- Health Conditions A-Z
- Health & Wellness
- Nutrition
- Fitness
- Health News
- Ayurveda
- Videos
- Medicine A-Z
- Parenting
- Web Stories

Credit: Canva
Getting Vaccine Reactions In Same Arm Boost Immune Response, Study Finds
Receiving a vaccine booster in the same arm as the first dose triggers a faster and stronger immune response and helps the body build protection faster, a new study from Australian scientists has revealed. The findings could help improve vaccine strategies and may eventually lead to vaccines that need fewer boosters. The study was published in the journal Cell and finds that the immune system responds more quickly when both doses are given in the same arm.
Why Will It Work?
Researchers have reasoned that getting jabbed in the same arm works better because immune cells in nearby lymph nodes, which are the body's infection-fighting hubs, become "primed" after the first shot. When the booster arrives in the same spot, these cells spring into action and help produce stronger antibodies. "This is a fundamental discovery in how the immune system organises itself to respond better to external threats," said the study's co-senior author Tri Phan, director of the Precision Immunology Program at the Garvan Institute.Researchers discovered this effect first in mice, then confirmed it in a clinical study involving 30 people who received the Pfizer COVID-19 vaccine. Those who had both doses in the same arm developed faster and more effective protection, especially against COVID-19 variants like Delta and Omicron. While both groups ended up with similar antibody levels after four weeks, the same-arm group gained protection more quickly, a potential game-changer during pandemic outbreaks.
"If you've had your COVID jabs in different arms, don't worry, our research shows that over time the difference in protection diminishes," said the study's co-senior author, Mee Ling Munier from the Kirby Institute.
How Do Vaccines Work?
The immune system has a wonderful layered system of defences, and when it comes to vaccines, two major defenses are activated. One of them is antibodies, which are proteins in the blood. Then you have something called cell-mediated immunity, which involves cells, usually T lymphocytes. You almost always get both. From a regulatory point of view, you often measure antibodies in people and basically know how effective a vaccine is in a population.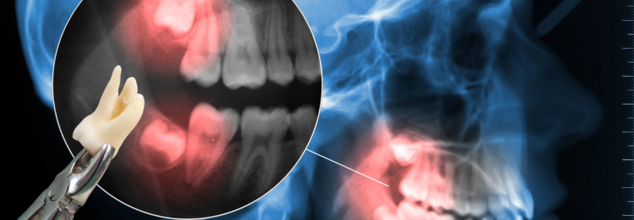
Credits: Canva
When Is It The Right Time To Get Your Wisdom Tooth Extracted?
As you grow older, a lot of things change in your body. Your body grows and develops. While some of these changes could be smooth, other transitions could create a bit of turmoil. One such is wisdom tooth.
What Is A Wisdom Tooth?
As per the National Library of Medicine, wisdom teeth come in at the very back of our mouth, with one at the end of each row of teeth. They usually do not fully develop until ages 18 to 24. This is when they appear and are commonly known as "troublemakers". This is because often in our jaws, there is not enough space for these teeth, and so it can cause pain when it comes out.
Often the growth of wisdom tooth could lead to pain and inflammation and thus, removal would be necessary.
Historically, wisdom tooth date back to our distant ancestors who had larger jaws and thus had more teeth. However, as time wet by and with evolution and changing eating practices, the jaws have shrunken and are thus too small for some people to accommodate the "extra" teeth. However, this does not mean that it causes problems for everyone. For many, these teeth can easily settle in.
The percentage of wisdom teeth extracted in women is significantly higher than men, this is because women often consult more often consult more than men, as is also noted in a 2021 study published in Annals of Medicine & Surgery, titled: The wisdom behind the third molars removal: A prospective study of 106 cases.
Another study published in the Journal of Oral Rehabilitation from 1987 also notes that women have a smaller maximum jaw opening than men. This could also be the reason why women need to get their wisdom tooth extracted more often than men.
What Are The Signs That Tell You To Extract Your Wisdom Tooth?
If you have these signs, you may want to consider extracting your wisdom tooth
Wisdom Tooth Impaction
This is when the third molars grow without fully emerging through your gums. This happens when they grow at an odd angle and emerge crooked, and cause further damage to the other healthy neighboring teeth. The impacted wisdom tooth could often grow at 180 degrees in the wrong direction into the jaw, and thus cause oral infection, jawbone cysts, and gym disease.
Gum Inflammation
This happens when food, plaque, and bacteria get underneath your gum tissue. Swollen or inflamed gums are often the first signs of wisdom tooth impaction.
Stiff Jaw
If you witness your jaw being stiff, then this could be because your wisdom tooth is pressing against your other teeth.
Jaw Pain
This could also happen when your wisdom tooth is impacted and thus you face pain in your jaw, especially while you try to open your mouth.
Persistent Bad Breath or Taste In Your Mouth
Despite brushing and following all the oral hygiene routine, you still experience bad breath, it could be because wisdom tooth have caused decay to your adjacent teeth.
So, When Should You Remove It?
If you face any of these signs, it is best to see your dentist and consult with them before you go ahead with an extraction surgery. Furthermore, the American Dental Association notes that you may need to have your wisdom tooth taken out, if you have:
- Pain in or near your wisdom teeth.
- Repeated infection of soft tissue behind the lower last tooth.
- Fluid-filled sacs called cysts.
- Tumors.
- Damage to nearby teeth.
- Gum disease.
- Widespread tooth decay

Credits: Canva
What Is Medetomidine? The Animal Sedative Now Turning Up In US Street Drugs
The Centers for Disease Control and Prevention (CDC) released three reports on Thursday that highlighted the clusters of medetomidine-related cases in Chicago, Philadelphia, and Pittsburgh. These reports have raised alarm about the growing presence of this drug in street opioids and the potential complications it brings to treatment and recovery.
What Is Medetomidine?
As per the American College of Medical Toxicology (ACMT), it is an alpha-2 agonist, similar to clonidine and xylazine, that is used clinically as a sedative and analgesic. It is categorized as an NPS due to its novelty in use. The CDC in its Morbidity and Mortality Weekly Report notes that it is a canine veterinary agent used for its anesthetic and analgesic properties.
However, the National Library of Medicine's study titled Classics in Chemical Neuroscience: Medetomidine has noted that this drug "has recently been detected in the illicit drug supply alongside fentanyl, xylazine, cocaine, and heroin, producing pronounced sedative effective that are not reversed by naloxone."
As per the latest CDC report released on May 1, twelve confirmed and 26 probable cases of medetomidine-involved overdose occurred in Chicago. Fentanyl was present in all blood specimens and drug samples that tested positive for medetomidine.
It was first identified in North America’s illicit opioid market in 2022, medetomidine is now showing up more frequently in mixtures with synthetic opioids—particularly fentanyl, the drug driving most overdose deaths in the U.S.
Why Is This Worrisome?
In May 2023, Chicago officials noticed a spike in overdose cases where naloxone—the standard overdose-reversal medication—did not work as expected. After investigation, the city's health department confirmed 12 cases involving medetomidine, with over 160 more suspected or probable cases, including one potential death. This marks the largest known medetomidine cluster to date.
The two other CDC reports focused on medetomidine withdrawal. In Philadelphia, testing revealed medetomidine in 72% of illegal opioid samples collected in late 2023, overtaking xylazine in frequency. Patients exposed to medetomidine experienced a distinctive type of drug withdrawal that didn’t respond to usual medications for fentanyl or xylazine. However, a related medication called dexmedetomidine showed some success in managing symptoms.
Pittsburgh reported 10 similar cases around the same time, suggesting the issue is not isolated to one area but may be spreading through regional drug supplies.
Why Does It Matter?
The presence of sedatives like medetomidine in illicit opioids creates several public health challenges:
Reduced effectiveness of naloxone: Standard treatment protocols for overdoses may not work when sedatives are involved, increasing the risk of death.
Complicated withdrawals: The addition of new, unregulated substances alters the withdrawal process, often making it harder to treat.
Lack of awareness and testing: Many emergency responders and clinics do not routinely test for medetomidine, which could delay proper care.
This development adds a new layer to the already complex U.S. opioid crisis. As drug suppliers continue to mix opioids with a variety of sedatives and adulterants, health officials face an evolving battle. Experts stress the importance of broader toxicology screening, continued research, and expanding the availability of alternative treatments like dexmedetomidine.
While medetomidine isn’t yet as widespread as fentanyl or xylazine, its growing presence in cities like Chicago, Philadelphia, and Pittsburgh points to a potentially dangerous trend—one that will require urgent attention from both medical professionals and policymakers.
Credit: Canva
Phthalates In Microplastics Linked To Heart Diseases—One Simple Hack To Cut Down Risk
Microplastics pose a danger to the heart. While there is enough evidence to show that they clog arteries and exacerbate the risk of stroke, recent research has found that these teeny particles of plastic can trigger cardiovascular diseases. It is estimated that chemicals in plastic were linked to nearly 350,000 heart disease deaths across the world in 2018. Adding to that, is this study published in the journal eBioMedicine, which estimated that roughly 13 per cent of cardiovascular deaths among 55- to 64-year-olds worldwide that year could be attributed to phthalates.
Where Are Phthalates are esters of phthalic acids, which are added to plastics to increase their flexibility, transparency, durability, and longevity. They are found in personal care products like shampoos and lotions as well as in food containers and packaging. It is also possible to injest them through food, absorb them through skin from products containing them or breathe them from dust.
Some studies have shown an association between phthalates and cardiovascular disease, but there isn’t strong evidence to show that the chemicals directly cause heart issues, said Sung Kyun Park, a professor of epidemiology and environmental sciences at the University of Michigan School of Public Health. However, there is enough evidence that states that phthalates increase the risk of metabolic disorders like obesity and Type 2 diabetes, which can cause cardiovascular disease. One way phthalates may do this is by increasing oxidative stress—cell and tissue damage that happens when there are too many unstable molecules in the body—and by promoting inflammation.
Microplastics: Explained
Microplastics are extremely small particles—often less than five millimetres in size—created when larger pieces of plastic break down. They can enter the human body in multiple ways: through the air we breathe, the food we eat, and even skin contact. An even smaller subset, known as nanoplastics, measures under 1,000 nanometers and is completely invisible to the naked eye. Because of their minuscule size, these particles can infiltrate tissues, organs, and potentially disrupt biological functions.
One Simple Way To Mitigate Risk Of Microplastics
Amid growing concerns about microplastic contamination, especially in drinking water, scientists have been working on practical ways to mitigate exposure. In 2024, a research team from Guangzhou Medical Centre made a breakthrough. They discovered that a common household activity—boiling water—can significantly reduce microplastic content in tap water.
According to the team, combining boiling with basic filtration can remove up to 90% of nanoplastic and microplastic particles (NMPs) from household water. However, the method’s effectiveness varied depending on the type of water used. In areas where tap water contains higher mineral content, commonly referred to as "hard water," the technique proved especially efficient.
The secret lies in limescale. As hard water is heated, it forms limescale—a chalky white substance—which appears to create a sticky layer that traps microplastic fragments. Researchers found this natural process enhanced the removal of plastic particles from water, offering a practical and affordable solution for most households.
While more research is needed to fully understand the long-term health effects of microplastics, early evidence suggests they may be more dangerous than previously thought—especially for cardiovascular health.
© 2024 Bennett, Coleman & Company Limited

