- Health Conditions A-Z
- Health & Wellness
- Nutrition
- Fitness
- Health News
- Ayurveda
- Videos
- Medicine A-Z
- Parenting
Can Ricinoleic Acid in Castor Oil Help Reduce Arthritis Pain and Inflammation?

If you grew up in an Indian household, your grandparents must have handed you a spoonful of castor oil for just about everything. It was their cure-all. Turns out, they were not entirely wrong, at least when it comes to joint pain. Castor oil contains a compound called ricinoleic acid that is now being looked at for its potential to ease arthritis-related pain and inflammation. With more people turning to gentler, natural options alongside standard treatment, this old remedy is quietly making a comeback.
What exactly is ricinoleic acid?
Ricinoleic acid is a monounsaturated omega-9 fatty acid. It makes up around 90 per cent of castor oil’s composition and has been shown to have anti-inflammatory, analgesic, and antioxidant properties. In simple terms, it can help reduce swelling, ease pain, and possibly shield tissues from further damage.
Why do people rub oil on sore joints?
Topical use of castor oil is not new. Ayurvedic and folk traditions have long endorsed it for joint stiffness, swollen knees, and general aches. The practice usually involves warming the oil slightly, applying it generously over the affected area, and covering it with a warm cloth or compress.
Heat improves circulation and opens up pores, which may help the ricinoleic acid penetrate deeper into the skin. Once inside, it is believed to interact with the body’s prostaglandin system, the same compounds that trigger inflammation and pain during arthritis flares.
What does science say?
Small animal studies have shown that ricinoleic acid can reduce swelling and pain in rodents with inflamed paws and joints.
Human evidence is still a bit thin but not non-existent. A few small clinical trials suggest that castor oil packs may help reduce arthritis symptoms when used regularly. Reportedly, patients with knee osteoarthritis who used castor oil packs reported reduced pain and stiffness after four weeks. However, the sample size was small, and the study was not double-blind.
Is it worth trying?
If you are someone who is dealing with arthritis and over-the-counter painkillers are not helping you, castor oil could be a gentle, low-risk addition to your routine. However, it is worth noting that it is not going to reverse joint damage or magically un-stiffen your limbs overnight. What it might do is reduce the pain, especially if used regularly with warm compresses and gentle massage.
Tips for trying castor oil at home:
- Buy cold-pressed, hexane-free castor oil. You want the pure stuff, not a chemical soup.
- Warm it slightly before applying. Use a hot water bottle or towel over the area for 20–30 minutes.
- Do a patch test before full use, especially if you have sensitive skin.
- Be consistent. Try it a few times a week for at least a month.
- Avoid broken skin or open wounds, since oil can trap bacteria.
40s Bring Lots Of Changes, Says Doctor, Take Care Of Your Bone, Joint And Urinary Health

Credits: Canva
Crossing 40 often brings subtle but noticeable changes in how your body feels and functions. Many people brush off early signs like morning stiffness, reduced flexibility, or frequent bathroom visits, not realizing these are part of natural age-related changes. These shifts primarily affect the bones, joints, and urinary system, areas that quietly define everyday comfort.
According to Dr. Aashish Chaudhry, Managing Director & Head, Orthopedics & Joint Replacement, Aakash Healthcare, these changes are expected but shouldn’t be ignored. “After 40, the body’s regenerative capacity slows down, particularly in bones and joints. Being aware of these changes helps in early prevention and better long-term outcomes,” he says.
Bone Health: Slower Regeneration and Higher Risk of Fractures
Bone density gradually declines with age due to hormonal changes. Women experience a drop in estrogen, and men see reduced testosterone levels—both crucial for supporting bone formation.
“Lower hormone levels weaken the natural bone-building cycle,” explains Dr. Chaudhry. “This increases the risk of fractures and even slows down healing when injuries occur.”
Key concerns include:
- Reduced bone density
- Higher risk of osteoporosis
- Slower fracture recovery
To counter this, weight-bearing exercises and strength training are crucial. A diet rich in calcium, vitamin D, and protein supports bone metabolism and maintains strength.
Joint Health: Wear, Tear, and Early Stiffness
Years of repetitive movements, combined with declining collagen production, make joints more vulnerable. Cartilage becomes less elastic, leading to stiffness, reduced mobility, and the early onset of osteoarthritis.
“Many people notice joint pain but assume it's just fatigue,” says Dr. Chaudhry. “In reality, early joint wear can be detected and managed much earlier with the right interventions.”
What contributes to joint discomfort after 40?
- Natural wear and tear
- Reduced cartilage elasticity
- Slower lubrication of joint spaces
- Early degenerative changes
Flexibility-focused exercises like yoga or stretching, along with anti-inflammatory foods such as leafy greens, berries, nuts, and omega-3 sources, can ease stiffness and protect long-term mobility.
Urinary Changes: More Common Than You Think
While both men and women experience changes in urinary patterns, men often notice symptoms more prominently due to prostate enlargement. A bigger prostate narrows the urinary passage, causing:
- Frequent urination
- Weak urinary stream
- Urgency or incomplete emptying
- Night-time urination
Women, on the other hand, may struggle with pelvic floor weakness, leading to leakage or urgency.
Dr. Chaudhry notes, “These symptoms are common after 40, but they shouldn’t be normalized. Early evaluation can prevent chronic discomfort.”
Hydration remains essential. Cutting back on caffeine, alcohol, and salty foods can also lighten urinary symptoms and prevent kidney irritation.
Lifestyle Adaptations That Make a Real Difference
Shifting from reactive to preventive care is key after 40. The goal isn’t to stop ageing—it's to age comfortably and confidently.
What helps:
- Strength and mobility exercises
- Pelvic floor training
- Maintaining a healthy weight
- Regular health screenings (bone density, kidney tests, prostate evaluation)
- Stress management through yoga, meditation, or deep breathing
- Consistent sleep routines to support tissue repair
“Think of this stage as preparing your body for the next decades,” says Dr. Chaudhry. “With the right lifestyle adjustments, most people can maintain excellent mobility and function well into older age.”
Leaked FDA Memo Sparks Fierce Debate Over Rare Vaccine-Linked Child Deaths

Credits: Canva
After the Thanksgiving, on Friday, the Food and Drug Administration (FDA)'s top vaccine regulator, Vinay Prasad made a clam that shocked the public-health established. "For the first time, the US FDA will acknowledge that COVID-19 vaccines have killed American children," he wrote in a leaked email to his staff, as reported by The Atlantic and The Washington Post.
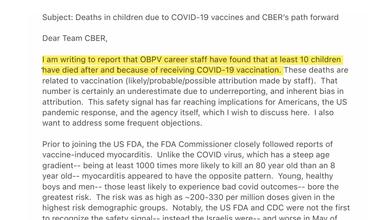
The agency has identified that at least 10 children died after getting COVID shots.
The email has been perceived by physicians as a "threat". A response from 12 former FDA commissioners, published in The New England Journal of Medicine on Wednesday, called Prasad's memo "a threat to evidence-based vaccine policy and public health security". All of the potential vaccine related deaths reported to government were already reviewed by the agency's staff, and had reached "different conclusions", wrote the former commissioners.
Elsewhere, doctors and scientists have declared that there are no evidence that links COVID-19 vaccines to deaths in children. The commissioners have claimed that in an attempt to deliberately bring evidence, Prasad and his colleagues had engaged in an "evidence-manufacturing mission", a "dumpster dive" for shoddy data, or worse, a campaign of lying.
Prasad is one of several public health officials who, under Robert F. Kennedy Jr.’s leadership, have been steadily chipping away at public trust in vaccines. So far, he has not provided evidence to back his claims, and his estimate of vaccine-related deaths may be exaggerated. The memo’s intense language and focus on political complaints also cast doubt on his assertions.
However, something that cannot be ignored is that fact that his memo may have provoked people to deny even the possibility of COVID-vaccine-related deaths. The Atlantic notes that "the idea that mRNA-based shots have, tragically, killed a very small number of children is not far-fetched." The article written by Benjamin Mazer, a physician who specializes in pathology and laboratory, notes that the this does not imply a "catastrophic threat to public health" as tens of millions of doses of the same vaccines have saved young people.
Understanding the Debate Of Vaccine-Linked Deaths
Public-health experts agree that COVID vaccines, like all medical treatments, can cause side effects. Myocarditis, a rare heart inflammation seen mostly in adolescent boys and young men after mRNA shots, remains the most discussed risk. Although usually mild and far less severe than virus-induced myocarditis, a few deaths have been documented worldwide, including isolated cases in the U.S., South Korea, and two American teenagers described in a peer-reviewed report.
These findings fuel ongoing debate about whether extremely rare vaccine-related deaths are being overlooked. Some scientists, including Paul Offit and Michael Osterholm, say the evidence does not prove the vaccines caused these deaths, noting that population-level studies show no rise in mortality after vaccination. Others argue that well-investigated autopsy-confirmed cases should be taken seriously rather than dismissed outright.
Experts such as Krutika Kuppalli, as cited by Mazer, emphasize that even if deaths occur, they are so uncommon they do not appear statistically, while the benefits, significantly reduced COVID mortality, are unmistakable. However, individual cases still raise questions on health authorities and the stricter standards of proofs they have applied when vaccines were involved to create a room for skepticism.
The concern is that rare side effects of vaccines could go undiscovered and not that vaccinations are inherently harmful.
This ONE Key Symptom Will Help You Differentiate Flu From COVID, According To Doctor

Credits: iStock
Are you down with fever? Are your symptoms also a little less common from an ordinary cold? Are you also confused between flu and COVID? Then knowing this one symptom could help you set flu apart from COVID. Dr Rupa Parmar, a GP and medical director at Midland Health tells The Mirror, that shortness of breath could be a key symptom that could differentiate between the two.
Dr Parmar highlights that it is a key indicator for COVID. "Shortness of breath is rare in both a cold and the flu, but as COVID more so affects the lungs due to inflammation, it is a common symptom."
The NHS website supports her advice, noting that breathlessness is a symptom more often tied to Covid, not the flu or a common cold. This kind of breathing difficulty is usually associated with infections like Covid or respiratory syncytial virus (RSV).
What Else Could Help You Know If You Have A COVID or Flu?
The nature of your cough could also help you understand different ailments. Dr Parmar said that a cold would produce a mild cough, whereas a flu cough could be more dry. However, with covid, "a cough will be dry and continuous, and many people will cough for more than an hour or have three or more coughing episodes within a day."
If one has lost their sense of smell or taste, then the chances are, this could be COVID. However, this symptom is also present in cold or in a flu.
For people who have Covid, the NHS advises staying home and avoiding contact with others if they or their children have symptoms and either develop a high temperature or feel too unwell to work, attend school, manage childcare, or carry out daily activities. If you are unsure about the cause, it is important to speak with a doctor.
Dr Parmar emphasized: "after all, it is always better to be safe than sorry when it comes to health."
What Is Flu?
The flu is a common respiratory illness that happen from the influenza virus. The common flu symptoms are:
- Fever
- Sore Throat
- Runny Nose
- Fatigue
- Body Aches
- Cough
- Headaches
What Is COVID-19?
As per the US Centers for Disease Control and Prevention (CDC), COVID-19 is a respiratory illness caused by the coronavirus. The common symptoms include:
- Fever
- Cough
- Fatigue
- Headache
- Nausea
- Sore Throat
- Runny Nose
- Loss of smell or taste
COVID-19 could also have some long-lasting symptoms unlike flu or cold, that could seem unrelated to the original infection.
As per the Ohio State University, the most recent COVID variant is XFG or the Stratus variant. Another new variant that causes the 'razor blade' like sore throat is Nimbus.
The symptoms of this new variant includes:
- Congestion
- Cough
- Fever
- Headache
- Sore throat
- Muscle Aches
'Razor blade' Throat
NB.1.8.1 or the Nimbus variant is a subvariant of Omicron, which is a dominant COVID variant since late 2021. Omicron variants tend to cause more throat problems than the other variants seen earlier.
The COVID virus binds to ACE2 receptors. According to WebMD, the cells in your nose and throat contain more ACE2 receptors than those deeper in the lungs, which makes them easier targets for Omicron variants. Once the virus attaches to these receptors in the upper airway, your immune system begins to respond.
© 2024 Bennett, Coleman & Company Limited

