- Health Conditions A-Z
- Health & Wellness
- Nutrition
- Fitness
- Health News
- Ayurveda
- Videos
- Medicine A-Z
- Parenting
Can You Drink Too Much Water?
Image Credit: Canva
From controlling body temperature and flushing out toxins, adequate hydration plays a vital role in our general health and well-being, water is a life essential. However, while dehydration garners significant attention, overhydration, or drinking excessive amounts of water, is a condition that can have serious and sometimes fatal consequences.
Although it may sound bizarre since drinking water is said to be the solution for most health related problems it is important to recognize how much water is considered "too much" or the risks involved with being overhydrated can maintain a healthy balance.
What Is Water Intoxication?
Water intoxication, also termed hyperhydration, water poisoning or water toxemia, develops when an individual drinks much more water than the kidney can excrete. The main function of the kidneys in the human body is the processing and excretion of excess water. However, the human kidneys can process only up to 0.8 to 1.0 liters of water at a time. Drinking an amount that exceeds this may overwhelm the kidneys and put the electrolyte balance out of sync in the human body.
Electrolytes, especially sodium, are essential in maintaining fluid balance within and outside cells. Hyponatremia is the condition when sodium levels fall below 135 mmol/L, resulting from excessive water intake. This causes water to shift into cells, swelling them. In the brain, this can cause severe complications, including coma or even death.
Symptoms of Water Intoxication
The symptoms of water intoxication vary from mild to severe. Early symptoms are often similar to dehydration, which makes self-diagnosis challenging. Common symptoms include:
- Headaches
- Nausea and vomiting
- Muscle cramps or weakness
- Fatigue or drowsiness
- Confusion and disorientation
In more serious cases, water intoxication can cause seizures, loss of consciousness, or swelling in the brain. These complications can be fatal if left untreated.
A notable case occurred in 2007 when a woman participating in a water-drinking contest tragically died after consuming nearly two gallons of water in under two hours. More recently, actress Brooke Shields experienced a grand mal seizure attributed to excessive water consumption.
Causes of Water Intoxication
Water intoxication is rare, but certain scenarios can increase the risk:
1. Sporting Events and Endurance Training
These endurance athletes are prone to water intoxication, especially if they drink large amounts of water without replacing lost electrolytes. Hyponatremia usually happens during long races or marathons as individuals mistake fatigue and muscle cramps for dehydration and continue drinking water in excess.
2. Military Training
Overhydration among military personnel is usually due to severe physical activity in extreme environmental conditions. The total number of hyponatremia cases documented from 2007 through 2022 for the active duty in the United States exceeds 1,600, with a note to this problem on exertion-related overhydration.
3. Mental Health Conditions
Compulsive water drinking, known as psychogenic polydipsia, is linked with some mental illnesses such as schizophrenia and psychosis. People with these conditions tend to drink too much water, causing a hazardous electrolyte imbalance.
4. Drug Abuse
Drugs such as MDMA (ecstasy) raise the body temperature and make people thirsty, and at times, some people tend to drink excess water at events like music festivals. MDMA also leads to urine retention, thus exacerbating the dangers of water intoxication.
How Much Water Is Too Much?
The exact amount of water that causes intoxication varies from one person to another. However, drinking more than 1 liter of water per hour for several hours raises the risk. For healthy individuals, the risk of overhydration is low unless taking part in extreme physical activity or ignoring thirst cues.
Certain medical conditions, such as kidney or liver disorders, can impair the body's ability to process fluids, and even moderate water intake may be harmful. Similarly, certain medications, such as diuretics and antipsychotics, can affect the perception of thirst or fluid regulation.
How Much Water Is Enough?
The widely touted recommendation of eight 8-ounce glasses of water per day has little basis in fact. According to the National Academy of Medicine, a daily total fluid intake is about 15 cups (3.7 liters) for males and 11 cups (2.7 liters) for females, from beverage sources and from food. Usually, about 20 percent of daily hydration comes from foods such as fruits and vegetables.
A better rule of thumb is to listen to your body and drink water based on thirst. Use the color of your urine as an indicator:
- Light yellow urine indicates proper hydration.
- Dark yellow urine may indicate dehydration.
Older adults, whose thirst mechanisms may decline with age, should be proactive about maintaining hydration, especially during illness or hot weather.
Water Intoxication vs. Dehydration
The symptoms of water intoxication—such as headaches, fatigue, and muscle weakness—are similar to those of dehydration. If you are unsure which condition you are experiencing, seek medical attention immediately rather than self-treating with more water.
Preventing Water Intoxication
To avoid the dangers of overhydration:
- Drink water gradually throughout the day rather than consuming large amounts at once.
- Replace lost electrolytes post high-intensity exercise or heavy sweating.
- Consider using sports drinks or salty snacks to help replenish sodium.
- Keep track of fluid consumption during long-duration activities, and do not consume more water than the body is losing in terms of electrolytes.
- If on medications or have specific medical conditions, check with your doctor regarding the safety of drinking water.
For signs of severe water intoxication-including confusion, drowsiness, seizures, and loss of consciousness-customer is advised to seek medical assistance immediately. In the meanwhile, a salty snack would help to temporarily correct low sodium levels.
Hydration is important to health, but overhydration can be a serious risk; the secret is in finding a balance. Drink enough water to satisfy your body, but not so much that it overwhelms your system. Remember, water is life, but moderation keeps it that way.
Hyponatremia (low sodium level in the blood). National Kidney Foundation. 2023.
Water Toxicity. NIH. 2023
Exercise-Associated Hyponatremia: 2017 Update. Front Med (Lausanne). 2017
Update: Exertional Hyponatremia Among Active Component Members of the U.S. Armed Forces, 2007–2022
Unique Symptoms Of Vitamin D Deficiency

Credits: Canva
Long winters and lack of sunlight has renewed attention on vitamin D deficiency, a condition closely linked to bone health and overall well-being. Health data show that the problem is far more widespread than many realize, with potential consequences that range from brittle bones to mood changes.
Vitamin D and Its Role in the Body
Vitamin D plays a crucial role in helping the body absorb calcium, an essential mineral for strong bones and teeth. Without enough vitamin D, calcium absorption drops, weakening bone structure over time. This increases the risk of fractures, particularly among older adults.
Beyond bone metabolism, vitamin D also supports muscle function and contributes to a healthy immune response. Researchers have also explored its influence on mental well-being, as vitamin D receptors are present in several areas of the brain.
Deficiency Affects a Large Section of Adults
According to figures from the Robert Koch Institute, around 30 percent of adults in Germany have insufficient vitamin D levels. This is striking, given that the vitamin is produced by the body when skin is exposed to sunlight.
Experts point to modern lifestyles as a key reason. Many people spend most of their day indoors, often working in offices with little exposure to natural light. Seasonal factors also play a role, as sunlight is weaker and less frequent during autumn and winter months. In such conditions, relying on sunlight alone is often not enough to maintain healthy vitamin D levels.
Can Diet Help Fill the Gap?
Food can support vitamin D intake, although it usually provides smaller amounts compared to sunlight. Fatty fish are among the best dietary sources. Salmon, herring, eel, tuna, and pike perch contain relatively high levels of the vitamin and are often recommended for people at risk of deficiency.
Other animal-based options include eggs, liver, beef, and butter. For those who avoid animal products, plant-based sources can contribute modest amounts. Mushrooms, spinach, kale, broccoli, and Brussels sprouts are commonly mentioned. Some fruits such as avocados, kiwis, oranges, bananas, and figs are also included in vitamin D-friendly diets, though their contribution is limited.
Read: Vitamin D Supplements Under Scrutiny As It Fails Safety Test
Because many of these foods are eaten infrequently, especially fish, diet alone often fails to correct a deficiency.
Symptoms Linked to Low Vitamin D Levels
Vitamin D deficiency can show up in different ways. Many people report persistent fatigue, low mood, or depressive symptoms. While studies support a connection, researchers note that the exact biological pathways are still being studied.
Physical signs are often related to bone health. Weakened bones can increase the risk of fractures and cause general bone pain. Digestive issues and reduced tolerance to certain foods have also been reported in some cases. A deficiency is usually confirmed through a blood test ordered by a doctor.
When Too Much Becomes Harmful
While deficiency is common, excessive vitamin D intake can also pose risks. Health experts stress that overdoses do not occur through sunlight or normal diets, but through high-dose supplements taken over time.
Too much vitamin D can raise calcium levels in the blood, a condition known as hypercalcemia. This may lead to kidney damage, heart rhythm problems, and calcification of blood vessels. Individual risk varies depending on factors such as body weight, metabolism, and alcohol consumption, making medical guidance essential before supplement use.
Breast Cancer Signs That Do Not Feel Like Cancer, Explain Doctors

Credits: iStock
On World Cancer Day 2026, we at Health and Me is focussing on the most common cancer among women in India. Breast Cancer, which accounts for over 216,000 new cases every year, as per the 2022 data. This means, 28.2 per cent of female cancers are attributed to breast cancer. What is more tragic is that one woman is diagnosed with breast cancer every four minutes, and one dies every eight minutes in the country.
While, we all know that finding a lump is the red flag, there are other signs that women often miss that delays their detection. Health experts are increasingly warning that this narrow understanding may be delaying early diagnosis for many patients. New medical insights suggest that several lesser-known changes in breast tissue, skin and nipple appearance may signal cancer but often go unnoticed or get dismissed as harmless hormonal changes.
Read: More Than A Diagnosis: Cancer Survivors Share The Small Wins That Helped Them Heal
Breast Cancer Is Not Just A Lump
Data from a consumer survey commissioned by The Ohio State University Comprehensive Cancer Center shows that 93 percent of adults identify a lump as a symptom of breast cancer. But fewer than half are aware of several other warning signs that could appear much earlier.

Experts warn that this knowledge gap can be risky because not all breast cancers form lumps that are easily felt. Breast medical oncologist Ashley Pariser explains that screening mammography remains the most effective tool for detecting breast cancer at its earliest and most treatable stages. She adds that being familiar with the normal look and feel of one’s breast tissue helps people detect subtle changes faster and seek timely medical care.
Pariser notes that many breast changes can occur due to aging or childbirth. Still, she stresses that breast cancer can present in multiple ways, making it important for individuals to report unusual symptoms without delay.
Signs That Should Not Be Ignored
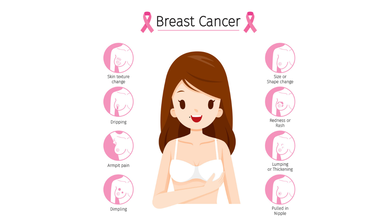
According to Dr Kanchan Kaur, Oncoplastic Breast Surgery Specialist, structural changes in the breast are among the most overlooked early warning signs. She highlights that while lumps are common indicators, deformations in breast shape such as flattening, indentation or dimpling should not be ignored.
Read: AI Detects More Breast Cancer Cases in Landmark Swedish Study
Dr Kaur also points out that an unusual increase or decrease in breast size, particularly when it affects only one breast, and sudden changes in breast symmetry may signal an underlying issue. She advises that these signs warrant clinical evaluation even if they appear painless or gradual.
Another concerning sign is skin texture change. She explains that a reddish, pitted texture resembling the surface of an orange or a marble-like area under the skin can indicate deeper tissue abnormalities. Any area of the breast that looks or feels noticeably different from surrounding tissue should be assessed by a doctor.
Nipple Changes Can Be Early Red Flags
Both research findings and clinical observations highlight nipple changes as key indicators that are often missed. Survey results from Ohio State University show that only about one-third of respondents recognized nipple inversion or retraction as a symptom of breast cancer.
Dr Kaur notes that nipples can provide early clues about breast disease. Symptoms such as newly inverted nipples, dimpling around the nipple, scaly red rashes, burning or itching, and ulceration should prompt medical attention.
Read: Oncologists Warns Of The Cancer Rising Among Women in India
Clear or bloody nipple discharge that is unrelated to pregnancy or breastfeeding is another warning sign. While discharge can occur due to benign causes, experts recommend prompt evaluation to rule out cancer.
Specialists at Moffitt Cancer Center caution that symptoms such as breast tenderness, swelling or changes in fullness are often mistaken for routine hormonal fluctuations. Because these symptoms frequently overlap with premenstrual changes, many women delay consulting a specialist.
Experts from the center advise that persistent breast pain, swelling or unusual fullness that does not resolve within a few days should be medically evaluated. They emphasize that sudden nipple inversion, discharge or skin texture changes require immediate attention.
World Cancer Day 2026: India’s 10 Most Common Cancers, Explains Doctor
Credits: Canva
Cancer trends in India are changing rapidly, driven by lifestyle patterns, environmental exposure, infections, and limited access to early healthcare in some regions. According to Dr Puneet Gupta, Chairman of Oncology Services at Asian Hospital, understanding early warning signs and adopting preventive habits can significantly improve survival outcomes.
“Cancer patterns in India are the results of multiple factors ranging from lifestyle, environmental exposure, infections and access to timely care,” Dr Gupta explained, adding that early symptoms can appear months or even years before the disease reaches advanced stages.
Breast Cancer: The Most Common Cancer In Women
Dr Gupta noted that breast cancer is frequently seen in women, especially after the age of 40. He highlighted that the disease often develops silently and without pain.
He explained that warning signs may include lumps in the breast or under the arm, changes in breast shape, skin dimpling, inward turning of the nipple, or unusual discharge. “Do not ignore these changes,” he cautioned. Regular self-examination, along with timely imaging tests such as mammography, ultrasound, or MRI, can help detect breast cancer early.
Cervical Cancer: Strongly Linked To HPV Infection
Cervical cancer mainly affects women between 30 and 60 years. Dr Gupta emphasised that HPV infection remains the leading risk factor. Early symptoms can include abnormal vaginal bleeding, bleeding after intercourse, or persistent pelvic pain, although early stages often remain symptom-free.
He stressed that routine Pap smear screening and HPV vaccination play a crucial role in prevention and early diagnosis.
Lung Cancer: Rising Risk Beyond Smoking
While lung cancer remains more common in men, Dr Gupta pointed out that cases among women are rising as well. Smoking is the primary cause, but exposure to fine particulate air pollution (PM2.5) also contributes to the risk.
He warned that persistent cough, chest pain, breathing difficulty, unexplained weight loss, or coughing blood require immediate medical evaluation, particularly in people with a history of tobacco use.
Oral Cancer: A Major Concern In India
Oral cancer remains widespread due to tobacco, gutka, areca nut consumption, and HPV infection. Dr Gupta explained that long-lasting mouth ulcers, red or white patches inside the mouth, jaw stiffness, or swallowing difficulty are early red flags. Regular dental and oral examinations can help detect early cancerous changes.
Colorectal Cancer: Lifestyle-Linked Risks
According to Dr Gupta, colorectal cancer is increasingly being diagnosed in adults around 40 years of age. Sedentary lifestyles, low-fiber diets, and excessive red meat intake are major contributing factors.
He said symptoms such as blood in stool, persistent bowel habit changes, abdominal pain, or unexplained anaemia should not be overlooked. Early screening and genetic testing in high-risk individuals can significantly improve outcomes.
Stomach Cancer: Often Shows Subtle Symptoms
Dr Gupta explained that stomach cancer may initially present as indigestion, early fullness, nausea, or unexplained weight loss. It is often associated with long-term Helicobacter pylori infection, smoking, and salt-heavy diets. Persistent digestive discomfort warrants medical attention.
Prostate Cancer: Common But Often Slow Growing
Prostate cancer typically affects men above 50 and usually progresses gradually. Dr Gupta noted that difficulty urinating and frequent nighttime urination are common early symptoms. Regular check-ups help detect the disease before complications arise.
Esophageal Cancer: Linked To Lifestyle And Nutrition
Tobacco use, alcohol consumption, poor nutrition, and iron deficiency increase the risk of esophageal cancer. Dr Gupta advised that swallowing difficulty, chest discomfort, or unexplained weight loss should prompt evaluation through tests like endoscopy or barium swallow.
Ovarian Cancer: Often Missed Due To Vague Symptoms
Dr Gupta explained that ovarian cancer frequently goes undetected due to non-specific symptoms such as bloating, abdominal discomfort, or early satiety. Women with persistent symptoms, particularly those with a family history of breast or ovarian cancer, should seek medical evaluation.
Liver Cancer: Screening Is Crucial For High-Risk Groups
Liver cancer often develops in individuals with chronic liver disease. Symptoms such as jaundice, abdominal swelling, or persistent pain usually appear late. Dr Gupta stressed that hepatitis vaccination and screening among high-risk groups are vital for prevention.
Lifestyle Changes And Screening Can Reduce Risk
Dr Gupta emphasized that although cancer cannot be completely prevented, a significant proportion of cases are linked to modifiable risk factors. Avoiding tobacco, maintaining a healthy weight, consuming balanced nutrition, managing stress, and staying physically active can lower risk.
He added that vaccinations against HPV and hepatitis further reduce cancer risk, while regular screening helps detect cancers at pre-cancer or early stages. “Education, prevention and early detection make the difference between late-stage disease and long-term survival,” Dr Gupta concluded.
© 2024 Bennett, Coleman & Company Limited

