- Health Conditions A-Z
- Health & Wellness
- Nutrition
- Fitness
- Health News
- Ayurveda
- Videos
- Medicine A-Z
- Parenting
- Web Stories
Having A Family Pet Can Decrease The Chances Of Your Kid Developing Eczema

(Credit-Canva)
Having a family pet is a favorable idea considered by many. While parents of young children are worried about bacteria and germs being an issue, there are also other factors to consider. Many studies, like ‘The Power of Pets’ published in the News in Health, have shown how pets play a very important role in a child’s development. They explain how pets have been observed to lower cortisol levels as well as lower blood pressure. They also pointed out that studies have found pets to lower the feeling of loneliness, increase social support as well, and boost your mood.
A new study shows a favorable result for families who wish to have pets, especially dogs, as they not only passively help your kid’s health, but they can also have an active effect on them.
New research suggests that having a family dog might lower a baby's chances of getting eczema later in life. This study, published on June 4th in the journal Allergy, indicates that being around dogs could actually change how a child's genes react to eczema, by calming down skin inflammation.
How Does Eczema Affect Kids?
Researchers explained that while we know genes play a role in eczema risk and that dogs might be protective, this is the first study to show how this happens at a very basic level. Eczema happens when something irritates the skin, causing it to become dry, itchy, and inflamed. We know some people are born more likely to get eczema, but exactly how their genes and their surroundings work together to either increase or decrease this risk hasn't been clear.
How Was The Research Conducted?
The researchers conducted a comprehensive analysis of data from 16 previously conducted studies. Their goal was to identify interactions between 24 specific genetic variants already known to be linked to eczema and a list of 18 environmental factors that could potentially influence a baby's susceptibility to the condition later in life.
which included over 25,000 people, narrowed down the environmental factors to seven key ones: antibiotic use, owning a cat, owning a dog, breastfeeding, having an older sibling, smoking, and hygiene.
Dogs, Genes, and Inflammation
The team then applied these findings to data from another 254,000 people to see which genes and environmental factors had the biggest impact on eczema risk. This second look found that a baby's exposure to dogs affects the interleukin-7 gene. This gene is involved in making a type of immune protein that helps control inflammation. Lab tests showed that being around dogs interacts with a gene variation that might otherwise cause eczema, essentially reducing skin inflammation by changing how interleukin-7 proteins work in human skin cells.
The experts explained that their research aims to answer common questions parents ask, like "Why does my child have eczema?" and "What can I do to protect my baby?" While these findings are exciting, the researchers also stressed that more studies are needed to confirm what they found in the lab and to better understand exactly how dogs might affect human genes in this way. Researchers believes these findings give us a chance to tackle the rise of allergic diseases and protect future generations.
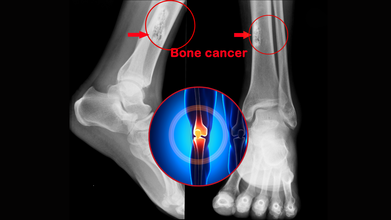
Bone Cancer Awareness Month: Bone Cancer Isn’t Just an Elderly Disease: When To Suspect A Tumor And Know The Risks At Any Age
Credits: Canva
Bone cancer develops when bone cells start to multiply rapidly and in an unusual manner. This results in break down of the bone. These bone cancer cells may also travel by blood to other oarts of the body like lung and other bones.
Bone tumours occur in two age groups. Children and adolescents and people above the age of 50 years. However it must be remembered that majority of the bony swellings are benign(non-cancerous).
What are the Signs and Symptoms of Bone Cancer?
The bone which is affected may start paining. The pain may be intermittent initially but can later become continuous as the disease progresses. The pain may be worse at night. There may be a swelling or lump in the area. The disease may weaken the bone to cause a fracture. All these symptoms can also be caused by conditions that are not bone cancer. So if you have these symptoms you must tell your doctor.
What Can The Doctor Do?
Your doctor can order an X-ray of the bone affected. If X-ray is suggestive of bone cancer other tests will be required. These include blood tests, imaging studies like CT scan and MRI scan to check the affected bone. A whole body bone scan or PET scan may required to see if the disease has spead to other parts of the body.
A biopsy is required to check if it is actually cancer. The biopsy is sent to a pathologist to confirm the diagnosis. The biopsy should be done by an experienced onco-surgeon. A wrongly placed biopsy site can be disastrous for the patient.
What Are the Treatment Options For Bone Cancer?
Bone cancer if detected in time can be cured. The treatment consists of mainly Sugery and Chemotherapy. Surgery these days involves what is known as limb salvage surgery. This is when the surgeon removes part of the arm or leg where the cancer is growing without removing the whole limb. Chemotherapy is required before and after surgery in many cases. It helps in killing cancer cells which may have spread by blood in the body. With early diagnosis and prompt treatment bone tumour can be cured in a large number of case especially in early stages. There are no common risk factors to bone cancers. Exposure to radiation and a family history are a few known factors.
The key to treatment of bone tumour is early referral to a specialist and management in a specilised oncology centre
My Eye Is Bleeding? What Does It Mean When You Have A Big Red Patch On The Whites Of Your Eye

(Credit-Canva)
A 13-year-old boy walked into the emergency room one day with bloodshot eyes. He didn't have any other eye problems like blurry vision, extra tears, discharge, or pain. He also didn't have a fever or any eye injury. His parents mentioned that for four days before his eyes turned red, he had been vomiting and had diarrhea a lot. This started after they returned home from a trip to Mexico that lasted a few weeks.
When doctors examined him, they found a healthy, awake boy who wasn't in any discomfort. Everything else about his body seemed normal, except for the very red eyes. The redness was in both eyes, underneath the clear outer layer, but there was no discharge, no sensitivity to light, and his eye movements and vision were fine.
Doctors believed his red eyes were caused by the extreme vomiting and gagging he experienced. This pressure likely made tiny blood vessels in his eye burst. He was admitted to the hospital for severe stomach flu. As his vomiting and diarrhea got better, the redness in his eyes also went away by itself within a few days.
A Scary Symptom But ‘Not So Scary’ Cause
According to the American Academy of Ophthalmology (AAO), a subconjunctival hemorrhage is simply one or more bright red spots on the white part of your eye. It happens because the clear covering of your eye, called the conjunctiva, has many tiny blood vessels. When one of these small vessels breaks, blood leaks out and gets trapped between the conjunctiva and the white of your eye (the sclera). This is what creates that noticeable red spot.
Even though these red spots can look alarming, a subconjunctival hemorrhage is usually harmless and will often heal on its own. The main symptom of a subconjunctival hemorrhage is just the red spot itself. You might not even realize you have it until you look in a mirror. Sometimes, you might feel a very slight irritation in your eye, but usually, there's no pain.
What Causes These Red Spots?
Most often, subconjunctival hemorrhages are caused by actions that briefly increase the pressure in your veins, such as:
- Coughing
- Sneezing
- Straining (like when lifting something heavy or having a bowel movement)
- This quick jump in pressure can cause those tiny blood vessels to break.
- Injuries to the eye, even something as simple as rubbing your eyes too hard, can also cause these spots.
Less common causes include:
- Diabetes
- High blood pressure
- Taking medicines that thin your blood, like aspirin or certain blood thinners
- Very rarely, a subconjunctival hemorrhage can be a sign of a blood clotting problem or another blood disorder affecting your whole body.
A subconjunctival hemorrhage typically heals by itself without any specific treatment. The time it takes to clear up depends on the size of the spot, usually ranging from a few days to a few weeks. If your eye feels a bit irritated, you can use artificial tears to help. If you find yourself getting these red spots often, your eye doctor will want to talk with you and might recommend further tests to figure out why.
When These Red Spots Are A Cause Of Concern
AAO explains that it is easy to mix up a hyphema with a common, harmless condition called a subconjunctival hemorrhage, which is just a broken blood vessel in the white part of your eye. A subconjunctival hemorrhage doesn't hurt. However, a hyphema is usually painful and needs proper medical attention right away, or it could cause lasting vision problems.
A hyphema is when blood collects in the front part of your eye. This happens in the space between the clear outer layer which is called the cornea and the colored part of your eye (the iris). The blood can cover some or all of your iris and the dark center of your eye which is the pupil. If you have a hyphema, your vision in that eye might be partly or completely blocked. Hyphema symptoms include,
- Blood in the front of your eye
- Sensitivity to light
- Pain in the eye
- Blurry, cloudy, or blocked vision
What Causes Hyphema?
Since most hyphemas are due to sports injuries, it's very important to wear proper eye protection when playing sports. Injuries from small, fast-moving balls, like in racquetball, can cause serious eye problems beyond just hyphema, such as cataracts, detached retinas, and glaucoma, which can even lead to blindness. However, it is treatable so it is best to visit a doctor to get it checked out
London Psychologist Gave Patients Ketamine, Now Loses License, Here's What We Know So Far

Credits: Wikimedia Commons and CBC news as submitted by Tatiana Zdyb
Tatiana Zdyb admitted to multiple professional misconduct charges, including intimate relationship with patient and misuse of psychedelic therapy
A London-based psychologist who offered ketamine-assisted psychotherapy to clients has been stripped of her license after admitting to serious professional misconduct, including sexual abuse of a patient, misrepresenting her credentials, and offering unproven treatments.
Zdyb, once publicly known for pioneering the use of psychedelic-assisted therapy in Southwestern Ontario, faced a disciplinary hearing on Wednesday before the Ontario College of Psychologists and Behaviour Analysts. The hearing addressed three separate notices of professional misconduct, culminating in the revocation of her license to practice.
The hearing, held in Toronto, heard that Zdyb engaged in an inappropriate and intimate relationship with a long-time patient, provided services unlikely to benefit clients, and misrepresented both her role and the safety of the treatments she was offering.
“These findings are not minor breaches,” said hearing chair Ian Nicholson. “They go to the core of your responsibilities as a regulated professional… Your actions represented a fundamental and egregious betrayal of that trust.”
The Psychedelic Controversy: What Is Ketamine Therapy?
Ketamine, originally developed as a fast-acting anesthetic for medical and veterinary use, has in recent years found a foothold in mental health care, particularly for patients with treatment-resistant depression. It is a controlled substance in Canada, meaning its use outside regulated medical or scientific settings is illegal.
When used under medical supervision, low-dose ketamine infusions or lozenges are believed to rapidly relieve depressive symptoms, sometimes within hours. However, the drug also has hallucinogenic effects and potential for misuse, raising concerns among medical professionals and regulators alike.
While Zdyb was not a medical doctor, she collaborated with prescribing physicians to incorporate ketamine into her psychotherapy sessions. She had previously promoted her clinic, under names like the MindSetting Institute and Zdyb Centre for Health Promotion, as one of the first in the region to offer this form of therapy.
ALSO READ: Matthew Perry Investigation: Can Ketamine Kill Someone?
Ketamine is an anaesthetic used to treat depression, anxiety and pain under supervised and controlled medical settings. However, it does have its side effects, which can lead to distortion of sight, sound and time. It can also produce calming and relaxing effects.
Ketamine increases a person’s heart rate and blood pressure. If overdosed, it can leave users confused and agitated and can cause them to hurt themselves without even realizing it. It can also lead to liver damage and bladder problems.
However, when used in moderation and under the supervision of medical doctors, it can treat depression where traditional antidepressants have failed.
Prof Rupert McShane, a University of Oxford psychiatrist who runs an NHS ketamine treatment clinic told BBC that ketamine “probably turns off the area of the brain that is involved in disappointment.”
In simple terms, it cannot, be if the dosage is given in a controlled setting and as prescribed. Ketamine infusion therapy uses drugs in small doses than those used for anaesthesia. It acts faster than traditional anti-depressants, but the effects also wear off way quickly. Which is why it is important to monitor patients’ mental state for relapsing back into depression and discouraging them from overdosing on it.
YOU MAY WANT TO READ: Can You Use Ketamine To Treat Depression?
Disciplinary Action Follows Settled Lawsuit
The College first issued an interim suspension of Zdyb’s licence in August 2023, pending investigation. But the roots of concern stretch back even further. Lawyer John Nicholson, who represented a former client of Zdyb's under the pseudonym “A.A.”, said his client’s mental health significantly deteriorated after receiving ketamine treatment under Zdyb’s care in 2020 for mild depression.
“She got worse,” Nicholson told CBC News. “And later, Zdyb recommended psilocybin [magic mushrooms] without having the training or expertise to manage that process. My client was unable to return to work and suffered greatly.”
The lawsuit alleged not only inappropriate treatment but also that Zdyb entered into a romantic relationship with A.A. during the course of her therapy, a clear violation of regulatory rules that prohibit any sexual relationship for at least one year after treatment ends. The case was settled out of court, with Nicholson confirming a monetary agreement but declining to share further details.
Admitted Misconduct and License Revocation
At Wednesday’s hearing, Zdyb admitted to all the allegations presented. Her legal representative, Grant Ferguson, acknowledged the “most serious” charge was the sexual relationship with a former client, which began in September 2022, the same month the patient ceased treatment.
But the College’s regulations are unequivocal: any romantic involvement within a year of therapy ending constitutes sexual abuse, carrying severe consequences including mandatory licence revocation.
© 2024 Bennett, Coleman & Company Limited

