- Health Conditions A-Z
- Health & Wellness
- Nutrition
- Fitness
- Health News
- Ayurveda
- Videos
- Medicine A-Z
- Parenting
- Web Stories
Hepatitis C in Children: What You Need to Know About Silent Symptoms, Hidden Risks, and Lifesaving Early Action

When it comes to children's health, what you don’t see can hurt. Hepatitis C in children often flies under the radar, presenting with no symptoms until the condition becomes serious. Here's what parents should know, straight from two experts in paediatric health.
What Hepatitis C Really Does?
According to Dr Anu K Vasu, Associate Consultant in the Department of Paediatric Gastroenterology, Hepatology and Liver Transplant at Kimshealth Trivandrum, “Hepatitis C infection can cause illness ranging from mild to severe.” While it may sometimes resolve on its own, she warns that it can become life-threatening, progressing to liver cirrhosis and even hepatocellular carcinoma.
“Clinical liver disease due to Hepatitis C is extremely rare in childhood unless they have risk factors like requiring repeated blood transfusions, chemotherapy, or immunotherapy,” Dr Rashmi Jeenakeri, Consultant Paediatrician and Neonatologist at Apollo Hospital, Seshadripuram, adds.
Also Read: Eating More Ultra-Processed Foods Linked to 41% Higher Lung Cancer Risk, Study
How Do Children Get Infected?
Dr Anu explains that “perinatal transmission (from infected mothers to newborns) is the predominant mode of HCV acquisition in young children.” However, it can also be transmitted via shared needles, unscreened blood transfusions, and even sexual contact.
Dr Rashmi further lists the ways children can become infected:
- Being born to a mother with Hepatitis C infection
- Receiving Hepatitis C-infected blood transfusion or organ transplantation
- Children on long-term kidney dialysis treatment
- Sharing personal hygiene items like toothbrushes or razors
Myths Busted: How Hepatitis C Does Not Spread
According to Dr Rashmi, parents can breathe a little easier knowing that Hepatitis C isn’t spread through:
- Air
- Broken skin
- Casual social contact like hugging or touching
- Breastfeeding
She stresses, “Children with Hepatitis C infection can participate in all normal childhood activities.”
Spotting the Silent Symptoms and Diagnosis
Most Hepatitis C infections in children are completely asymptomatic, says Dr Anu. Some may only show subtle signs like fatigue, muscle aches, poor weight gain, or abdominal bloating. Often, diagnosis happens incidentally during unrelated medical tests when elevated liver enzymes are spotted.
Dr Rashmi concurs: “Children with Hepatitis C infection usually do not have any symptoms or have mild flu-like symptoms.” However, she cautions that about 60-80 per cent may eventually show signs of chronic liver disease and, in rare cases, develop liver cancer.
Diagnosis, according to both experts, is through blood tests, either by detecting HCV antibodies or using PCR testing to find the viral RNA.
Why Screening Early Can Change the Game
Dr Anu stresses the importance of early detection: “All pregnant mothers should be screened for Hepatitis C viral infection.” If a mother is infected, her infant should be screened at six months via PCR testing or at 18 months using antibody tests.
She adds, “Children diagnosed with Hepatitis C infection should be followed up by a paediatric hepatologist to assess their eligibility for treatment by the age of 3 years.”
Treatment
While there is no vaccine for Hepatitis C, there is hope in the form of treatment. Dr Rashmi shares that “effective yet costly treatments are available which can cure up to 95 per cent of children.” Dr Anu recommends that all children above 3 years who are diagnosed should begin antiviral treatment to prevent long-term complications like chronic liver disease or liver cancer.
And in extreme cases? Dr Rashmi says, “Children with severe scarring of the liver need liver transplantation.”
Teenagers and Risky Behaviour
Dr Anu strongly advises on preventive education for adolescents. They should be taught about the dangers of needle sharing, getting tattoos or piercings in unregulated environments, and having unprotected sex. Parents, she says, “should be vigilant about the possibility of drug abuse among children and seek help from substance abuse treatment centres if necessary.”
Dr Rashmi adds that adolescents should avoid “getting tattoos, alcohol abuse, engaging in unprotected sex and sharing needles.”
Catch It Early, Act Fast
As Dr Anu says, early screening and timely treatment are crucial, not just for the child’s health but also to prevent the spread to others. And while symptoms may be silent, the long-term effects of ignoring Hepatitis C in children are anything but.
Ronald Acuña Jr. Sidelined with Achilles Tendon Tightness: What It Means and Why It Matters

It’s déjà vu Braves fans didn’t ask for. Ronald Acuña Jr., Atlanta’s powerhouse baseball outfielder and reigning National League MVP, has hit the injured list again, this time with tightness in his right Achilles tendon. Just months after returning from a torn ACL in his left knee, Acuña pulled up sore after sprinting the bases and later chasing a fly ball, exiting Tuesday’s game against the Royals mid-inning.
But what does Achilles tendon tightness actually mean, and why does it freak out athletes and sports doctors alike?
The Achilles tendon, also known as the calcaneal tendon, is the thick band of tissue that connects your calf muscles to your heel bone. It is the biggest and strongest tendon in the human body. But it can bring even the fittest athletes to their knees.
It helps you run, jump, pivot and push off the ground, basically every move an outfielder like Acuña makes in a single play. When it is tight, inflamed or partially torn, that springy propulsion becomes painful and unstable. Cue the limping, grimacing and, in some cases, weeks on the injured list.
Why Achilles Pain Is a Red Flag
Achilles tightness might sound like a minor complaint, but it is often the body’s early warning system. It could stem from overuse, fatigue, poor footwear, or biomechanical imbalances.In Acuña’s case, the discomfort reportedly began the night before while sprinting around the bases and got worse chasing fly balls. That is a classic setup: high-intensity bursts, sudden stops, and quick direction changes, all high-risk moves for the Achilles.
If ignored, tightness can escalate to tendonitis (inflammation), partial tears, or the dreaded rupture, which is basically the tendon snapping in two. That is a season-ending injury, often requiring surgery and months of rehab.
When the Body Says No
Beyond the physical pain, repeated injuries hit hard on the mental game. Acuña admitted he did not want to sit out, even though the pain intensified, because he has already missed too much time.But ignoring Achilles issues can backfire in the worst way. What starts as tightness today could be crutches tomorrow. The tendon does not heal fast, and re-injury is a very real risk if recovery is rushed.
The Game Plan for Recovery
For now, Acuña’s been placed on the 10-day injured list, but tendon issues do not always follow a schedule. He will likely undergo scans to rule out structural damage, followed by rest, anti-inflammatories, and physical therapy to stretch and strengthen the area.Recovery is not just about waiting for the pain to stop; it is about rebuilding strength, restoring flexibility, and ensuring both legs are balanced and strong.
Why This Matters for Everyone Who Plays
This is not just a pro-athlete problem. Achilles injuries are surprisingly common in runners, dancers, and gym-goers. If you feel stiffness in your heel or lower calf, especially first thing in the morning or during exercise, do not brush it off.Stretch regularly, warm up before activity, avoid sudden ramp-ups in intensity, and listen to your body. And if the pain lingers or worsens, see a specialist. Ronald Acuña Jr.’s Achilles flare-up might just be tightness, but it is the kind of tightness that turns trainers serious and fans anxious. It’s also a timely reminder that this tendon is small but mighty, and when it acts up, rest is not optional. Whether you are chasing fly balls or your morning run goal, treat your heels with the caution they deserve.
Manhattan Shooter Cited CTE in Suicide Note: Here Is What the Condition Means
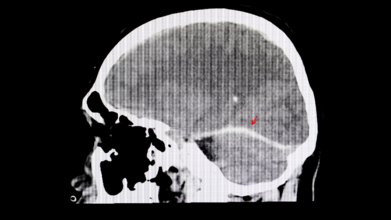
A recent tragic shooting in Midtown Manhattan has pulled an obscure but alarming brain disease back into the headlines. The shooter reportedly left behind a suicide note claiming he suffered from CTE, short for chronic traumatic encephalopathy, a condition linked to repeated head trauma. As shocking as the incident was, it has opened up a floodgate of questions: What exactly is CTE? Can it really make someone act out violently? And how can we even know if someone had it?
What Exactly Is CTE?
CTE is not your everyday concussion aftermath. It is a progressive, degenerative brain disease caused by repeated head injuries, the kind you get from rough contact sports, military service, or just too many unfortunate falls. Over time, these impacts seem to trigger the buildup of an abnormal protein in the brain called tau. This sticky substance does not just sit there quietly. It gradually spreads through the brain, messing with vital functions and causing serious, irreversible damage.The Symptoms
People with CTE do not wake up one morning knowing something is wrong. The symptoms can creep in slowly, subtle at first, then increasingly hard to ignore, leading to memory lapses, confusion, impulsive behaviour, unexplained aggression, mood swings, deepening depression and, in many tragic cases, suicidal thoughts.It is the sort of change that can feel like a personality transplant. Loved ones often report seeing someone “become a different person” over time.
Not Just a Pro Athlete Problem
For a long time, CTE seemed to be the unwanted souvenir of retired American football players. The sport's culture of full-body collisions made it the perfect storm for head trauma. But recent research is telling a more disturbing story. A 2023 study uncovered CTE in younger, amateur athletes, including teens as young as 17.Back to the Manhattan case. While the shooter’s note mentioned CTE, we still do not know whether he actually had it, let alone whether it influenced his behaviour. This brings up messy territory: should possible brain disease be considered in criminal responsibility? Can CTE be a mitigating factor in violent crime?
It is a grey zone. And until we develop reliable tools to diagnose CTE in the living, we are mostly left guessing.
What Can We Do?
CTE is a slow, silent thief, robbing people of their memory, emotions, and identity. And while scientists are racing to understand it better, prevention remains our best bet for now. That means:- Rethinking how we approach youth and professional sports
- Reducing repeated head trauma wherever possible
- Keeping an eye out for changes in behaviour following head injuries
What Is That One Thing That Makes Hepatitis So Dangerous?

Hepatitis is not nicknamed the “silent killer” for nothing. What makes it so dangerous is how symptomless it often is for years. It can quietly chip away at your liver without so much as a warning sign. By the time symptoms like fatigue, jaundice, or abdominal pain appear, significant harm may already have occurred. This eerie silence allows hepatitis to go undetected until it has done some serious damage.
Just Because You Cannot Hear It Does Not Mean It Is Not There
Dr Vikram Vora says that hepatitis is a major global health threat, killing over a million people each year. What is even more tragic? These deaths are, in his words, “largely preventable”. The villains in this tale, cirrhosis and liver cancer, often stem from untreated or undiagnosed hepatitis infections.
Prevention Helps
“The cornerstone of hepatitis control is prevention,” Dr Vora says. And the good news is that you have got some powerful tools at your disposal. “Vaccination, especially against Hepatitis B, is one of the most effective tools available,” he says, adding that infants, healthcare workers, and at-risk adults should be prioritised. Other prevention measures include safe injection practices, steering clear of needle-sharing, and ensuring blood transfusions are properly screened.
But danger often hides in plain sight. Dr Vora warns that something as seemingly harmless as getting a tattoo or piercing can carry lifelong consequences if done in an unregulated facility. His advice? “Choosing safe, licensed establishments is non-negotiable.”
Why You Should Not Wait for Symptoms
If there is one thing hepatitis is good at, it is staying undetected. That is why Dr Vora champions regular screening, especially if you have had medical procedures, blood transfusions, or close contact with someone infected. “Early diagnosis is a game-changer,” he says. Caught in time, hepatitis can be treated effectively, helping patients avoid severe liver disease or even make a full recovery.
A Diagnosis Is Not a Death Sentence
Dr Vora offers hope to those living with hepatitis. “With proper medical care and lifestyle adjustments, a healthy life is achievable,” he insists. That means ditching alcohol, sticking to a balanced diet, maintaining a healthy weight, and closely following medical advice. He also points out the mental and emotional toll a diagnosis can take. “Support from family, community, and healthcare providers can make a significant difference in outcomes.”
The Stigma That Silences
Perhaps just as damaging as the virus itself is the social stigma surrounding it. Dr Vora identifies this as a major hurdle in tackling hepatitis. “Fear of social exclusion keeps many from seeking help,” he explains. And that delay can cost lives. According to him, building a culture of empathy and understanding is critical. He encourages public health campaigns, education, and open dialogue as essential tools to dismantle this stigma.
Make Noise Against the Silence
In Dr Vora’s words, “Hepatitis may be silent, but it is not invincible.” Every little step, whether it is getting vaccinated, getting screened, or just talking about it, can chip away at the power hepatitis holds. Silence has cost too many lives already. Awareness can save them.
© 2024 Bennett, Coleman & Company Limited

