- Health Conditions A-Z
- Health & Wellness
- Nutrition
- Fitness
- Health News
- Ayurveda
- Videos
- Medicine A-Z
- Parenting
Can You Detect Dementia With An Eye Test?

Dementia. It is a brain condition that causes loss of cognitive function, which includes thinking, remembering and reasoning. It can also affect a person's ability to perform daily activities. It is a progressive neurological condition, which means the ability to communicate, or to perform cognitively deteriorates with time. You can delay the deterioration, but cannot stop it. But how does one delay the progress without knowing that it is happening? Well now, this can be achieved as Scottish researchers are working on a new AI tool that uses high-street opticians to spot early signs of dementia.
Now, dementia can be diagnosed through an eye test.
AI, Eye Test, And Dementia
Scottish scientists from the NeurEye research team have found that photographs taken of the retina at the back of the eye can indicate of brain health. It is done using AI software to analyze the information. Scientists also use this to spot signs of diseases before any symptoms are even experienced.
The team of scientists has collected a million eye scans from opticians across Scotland, which is also the largest data set of this kind. With the help of AI, they have developed an algorithm that can assess the health of the blood vessels in the eye that indicates neurogenerative diseases.
The database built by the team can be applied to photographs taken during routine eye checkups and could be used by clinicians to prevent diseases from occurring. It could also help them in diagnosing conditions at an earlier stage than what they currently can.
How It Works?
The blood vessels in the eye are small and fine, which means they show up conditions earlier than any other part of our body. Balijean Dhillon, who is part of the research group led by the University of Edinburg and researchers from Glasgow Caledonian University said that eyes can reveal more than was thought possible.
All the systems of the body are represented in eye. In fact, the diseases like cataracts, glaucoma, macular degeneration, problem with vision could also detect vascular system, heart health, high blood pressure, diabetes and even neurological conditions. While some of these conditions may show up late, eye care can detect it way before. The earlier you find it, the better it is for you to be able to delay the deterioration.
What Is Dementia?
Dementia is an umbrella term to describe diseases that cause people to lose their cognitive functions. These diseases gradually progress decreasing the ability for someone to function in daily life and take care of themselves. There are some medications used to delay the onset of it and to manage it. People can reduce the chances of developing it by following a healthy diet and lifestyle.
Types of Dementia
Different types of dementia occur due to different reasons. Some types of this disease are:
Alzheimer’s Disease
Alzheimer’s disease occurs when two abnormal proteins (tau and amyloid protein) build up in the brain. Some of its diseases include mental confusion, short-term memory loss, and personality and behaviour changes. In later stages, people may start having trouble talking, recalling distant memories and have issues with walking.
Vascular Dementia
Vascular dementia may occur because of a stroke or atherosclerosis. Atherosclerosis is the hardening of the arteries from plaque building up gradually inside of them. It blocks and damages blood vessels in the brain. This disease has symptoms such as memory problems, confusion, concentration problems and difficulty in completing tasks.
Mixed Dementia
Mixed dementia is a combination of two or more types of the disease. Sometimes, Alzheimer’s disease combined with vascular dementia causes mixed dementia. The health condition usually declines faster in people with mixed dementia than those who only have one type.
Huntington’s Disease
A mutation in the huntingtin(HTT) gene causes a breakdown in the brain’s nerve cells and it is responsible for Huntington’s. This disease causes body movement control problems, trouble thinking, decision-making, memory trouble and personality changes.
Traumatic Brain Injury
Someone may develop dementia-like symptoms if they suffer from repeated physical trauma to their head. Symptoms may appear after a long time and may include memory loss, behaviour or mood changes, slurred speech and headaches.
Parkinson’s Disease
People who have Parkinson's disease may develop secondary dementia in the later stages. Some of its symptoms are having trouble with thinking or speaking. Patients may have hallucinations and delusions, or suffer from depression.
Normal Pressure Hydrocephalus(NPH)
When Cerebrospinal Fluid(CSF) builds up in the brain’s ventricles the excess build-up harms the brain and this causes Normal Pressure Hydrocephalus(NPH). A brain infection, brain injury, bleeding in the brain or any previous brain surgery can also cause this condition.
This disease has some symptoms such as poor balance, forgetfulness, and short attention span, loss of bladder control, frequent falls and mood swings.
Infections
Some infections such as HIV infection, syphilis as well as Lyme disease can cause dementia-like symptoms. Urinary Tract Infections or UTIs, and lung infections can cause symptoms that match dementia.
Central Nervous infections and brain infections can cause cognitive symptoms. Also, COVID-19 symptoms include acute delirium or brain fog.
Unique Symptoms Of Vitamin D Deficiency

Credits: Canva
Long winters and lack of sunlight has renewed attention on vitamin D deficiency, a condition closely linked to bone health and overall well-being. Health data show that the problem is far more widespread than many realize, with potential consequences that range from brittle bones to mood changes.
Vitamin D and Its Role in the Body
Vitamin D plays a crucial role in helping the body absorb calcium, an essential mineral for strong bones and teeth. Without enough vitamin D, calcium absorption drops, weakening bone structure over time. This increases the risk of fractures, particularly among older adults.
Beyond bone metabolism, vitamin D also supports muscle function and contributes to a healthy immune response. Researchers have also explored its influence on mental well-being, as vitamin D receptors are present in several areas of the brain.
Deficiency Affects a Large Section of Adults
According to figures from the Robert Koch Institute, around 30 percent of adults in Germany have insufficient vitamin D levels. This is striking, given that the vitamin is produced by the body when skin is exposed to sunlight.
Experts point to modern lifestyles as a key reason. Many people spend most of their day indoors, often working in offices with little exposure to natural light. Seasonal factors also play a role, as sunlight is weaker and less frequent during autumn and winter months. In such conditions, relying on sunlight alone is often not enough to maintain healthy vitamin D levels.
Can Diet Help Fill the Gap?
Food can support vitamin D intake, although it usually provides smaller amounts compared to sunlight. Fatty fish are among the best dietary sources. Salmon, herring, eel, tuna, and pike perch contain relatively high levels of the vitamin and are often recommended for people at risk of deficiency.
Other animal-based options include eggs, liver, beef, and butter. For those who avoid animal products, plant-based sources can contribute modest amounts. Mushrooms, spinach, kale, broccoli, and Brussels sprouts are commonly mentioned. Some fruits such as avocados, kiwis, oranges, bananas, and figs are also included in vitamin D-friendly diets, though their contribution is limited.
Read: Vitamin D Supplements Under Scrutiny As It Fails Safety Test
Because many of these foods are eaten infrequently, especially fish, diet alone often fails to correct a deficiency.
Symptoms Linked to Low Vitamin D Levels
Vitamin D deficiency can show up in different ways. Many people report persistent fatigue, low mood, or depressive symptoms. While studies support a connection, researchers note that the exact biological pathways are still being studied.
Physical signs are often related to bone health. Weakened bones can increase the risk of fractures and cause general bone pain. Digestive issues and reduced tolerance to certain foods have also been reported in some cases. A deficiency is usually confirmed through a blood test ordered by a doctor.
When Too Much Becomes Harmful
While deficiency is common, excessive vitamin D intake can also pose risks. Health experts stress that overdoses do not occur through sunlight or normal diets, but through high-dose supplements taken over time.
Too much vitamin D can raise calcium levels in the blood, a condition known as hypercalcemia. This may lead to kidney damage, heart rhythm problems, and calcification of blood vessels. Individual risk varies depending on factors such as body weight, metabolism, and alcohol consumption, making medical guidance essential before supplement use.
Breast Cancer Signs That Do Not Feel Like Cancer, Explain Doctors

Credits: iStock
On World Cancer Day 2026, we at Health and Me is focussing on the most common cancer among women in India. Breast Cancer, which accounts for over 216,000 new cases every year, as per the 2022 data. This means, 28.2 per cent of female cancers are attributed to breast cancer. What is more tragic is that one woman is diagnosed with breast cancer every four minutes, and one dies every eight minutes in the country.
While, we all know that finding a lump is the red flag, there are other signs that women often miss that delays their detection. Health experts are increasingly warning that this narrow understanding may be delaying early diagnosis for many patients. New medical insights suggest that several lesser-known changes in breast tissue, skin and nipple appearance may signal cancer but often go unnoticed or get dismissed as harmless hormonal changes.
Read: More Than A Diagnosis: Cancer Survivors Share The Small Wins That Helped Them Heal
Breast Cancer Is Not Just A Lump
Data from a consumer survey commissioned by The Ohio State University Comprehensive Cancer Center shows that 93 percent of adults identify a lump as a symptom of breast cancer. But fewer than half are aware of several other warning signs that could appear much earlier.

Experts warn that this knowledge gap can be risky because not all breast cancers form lumps that are easily felt. Breast medical oncologist Ashley Pariser explains that screening mammography remains the most effective tool for detecting breast cancer at its earliest and most treatable stages. She adds that being familiar with the normal look and feel of one’s breast tissue helps people detect subtle changes faster and seek timely medical care.
Pariser notes that many breast changes can occur due to aging or childbirth. Still, she stresses that breast cancer can present in multiple ways, making it important for individuals to report unusual symptoms without delay.
Signs That Should Not Be Ignored
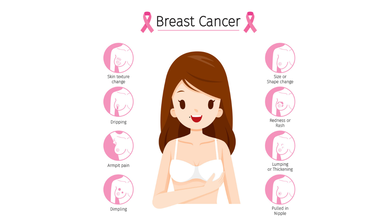
According to Dr Kanchan Kaur, Oncoplastic Breast Surgery Specialist, structural changes in the breast are among the most overlooked early warning signs. She highlights that while lumps are common indicators, deformations in breast shape such as flattening, indentation or dimpling should not be ignored.
Read: AI Detects More Breast Cancer Cases in Landmark Swedish Study
Dr Kaur also points out that an unusual increase or decrease in breast size, particularly when it affects only one breast, and sudden changes in breast symmetry may signal an underlying issue. She advises that these signs warrant clinical evaluation even if they appear painless or gradual.
Another concerning sign is skin texture change. She explains that a reddish, pitted texture resembling the surface of an orange or a marble-like area under the skin can indicate deeper tissue abnormalities. Any area of the breast that looks or feels noticeably different from surrounding tissue should be assessed by a doctor.
Nipple Changes Can Be Early Red Flags
Both research findings and clinical observations highlight nipple changes as key indicators that are often missed. Survey results from Ohio State University show that only about one-third of respondents recognized nipple inversion or retraction as a symptom of breast cancer.
Dr Kaur notes that nipples can provide early clues about breast disease. Symptoms such as newly inverted nipples, dimpling around the nipple, scaly red rashes, burning or itching, and ulceration should prompt medical attention.
Read: Oncologists Warns Of The Cancer Rising Among Women in India
Clear or bloody nipple discharge that is unrelated to pregnancy or breastfeeding is another warning sign. While discharge can occur due to benign causes, experts recommend prompt evaluation to rule out cancer.
Specialists at Moffitt Cancer Center caution that symptoms such as breast tenderness, swelling or changes in fullness are often mistaken for routine hormonal fluctuations. Because these symptoms frequently overlap with premenstrual changes, many women delay consulting a specialist.
Experts from the center advise that persistent breast pain, swelling or unusual fullness that does not resolve within a few days should be medically evaluated. They emphasize that sudden nipple inversion, discharge or skin texture changes require immediate attention.
World Cancer Day 2026: India’s 10 Most Common Cancers, Explains Doctor
Credits: Canva
Cancer trends in India are changing rapidly, driven by lifestyle patterns, environmental exposure, infections, and limited access to early healthcare in some regions. According to Dr Puneet Gupta, Chairman of Oncology Services at Asian Hospital, understanding early warning signs and adopting preventive habits can significantly improve survival outcomes.
“Cancer patterns in India are the results of multiple factors ranging from lifestyle, environmental exposure, infections and access to timely care,” Dr Gupta explained, adding that early symptoms can appear months or even years before the disease reaches advanced stages.
Breast Cancer: The Most Common Cancer In Women
Dr Gupta noted that breast cancer is frequently seen in women, especially after the age of 40. He highlighted that the disease often develops silently and without pain.
He explained that warning signs may include lumps in the breast or under the arm, changes in breast shape, skin dimpling, inward turning of the nipple, or unusual discharge. “Do not ignore these changes,” he cautioned. Regular self-examination, along with timely imaging tests such as mammography, ultrasound, or MRI, can help detect breast cancer early.
Cervical Cancer: Strongly Linked To HPV Infection
Cervical cancer mainly affects women between 30 and 60 years. Dr Gupta emphasised that HPV infection remains the leading risk factor. Early symptoms can include abnormal vaginal bleeding, bleeding after intercourse, or persistent pelvic pain, although early stages often remain symptom-free.
He stressed that routine Pap smear screening and HPV vaccination play a crucial role in prevention and early diagnosis.
Lung Cancer: Rising Risk Beyond Smoking
While lung cancer remains more common in men, Dr Gupta pointed out that cases among women are rising as well. Smoking is the primary cause, but exposure to fine particulate air pollution (PM2.5) also contributes to the risk.
He warned that persistent cough, chest pain, breathing difficulty, unexplained weight loss, or coughing blood require immediate medical evaluation, particularly in people with a history of tobacco use.
Oral Cancer: A Major Concern In India
Oral cancer remains widespread due to tobacco, gutka, areca nut consumption, and HPV infection. Dr Gupta explained that long-lasting mouth ulcers, red or white patches inside the mouth, jaw stiffness, or swallowing difficulty are early red flags. Regular dental and oral examinations can help detect early cancerous changes.
Colorectal Cancer: Lifestyle-Linked Risks
According to Dr Gupta, colorectal cancer is increasingly being diagnosed in adults around 40 years of age. Sedentary lifestyles, low-fiber diets, and excessive red meat intake are major contributing factors.
He said symptoms such as blood in stool, persistent bowel habit changes, abdominal pain, or unexplained anaemia should not be overlooked. Early screening and genetic testing in high-risk individuals can significantly improve outcomes.
Stomach Cancer: Often Shows Subtle Symptoms
Dr Gupta explained that stomach cancer may initially present as indigestion, early fullness, nausea, or unexplained weight loss. It is often associated with long-term Helicobacter pylori infection, smoking, and salt-heavy diets. Persistent digestive discomfort warrants medical attention.
Prostate Cancer: Common But Often Slow Growing
Prostate cancer typically affects men above 50 and usually progresses gradually. Dr Gupta noted that difficulty urinating and frequent nighttime urination are common early symptoms. Regular check-ups help detect the disease before complications arise.
Esophageal Cancer: Linked To Lifestyle And Nutrition
Tobacco use, alcohol consumption, poor nutrition, and iron deficiency increase the risk of esophageal cancer. Dr Gupta advised that swallowing difficulty, chest discomfort, or unexplained weight loss should prompt evaluation through tests like endoscopy or barium swallow.
Ovarian Cancer: Often Missed Due To Vague Symptoms
Dr Gupta explained that ovarian cancer frequently goes undetected due to non-specific symptoms such as bloating, abdominal discomfort, or early satiety. Women with persistent symptoms, particularly those with a family history of breast or ovarian cancer, should seek medical evaluation.
Liver Cancer: Screening Is Crucial For High-Risk Groups
Liver cancer often develops in individuals with chronic liver disease. Symptoms such as jaundice, abdominal swelling, or persistent pain usually appear late. Dr Gupta stressed that hepatitis vaccination and screening among high-risk groups are vital for prevention.
Lifestyle Changes And Screening Can Reduce Risk
Dr Gupta emphasized that although cancer cannot be completely prevented, a significant proportion of cases are linked to modifiable risk factors. Avoiding tobacco, maintaining a healthy weight, consuming balanced nutrition, managing stress, and staying physically active can lower risk.
He added that vaccinations against HPV and hepatitis further reduce cancer risk, while regular screening helps detect cancers at pre-cancer or early stages. “Education, prevention and early detection make the difference between late-stage disease and long-term survival,” Dr Gupta concluded.
© 2024 Bennett, Coleman & Company Limited

