- Health Conditions A-Z
- Health & Wellness
- Nutrition
- Fitness
- Health News
- Ayurveda
- Videos
- Medicine A-Z
- Parenting
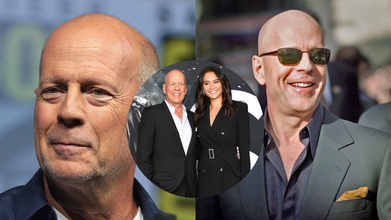
Bruce Willis’ Dementia Diagnosis Left Wife Emma Heming Feeling ‘Lost’ And ‘Isolated’ - What Are The Signs Of Caregivers Burnout?

In 2022, beloved actor Bruce Willis was diagnosed with frontotemporal dementia, a heartbreaking turn that deeply impacted not only him but his whole family. Although the news left fans around the world in shock, it was actually his wife, Emma Heming Willis, who carried the emotional brunt of the diagnosis in the moment. At the Women's Alzheimer's Movement Forum in Las Vegas last month, Emma spoke for the first time about the emotional damage done by that experience and the unseen toll of caregiving—one that millions of people worldwide quietly experience daily.
Emma Heming Willis recalled the day Bruce was formally diagnosed with dementia as one that made her feel "lost, isolated and afraid."
"On the day Bruce got his diagnosis, we walked out of the doctor's office with a pamphlet and an empty goodbye. No plan, no guidance, no hope, just shock," she explained in front of a packed auditorium, People reported.
In one instant, the family's future disappeared. The Oscar-winning actor, famous for his quick wit and performances in Die Hard and The Sixth Sense, would be leaving his career behind. Emma found herself thrust into a whole new role of full-time caregiver at the same time.
She continued to explain, "I found myself having to keep my family intact, raise our two small girls, and tend to the man that I love while dealing with an illness I hardly knew anything about."
Emma's emotional candor resonated with hundreds of families who have received similar diagnoses and encouraged her to author a book, The Unexpected Journey, scheduled for publication in September. In Emma's words, "This is the book I hope will assist the next caregiver. It is packed with encouragement, wisdom, and the encouragement necessary to walk this path.
Frontotemporal dementia is a less prevalent type of dementia that mainly occurs in the frontal and temporal lobes of the brain. It tends to affect behavior, personality, language, and movement more than memory, particularly in its initial stages.
In contrast to Alzheimer's, which generally strikes older individuals, FTD can hit at an earlier age—sometimes as young as 40. The symptoms can range from changes in personality, emotional flatness, or the inability to show empathy to impulsiveness, so it is especially hard for spouses and children to cope.
Emma's case illustrates how abrupt and disrupting this diagnosis can be—not only for the patient but for caregivers as well.
Whereas Bruce Willis' diagnosis hit global headlines, the mental toll taken by Emma, his caregiver, was largely in the background—until she decided to come forward.
Caregiving is a respectable position, but it's also a challenging and thankless one. For those who are caring for loved ones with dementia or other chronic illnesses, the stress of "keeping it all together" can result in a condition called caregiver burnout.
"Caring for someone is the most intimate and demanding work of love," Emma explained, "but when you're not noticed or supported, it begins to undermine your health—mentally and physically."
What Is Caregiver Burnout?
Caregiver burnout is a condition of emotional, physical, and mental weariness resulting from long-term and excessive caregiving demands. It tends to lead to feelings of hopelessness, loneliness, and guilt—and is worsened when caregivers fail to prioritize their own health and well-being.
In the United States alone, over 53 million individuals act as unpaid caregivers, reports the National Alliance for Caregiving. While they bear a massive burden, too many of them are without access to support structures or mental health resources.
Signs Of Caregiver Burnout
If you are caring for a loved one—particularly someone with a degenerative condition such as dementia—it's important to look for these early warning signs of burnout:
Chronic fatigue: Being physically and emotionally drained, even after rest or sleep.
Lack of interest in hobbies: Avoiding activities and passions you used to enjoy.
Social withdrawal: Steering clear of friends and family out of exhaustion or feelings of being overwhelmed.
Increased irritability: Becoming angry or resentful with the person you're caring for, or blowing up over trivial inconveniences.
Illness: Persistent headaches, gastrointestinal problems, weakened immune system, or getting chronic illnesses.
Sleep disturbances: Waking up often, insomnia, or sleeping too much.
Emotional numbing or persistent crying: Feeling of being trapped without relief in sight, along with emotional numbing or excessive crying.
Why Addressing Burnout Is Important?
Caregiver burnout isn't just hard on the caregiver—it's also destructive to the quality of care received. Burned out and frazzled, it becomes more difficult to bring compassion, patience, and focus to caring for someone with intricate needs.
If left unaddressed, burnout can create depression, anxiety disorders, and even physical breakdown, which is why it is so important to get help before getting to a point of crisis.
Emma Heming Willis's openness to talk about her own challenges brings light to a larger social problem: the invisibility and unavailability of caregiver resources.
Her work strives to make discussion of caregiver mental health common and give others the tools she wishes someone had given her when Bruce was initially diagnosed. "What I needed that day wasn't a pamphlet," she said to the crowd. "I needed someone to look me in the eye and tell me, 'This feels impossible right now, but you will find your footing.'"
Steps to Prevent and Manage Burnout
To assist in preventing or coping with caregiver burnout, professionals suggest:
Pursuing professional help: Counseling or therapy can be a lifesaver.
Regular breaks: Respite care programs or a reliable family member can take over.
Support groups: Talking with others who experience the same situation can soften the sense of loneliness.
Taking care of your own health: Healthy meals, exercise, and routine check-ups.
Establishing boundaries: Saying no is acceptable, and asking for assistance is okay.
As the global population ages and the prevalence of neurodegenerative diseases grows, it’s more important than ever to champion and protect those who give so selflessly.
Caregiving can start as a labor of love—but it needs to be valued, respected, and maintained by community, healthcare systems, and society as a whole.
Bruce Willis’ Wife Emma Says He Is Unaware of His Dementia Diagnosis
Credits: Wikimedia Commons
Bruce Willis was diagnosed with frontotemporal dementia in 2022. His wife, Emma Heming Willis recalled the day when Bruce was diagnosed with the condition and how it made her feel "lost, isolated and afraid." Talkin to PEOPLE, Emma said, Bruce "never connected the dots" that he has been diagnosed with frontotemporal dementia. “I think that's like the blessing and the curse of this, is that he never connected the dots that he had this disease, and I'm really happy about that. I'm really happy that he doesn't know about it,” she shared about Bruce, 70.
Bruce Willis' Diagnosis
"On the day Bruce got his diagnosis, we walked out of the doctor's office with a pamphlet and an empty goodbye. No plan, no guidance, no hope, just shock," she explained in front of a packed auditorium, People reported.
In one instant, the family's future disappeared. The Oscar-winning actor, famous for his quick wit and performances in Die Hard and The Sixth Sense, would be leaving his career behind. Emma found herself thrust into a whole new role of full-time caregiver at the same time.
She continued to explain, "I found myself having to keep my family intact, raise our two small girls, and tend to the man that I love while dealing with an illness I hardly knew anything about."
Emma's emotional candor resonated with hundreds of families who have received similar diagnoses and encouraged her to author a book, The Unexpected Journey, scheduled for publication in September. In Emma's words, "This is the book I hope will assist the next caregiver. It is packed with encouragement, wisdom, and the encouragement necessary to walk this path.
What Is Frontotemporal Dementia?
Frontotemporal dementia is a less prevalent type of dementia that mainly occurs in the frontal and temporal lobes of the brain. It tends to affect behavior, personality, language, and movement more than memory, particularly in its initial stages.
In contrast to Alzheimer's, which generally strikes older individuals, FTD can hit at an earlier age—sometimes as young as 40. The symptoms can range from changes in personality, emotional flatness, or the inability to show empathy to impulsiveness, so it is especially hard for spouses and children to cope.
Emma's case illustrates how abrupt and disrupting this diagnosis can be—not only for the patient but for caregivers as well.
Whereas Bruce Willis' diagnosis hit global headlines, the mental toll taken by Emma, his caregiver, was largely in the background—until she decided to come forward.
Caregiving is a respectable position, but it's also a challenging and thankless one. For those who are caring for loved ones with dementia or other chronic illnesses, the stress of "keeping it all together" can result in a condition called caregiver burnout.
"Caring for someone is the most intimate and demanding work of love," Emma explained, "but when you're not noticed or supported, it begins to undermine your health—mentally and physically."
‘Work Stress Makes You Gay’: Why Malaysian Minister's Remark Proves The Need To Understand Sex, Gender And Sexuality

Credits: X and Canva
Work stress could make you gay, said a Malaysian minister Zulkifli Hasan, as continued government intervention of what is described as 'sexually deviant behavior' has pressured the country's LGBTQ community. This happened two weeks after religious authorities and police acted on complaints from a sultan and Islamist politicians that a camping retreat was promoting the LGBTQ lifestyle, reported South China Morning Post.
Religious Affairs Minister Hasan on Tuesday said that work stress could be among many other factors that is pushing people into sexual orientations other than heterosexuality. “Societal influence, sexual experiences, work stress and other personal factors come under this category [of possible causes],” Zulkifli said in a written parliamentary reply to a question by Siti Zailah Mohd Yusoff, a lawmaker with the opposition Islamist party PAS.
Also Read: Andy Kershaw Diagnosed With Spinal Cancer That Left Him Unable To Walk
He cited a 2017 study by Sulaiman et.al., that said such elements "can contribute to the increase in LGBT acts".
His comments have attracted a lot of backlash, with many people on social media mocking him. A social media user Muaz Zam said, "By this logic, I am genuinely shocked my entire office isn't gay by now". Another one read: "In other words: they never work hard in the parliament."
However, these claims are not scientifically back. Work related stress can impact a person, but cannot change their sexuality. It can, however, cause health effects. What it does not do is change one's sexuality and this is why one should know the difference about gender, sex and sexual orientation or sexuality.
'Work Stress Makes You Gay': The Difference Between Gender vs Sex

While these both terms are often used interchangeably in official forms, there is a difference between the two.
As per the Council of Europe, gender is an area that cuts across thinking about society, law, politics, and culture.
Read: Trump Administration Deadnames Transgender Former HHS Officer Rachel Levine in Official Portrait
Definition Of Gender vs Sex by WHO
The World Health Organization notes that sex refers to: "the different biological and physiological characteristics of males and females, such as reproductive organs, chromosomes, hormones, etc.”
Whereas, gender refers to: "the socially constructed characteristics of women and men – such as norms, roles and relationships of and between groups of women and men. It varies from society to society and can be changed. The concept of gender includes five important elements: relational, hierarchical, historical, contextual and institutional. While most people are born either male or female, they are taught appropriate norms and behaviours – including how they should interact with others of the same or opposite sex within households, communities and work places. When individuals or groups do not “fit” established gender norms they often face stigma, discriminatory practices or social exclusion – all of which adversely affect health."
Definition Of Gender vs Sex by The European Institute For Gender Equality
“Sex refers to the biological and physiological characteristics that define humans as female or male. These sets of biological characteristics are not mutually exclusive, as there are individuals who possess both, but these characteristics tend to differentiate humans as females or males.”
“Gender refers to the social attributes and opportunities associated with being female and male and to the relationships between women and men and girls and boys, as well as to the relations between women and those between men. These attributes, opportunities and relationships are socially constructed and are learned through socialisation processes. They are context- and time-specific, and changeable. Gender determines what is expected, allowed and valued in a woman or a man in a given context. In most societies, there are differences and inequalities between women and men in responsibilities assigned, activities undertaken, access to and control over resources, as well as decision-making opportunities. Gender is part of the broader sociocultural context. Other important criteria for sociocultural analysis include class, race, poverty level, ethnic group and age.”
The main difference is that gender is a social construct, whereas sex is the biologically labelled term based on organs and hormones.
Read More: Trump's Top Health Nominee Wants ‘Corrective Care’ For Trans People
What Is Sexuality?

As per the American Psychological Association (APA), sexuality is the capacity to derive pleasure from various forms of sexual activity and behavior. The Lanarkshire Sexual Health describes sexual orientation as a way to describe the feelings you have for someone you fancy or are attached to.
While sexuality can change overtime, it is not a choice. There is no evidence that sexual orientation can be forced to change through therapy.
Can Stress Impact Sexuality?
While stress can impact sexual function by reducing libido, causing fatigue, and triggering hormonal changes, it does not change one's sexual orientation. Jason Teoh, who writes on LGBTQ issues, project partner at NSW Department of Planning, Housing and Infrastructure, notes: "Sexual orientation is not caused by stress. It is not caused by trauma, influence or difficult life circumstances."
The WHO notes: sexual orientation is a natural, stable part of human identity shaped by biology, genetics, and early development. The WHO removed homosexuality from its disease classification in 1990. The American Psychiatric Association did the same in 1973.
The 4 Parkinson's Signs That Appear Years Before Diagnosis

Credit: Canva
Parkinson's disease is a progressive, neurodegenerative movement disorder caused by the loss of dopamine-producing brain cells, primarily affecting people over 60. Apart from motor loss, the disease also causes cognitive decline, depression, anxiety and swallowing problems.
The first symptom may be a barely noticeable tremor in just one hand or sometimes a foot or the jaw. Over time, swinging your arms may become difficult and your speech may become soft or slurred. The disorder also causes stiffness, slowing of movement and trouble with balance that raises the risk of falls.
However, before clear symptoms begin to appear, Neurologist Rachel Dolhun says certain signs may help identify the onset of the disease decades before it is diagnosed.
“It’s important to stress that not everyone who has these symptoms goes on to develop Parkinson’s,” said neurologist Rachel Dolhun. “But we know that in some people, these can be some of the earliest signs," she told The Washington Post.
Here is what you should look out for:
1. Loss Of Smell
Loss of smell, or hyposmia, is a common and early non-motor symptom of Parkinson's disease, affecting up to 90 percent of patients. This symptom can significantly impact quality of life by reducing the enjoyment of food and diminishing appetite.
While strongly linked to Parkinson's, smell loss can also stem from other causes, including sinus problems, COVID-19, or aging.
2. Acting Out Dreams
Acting out dreams, known as REM Sleep Behavior Disorder (RBD), involves physically enacting vivid, often unpleasant dreams through shouting, punching, or kicking during sleep.
This typically happens because the brainstem fails to temporarily paralyze muscles during REM sleep. It is a strong early warning sign of Parkinson's disease, often appearing years or decades before motor symptoms. About 50 percent of people with Parkinson's experience RBD.
READ MORE: Parkinson’s Patients May Soon Walk Better With This New Personalized Brain Therapy
3. Constipation
Constipation is a very common and significant non-motor symptom of Parkinson's disease that is caused by nerve changes slowing gut muscles and potentially exacerbated by low activity and dehydration.
Constipation can also be caused by Parkinson's medications such as anticholinergics, amantadine and other common drugs such as opioids, iron/calcium antacids.
4. Dizziness As You Stand
The autonomic nervous system fails to properly constrict blood vessels or increase heart rate upon standing, often due to a lack of norepinephrine. This causes the autonomic nervous system to fail in regulating blood pressure. Over time, this leads to Neurogenic Orthostatic Hypotension.
Beyond dizziness, symptoms include blurred vision, weakness, fatigue, cognitive "fog," and "coat hanger pain" (pain in the neck/shoulders). Often times, patients experience dizziness in the morning or immediately after meals.
Diagnosing Parkinson’s disease is mostly a clinical process, meaning it relies heavily on a healthcare provider examining your symptoms, asking questions and reviewing your medical history. Various imaging and diagnostic tests used to detect disease includes CT scan, PET scan, MRI scan and genetic testing.
© 2024 Bennett, Coleman & Company Limited

