.
How Far Can Science Go in Extending Fertility?
With the help of improvements in assisted reproductive technologies (ART), the limits of biological fertility are gradually being extended. Methods like egg freezing (oocyte cryopreservation), in vitro fertilization (IVF), and the employment of donor eggs have helped many women give birth well into their 40s – and, in some instances, even their 50s.
Egg freezing, specifically, has been a game-changer. It enables women to save their younger, healthier eggs to use later in life. It's not a surefire insurance policy, though. Success is dependent on age at the time of freezing, number of eggs saved, and overall health.
Nevertheless, though technology may provide additional time, it will not halt the natural aging of the ovaries or enhance the genetic quality of aging eggs. There is still a biological limit.
Decrease in Male Fertility Level
Men, too, experience a decline in fertility – but it tends to occur more gradually. Starting around age 40 to 45, men see a drop in sperm quality and volume, but they often retain the ability to father children into their 60s and beyond. Unlike women, men continuously produce new sperm, whereas women are working from a non-renewable stockpile of eggs.
This disparity implies that while more and more couples are opting to wait to have children, the responsibility of the "biological clock" remains mostly on women.
Although most of the discussion about female reproductive aging centers on wanting to have children, it is important to note that it also marks more general changes in a woman's health – specifically the onset of menopause and its attendant risks. Perhaps one of the most important but most underappreciated is the increasing significance of regular reproductive screenings, particularly as women get older.
Among these, cervical cancer screening stands out as a powerful tool to protect women’s health beyond their childbearing years.
Pap smears and HPV testing are able to pick up on abnormal cell changes before they develop into cancer. Because the immune system shifts with age and hormonal changes impact cervical health, regular screening is even more important. Women in their 30s and 40s – the same time frame when fertility is actively shifting – need to continue to be vigilant about their yearly OB-GYN checkups.
Actually, while women are thinking of or undergoing fertility treatments or assessing their reproductive future, this is the ideal opportunity to make sure their cervical health is under surveillance. New technologies in at-home HPV testing, liquid-based cytology, and co-testing provide more convenient and precise diagnoses ever before.
So is there a boundary beyond which female fertility can be prolonged? Biologically, yes. Despite incredible scientific strides, the natural aging of eggs and of the ovaries places limits that technology can only stretch so far.
Yet reproductive health is more than fertility. By broadening the story to encompass cervical screenings and preventive care, we give women the ability to take holistic control of their reproductive path – whether they opt to become mothers at 25, 35, or older because prolonging fertility isn't merely about having the capacity to conceive, it's about maintaining a lifetime of reproductive health.

Credits: Collect/PA Real Life
31-Year-Old Woman Dies From Dementia After Critical Early Signs Were Missed; How Prevent Early Memory Decline
Gemma Illingworth was only 31 when she died from a rare and aggressive type of dementia. A bright, independent artist who painted, traveled the world, and valued life's creative liberties, Gemma's life is not only tragic — it's a valuable lesson in the crucial need to recognize subtle neurological symptoms early on. Diagnosed at 28 with posterior cortical atrophy (PCA), a rare dementia that attacks the brain's visual processing area, Gemma's condition worsened quickly.
Her premature death highlights an increasing public health issue: overlooked early warning signs of cognitive and neurodegenerative impairment. For policymakers, healthcare professionals, and family members, her tale is both a warning and a reminder.
What is Posterior Cortical Atrophy?
Posterior Cortical Atrophy (PCA) is a rare, progressive neurodegenerative illness usually regarded as a subtype of Alzheimer's disease. In contrast to normal Alzheimer's, which first compromises memory, PCA attacks the rear portion of the brain — the occipital and parietal lobes — that are involved in visual and spatial processing. Some of the symptoms are:
- Trouble reading, identifying objects, or estimating distances
- Visual confusion or disorientation
- Hand-eye coordination difficulties
- Trouble with daily visual activities
Because of its atypical presentation, PCA often goes misdiagnosed as depression, anxiety, or even ophthalmological issues. This diagnostic challenge delayed Gemma’s care for years, despite her early struggles with sight, time perception, and coordination — red flags that now, in hindsight, point clearly to the disease’s onset.
The Missed Signs of Early-Onset Alzheimer's
Gemma's family recalls her as "ditsy," a girl who was unusual but self-reliant. From an early age, she had difficulty with her eyesight, telling the time, and coordination. Her difficulties were attributed to her character and not taken as possible signs of a neurological disorder.
It was not until 2020, during the COVID-19 lockdown, that her condition progressed quickly. She was no longer able to process visual information on her computer screen, and she had to cease working. Her symptoms were first blamed on anxiety and depression. It was not until thorough neurological testing in 2021 that PCA was diagnosed. By this time, the disease had progressed significantly.
This delay in diagnosis had a devastating impact — and it serves as a powerful reminder that even subtle neurological symptoms should not be ignored or dismissed.
Once diagnosed, Gemma's ability to live independently quickly declined. She began needing help with basic tasks: dressing, using the stove, managing appointments. She would call her mother up to 20 times a day. Eventually, she returned home, requiring full-time care.
Her sister Jess remembered, "She didn't know what [PCA] really meant, but that was obviously a blessing in disguise." Even with the dire prognosis, Gemma was relieved at first, believing she could now "fix" whatever was amiss.
But there was no cure. Her illness affected her ability to eat, swallow, talk, and walk. Her family took care of her at home until she died in November 2023, surrounded by loved ones. Her sense of humor, they reported, never left her — one of the few things the disease couldn't steal.
In Gemma's memory, her best friend and siblings completed the 2024 London Marathon, raising more than $47,000 for the National Brain Appeal and Rare Dementia Support (RDS).
"RDS couldn't cure Gemma, but they supported us through it the best way possible," her brother Ben explained. Their aim now is not to let other families endure the same suffering.
The funds raised support research, education, and family care for those with rare dementias — a community frequently ignored in popular discussions of memory decline and aging.
Why Early Detection is Important?
Dementia is commonly regarded as an old person's disease. Gemma's experience shatters the stereotype. Although PCA is uncommon, dementias in younger people are increasingly being diagnosed by neurologists globally.
Cognitive decline does not necessarily begin with memory loss. It may begin subtly — in the guise of visual problems, coordination problems, repeated disorientation, or even mood swings. That's why it's important that clinicians, educators, and families realize early symptoms can be disguised as behavioral idiosyncrasies or psychological problems. Early diagnosis can:
Give time for appropriate care planning and lifestyle changes
Halt progression with cognitive therapies or medications (where indicated)
Provide emotional relief and clarity for patients and families
How to Recognize and Prevent Early Memory Decline?
Although prevention of dementia is not always possible, early identification can dramatically enhance quality of life. Following are the preventive steps anyone can take:
1. Be Alert to Atypical Symptoms
Observe sudden or progressive change in visual-spatial awareness, particularly in young adults. Difficulty judging distances, recognizing objects, or maneuvering in familiar spaces may require neurological assessment.
2. Prioritize Complete Health Evaluations
When symptoms occur, push for full testing. This should involve neuroimaging (MRI or CT), cognitive screening, and — if necessary — spinal fluid analysis.
3. Get Early Intervention
Work with experts like neuropsychologists, neurologists, and occupational therapists early on. They can offer tools and coping strategies to deal with daily activities.
4. Emphasize Brain Health
A diet high in antioxidants (berries, greens), exercise, mental stimulation, and adequate sleep all help improve brain function and lower the risk of cognitive impairment.
5. Know Your Family History
Certain dementias are linked to genetics. If family history exists, don't wait on neurological evaluation if symptoms develop.
© 2024 Bennett, Coleman & Company Limited

