- Health Conditions A-Z
- Health & Wellness
- Nutrition
- Fitness
- Health News
- Ayurveda
- Videos
- Medicine A-Z
- Parenting
- Web Stories
Doctors Call for Change in How Patients Are Treated at Life’s End

Credits: Canva
Doctors are calling for a national strategy and a public awareness campaign to improve end-of-life care, warning that dying is often treated as an “unexpected” event or last-minute crisis, even when a patient’s condition has long been deteriorating.
The Royal College of Physicians (RCP) said healthcare systems tend to prioritize curative treatments, despite many patients living with progressive, life-limiting conditions such as frailty or advanced chronic illness. The college urged a “cultural shift” in both healthcare and wider society to recognize the value of palliative and end-of-life care.
Dr Hilary Williams, RCP’s clinical vice president, as reported by The Independent, described recognizing the end of life as “an act of clinical courage and kindness.” She stressed that early planning could improve comfort, dignity and choice for patients.
Most Deaths Are Predictable, Yet Families Unprepared
Citing earlier research, the RCP said around 70% of people die from long-term health conditions that typically follow a predictable course, meaning death can be anticipated well in advance. Despite this, many patients and families are left unprepared, missing opportunities for open discussions that could shift the focus from aggressive treatment to quality-of-life support.
The RCP has recommended that the Government:
- Launch a public campaign on end-of-life and palliative care
- Support professional education to improve recognition and delivery of such care
- Develop a national strategy, including workforce training
The college also warned of barriers such as social care challenges, funding gaps and workforce shortages that limit timely, compassionate care.
Need for Honest Conversations
Dr Williams said too often recognition that someone is approaching the end of life happens only in the final days or weeks, usually in acute care settings. She called for valuing continuity of care, experienced decision-making and time for clinicians to hold honest conversations with patients and families.
“With treatment options expanding, knowing when to start or stop interventions and when to focus on quality of life has become more complex,” she said. “These are skills rooted in expertise, and the system must value them.”
Support from Other Medical Leaders
Dr Nick Murch, president of the Society for Acute Medicine, as reported in The Independent said better planning could allow more people to die with comfort, dignity and in a place of their choosing.
Dr Suzanne Kite, president of the Association for Palliative Medicine, emphasized the need for a national strategy to guarantee access to high-quality palliative care at any time and location, supported by training and public dialogue, as reported by The Independent.
Charity Sue Ryder, which provides hospice and palliative services, backed the RCP’s call, noting that some patients die before hospice admission due to late referrals. The charity urged healthcare professionals to consider palliative care from the point of a terminal diagnosis.
Government Response
A Department of Health and Social Care spokesperson said the Government aims to ensure compassionate, high-quality care from diagnosis to end of life. Under its 10 Year Health Plan, more healthcare will move from hospitals into communities, with palliative care playing a central role. The department has invested £100 million in hospices, the largest such funding in a generation.
Separate from Assisted Dying Debate
The RCP clarified that its position on end-of-life care is separate from its stance on the assisted dying Bill. While acknowledging deficiencies in the proposed legislation, the college urged further safeguards to protect vulnerable patients and maintain trust in the doctor-patient relationship.
What Eating Sugar Does to Your Teeth and Why Oral Health Could Shape Your Whole Body’s Wellbeing

In today’s world, things move very fast. Our meals are rushed, and food choices often lean toward convenience. Supermarkets overflow with ready-to-eat snacks, sugary drinks, and packaged meals. These quick bites may save time, but they come at a hidden cost, especially to our teeth. While these usually dominate health discussions, one silent victim of modern diets is often ignored, which is our smiles.
How Sugar Affects Teeth
According to Dr. Sanyukta Rege, Periodontist, Laxmi Dental Limited, sugar is in almost everything we consume. From breakfast to dinner, it shows up in cereals, sauces, juices, and snacks. When we eat sugary food, mouth bacteria feed on it. As they feed, they release acid which eats away the enamel. As enamel wears down, cavities form. Over time, untreated cavities lead to deeper decay, infections, and even tooth loss.
Why Oral Health Affects the Whole Body
Your mouth does not work in isolation. It connects to your entire body. Studies show that poor oral health links to heart problems, diabetes, and even respiratory diseases. Dr. Rege explains that if gum disease causes inflammation, bacteria can enter the bloodstream and travel to other organs.
Hence, tooth decay is not just about losing teeth. It is about how diet choices affect the body as a whole. What starts as a cavity can become a larger health issue, especially if ignored for years.
Escaping the Sugar Trap
Stopping sugar damage is not just about brushing more. It takes a group effort by everyone and here is how we can start:
Teach Kids Early
Children need to know that diet affects teeth. Schools should explain how sugar leads to decay. Lessons should include how to read food labels and choose better snacks. Dr. Rege says that instilling these lessons early makes healthier habits more likely to stick.
Help Parents Make Informed Choices
Parents shape early eating habits. By cooking more at home, checking labels, and offering fruits instead of packaged snacks, they can limit sugar exposure. Dr. Rege adds that this not only helps children’s teeth but also improves overall family health.
Make Dental Care Accessible
Regular check-ups can catch problems early. Sealants, fluoride treatments, and cleanings protect teeth. Free or affordable dental programmes in schools and communities can help reach more children. Dr. Rege stresses that prevention is far less costly than treating advanced dental issues.
Modern diets may be quick and tasty, but they often fail our long-term health. What we eat today shapes our bodies and our smiles tomorrow. The solution lies not just in brushing more but in eating smarter and acting earlier. As Dr. Rege reminds us, caring for your teeth is not just about avoiding cavities; it is an investment in your overall wellbeing.
Low FODMAP Diet Could Help Women with Endometriosis Finally Tackle Debilitating Gut Symptoms, Study

For many women with endometriosis, chronic and painful gastrointestinal symptoms are part of daily life, yet they often go untreated due to under-recognition by healthcare providers and a lack of evidence-based treatment options.
Endometriosis is a chronic, inflammatory gynaecological disorder affecting one in seven Australian women. It causes a range of unpredictable and often severe symptoms, including dysmenorrhoea (painful periods), pelvic pain (below the belly button and between the hips), and dyspareunia (pain during sexual intercourse). These symptoms disrupt daily life, impacting finances, relationships, mental health, and the ability to work, learn, socialise, exercise, and have children.
According to Jane Varney, Senior Research Dietitian at the Department of Gastroenterology, Monash University, gastrointestinal symptoms such as abdominal pain, bloating, distension, diarrhoea, constipation, and painful defecation affect more than three-quarters of sufferers. These symptoms often intensify during menstruation, occur regardless of bowel involvement, and overlap with irritable bowel syndrome (IBS), which affects between 10.6 per cent and 52 per cent of women with endometriosis.
Why current treatments fall short
Despite the high prevalence and burden of gut symptoms in endometriosis, treatment options are limited. Few treatments specifically target these gastrointestinal issues, and some, such as progesterone and opioid medications, can make them worse. Surgery can come with long waiting times, high costs, ongoing pain, and the need for repeat procedures, while hormone treatments and pain relief medicines are limited by modest effectiveness and troublesome side effects.
It is no surprise that many women turn to self-management strategies such as diet and nutritional supplements to help control symptoms and take an active role in their care. International data shows that more than 58 per cent of women with endometriosis have tried supplements, though only 43 per cent reported an improvement in pain. In Australia, three-quarters use fish oil, multivitamins, vitamin B, or vitamin D.
Dietary changes are also common. Surveys from Australia, Holland, the UK, and beyond reveal that between 27 per cent and 84 per cent of women with endometriosis use dietary modifications to manage symptoms, with many reporting benefits. Popular approaches include anti-inflammatory diets or avoiding red meat, gluten, dairy, lactose, FODMAPs, caffeine, soy, and alcohol. However, the evidence for most of these is limited or absent.
The EndoFOD study
Recognising the gap in evidence and the similarity of symptoms between IBS and endometriosis, Monash University researchers recently examined the effect of a low FODMAP diet on women with endometriosis and persistent gut symptoms.
The study was the first randomised controlled crossover feeding trial in this patient group. Thirty-five participants were assigned to a 28-day low FODMAP diet or a control diet based on Australian dietary guidelines, with both diets nutritionally matched except for their FODMAP content. After a washout period of at least 28 days, they switched to the other diet. Each diet began on the first day of a menstrual cycle to account for hormonal symptom fluctuations.
By the end of the trial, 60 per cent of participants responded to the low FODMAP diet, with significant improvements in gut symptom severity. Abdominal pain, bloating, stool consistency, and quality of life all improved. Changes were noticeable by week two, continuing steadily until the end of the intervention.
What it means for endometriosis care
These results offer the first evidence-based diet therapy for women with endometriosis. While the low FODMAP diet is not a replacement for medical or surgical treatment, it provides an effective additional tool for managing troublesome gut symptoms.
What’s next for diet research
Researchers emphasise that further studies are needed to confirm these results in real-world conditions. The trial controlled variables tightly by supplying participants with most of their food, ensuring adherence. In everyday life, however, patients face barriers such as motivation, understanding the diet, food availability, and convenience. The next step is a larger, multicentre trial involving dietitians teaching the approach, with participants applying it in their own kitchens. If these results are replicated outside the research setting, the low FODMAP diet could become a valuable and widely accessible adjunct to endometriosis management.
What Causes Epilepsy? 5 Common Reasons Why It Happens
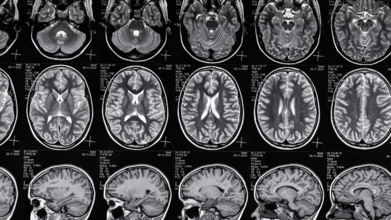
Credits: Canva
Epilepsy affects millions of people worldwide, yet it remains one of the most misunderstood neurological conditions. The disorder is marked by recurring seizures, sudden bursts of electrical activity in the brain , which can cause symptoms ranging from brief confusion and muscle twitches to severe convulsions.
While anyone can have a single seizure for a variety of reasons, epilepsy is diagnosed when a person experiences two or more unprovoked seizures. Experts say understanding the causes can help with both prevention and treatment.
Genetics Can Play a Role
In some cases, epilepsy runs in families, pointing to a genetic connection. Certain gene mutations can disrupt normal brain activity, making seizures more likely.
Genetic epilepsy can be inherited, but the link isn’t always straightforward, says neurologists. Different genes affect the brain in different ways, and researchers are still uncovering exactly how these changes lead to seizures.
Even without a family history, spontaneous mutations in a person’s genes can also result in epilepsy.
Brain Damage Can Lead to Epilepsy
Any structural damage to the brain can disrupt its electrical signalling, triggering seizures over time. This damage might be recent or decades old.
Common structural causes include:
- Birth complications that reduce oxygen supply to the brain
- Head trauma from accidents or falls
- Brain tumors
- Stroke or bleeding in the brain
“Sometimes the injury happened years earlier, such as during birth, but its effects on brain function appear much later,” says Dr Gabriel Martz, MD, FAES, writing for Hartford HealthCare, who is a neurologist and director of the Ayer Neuroscience Institute Epilepsy Center.
Infections and Autoimmune Conditions Can Be Triggers
Infections that cause brain inflammation, such as meningitis or encephalitis, can have long-term consequences. Even after recovery, scarring and other changes in brain tissue can increase the risk of seizures.
In other cases, the immune system mistakenly attacks the brain, a condition known as autoimmune encephalitis, which can also lead to epilepsy.
“These causes highlight why protecting brain health through early diagnosis and treatment of infections is so important,” specialist notes.
4Sometimes, the Cause is Unknown
Despite advances in brain imaging and genetic testing, many people with epilepsy never learn the exact cause.
“We don’t always get a clear answer,” Dr Martz notes. “Not knowing the cause can be frustrating, but it doesn’t make the condition less real or less treatable.”
This uncertainty means that in some cases, treatment focuses entirely on managing seizures rather than addressing an underlying trigger.
Lifestyle and Environment Matter
While lifestyle alone doesn’t cause epilepsy, certain factors can raise the risk by increasing the chances of brain injury or neurological stress. These include:
- Substance misuse
- Dangerous sports without protective gear
- Repeated concussions
“Protecting your brain is one of the best ways to reduce preventable risk,” doctor says. Wearing helmets, avoiding risky behavior, and staying away from drugs can make a real difference.
When to Seek Medical Advice
If you or someone you know experiences a first-time seizure, it’s essential to consult a doctor. Tests such as an MRI, EEG, or bloodwork can help identify potential causes and guide treatment.
Epilepsy affects people in deeply personal ways, not only in how seizures manifest but also in how the condition impacts daily life and emotional well-being. Understanding what lies behind it is the first step toward effective care and fuller, healthier lives.
© 2024 Bennett, Coleman & Company Limited

