- Health Conditions A-Z
- Health & Wellness
- Nutrition
- Fitness
- Health News
- Ayurveda
- Videos
- Medicine A-Z
- Parenting
- Web Stories
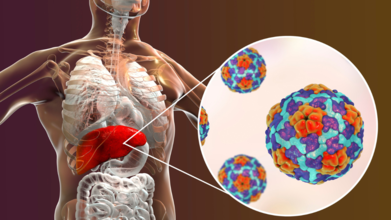
Hepatitis Day 2025: Is Hepatitis On A Decline Or Still A Cause Of Concern?
Credits: Canva
On World Hepatitis Day today, the spotlight is on one of the most misunderstood but critical public health challenges, viral hepatitis. Observed annually on July 28, this global awareness day focuses on liver inflammation that can silently progress into liver cirrhosis or cancer.
This year’s theme, “Hepatitis: Let’s Break It Down,” urges dismantling financial, social, and systemic barriers that prevent people from seeking testing, vaccination, and treatment.
The World Health Organization (WHO) continues to call for unified action to eliminate hepatitis as a public health threat by 2030.
Also Read: 5 Surprisingly Easy Things You Can Do Daily to Start Reversing Fatty Liver
But how far have we come in achieving that goal? A look at the data and expert insights reveals a mixed picture.
Hepatitis A on the Rise Among Adults
Traditionally associated with childhood jaundice, hepatitis A is now emerging as a more serious threat, especially in urban adults. Doctors in Mumbai report a rise in severe adult hepatitis A cases, including complications like liver failure. As hygiene standards improved in metros, fewer people were exposed to the virus in early childhood, leaving them without natural immunity. This means adults now face more aggressive symptoms when exposed through contaminated food or water, often during the monsoon season.
Pregnant women, too, are being impacted. In one case, a woman admitted for what appeared to be morning sickness was found to have hepatitis A. Doctors emphasize that hepatitis A can affect both mother and baby, and early diagnosis is crucial.
Hepatitis C Cases Drop Thanks to Free Treatment
There is, however, good news when it comes to hepatitis C. Since 2018, India’s National Viral Hepatitis Control Programme has made direct-acting antiviral treatments freely available. These drugs offer a full cure in just three months. As a result, new hepatitis C infections have declined significantly in both public and private hospitals.
In Maharashtra alone, over 28 lakh people were tested for hepatitis C in 2024-2025, out of which 9,476 tested positive. More than 2,000 people were started on treatment. Compared to 1,339 reported cases in 2021-2022, this rise in diagnosis doesn’t necessarily indicate more infections — instead, it reflects better testing and surveillance. Experts credit this progress to improved blood screening protocols and increased awareness around the dangers of needle sharing.
Hepatitis B Still a Serious Threat
Despite medical advancements, hepatitis B remains a major concern. Often referred to as one of the most infectious viruses, it affects millions and is known for its ability to stay dormant and reactivate. While it isn’t curable yet, it is manageable with long-term antiviral therapy. Unfortunately, lack of early symptoms means many people are diagnosed only when serious liver damage has already occurred.
Data from Maharashtra shows an alarming increase in hepatitis B cases, from 9,000 in 2021-2022 to 65,000 last year. This includes 23,000 pregnant women, highlighting the virus’s continued prevalence and risk of mother-to-child transmission. In some cases, patients have even required liver transplants due to delayed diagnosis and treatment.
Testing and Vaccination Are the Need of the Hour
Advances in diagnostics are changing the game. Portable machines like Truenat are making it easier to test for hepatitis viruses in remote areas. Maharashtra saw a 150% rise in hepatitis B testing and a fivefold increase in hepatitis C testing from 2023-24 to 2024-25. The central government is reportedly planning to install Truenat machines in all 40,000 primary health centres across the country in the next two years.
Vaccines for hepatitis A and B are available and effective, yet coverage remains uneven. Experts strongly advise vaccination for high-risk individuals and routine screening for hepatitis B surface antigen (HBsAg) and anti-HCV antibodies. These simple blood tests can be lifesaving when followed up with further tests to assess viral load.
Dr. Somnath Mukherjee, gastroenterologist at CMRI Kolkata, points out that hepatitis continues to be “one of the least understood global health challenges”, despite being preventable, treatable, and in some cases, curable.
He emphasizes the need to dismantle ignorance and stigma around testing and treatment. “World Hepatitis Day provides an opportunity to simplify awareness and dismantle barriers to infection awareness and elimination,” he says. His message is clear: Get tested. Get treated. Get protected.
Hepatitis 101
Hepatitis, caused by viruses labeled A through E, can often go unnoticed until significant liver damage has occurred. “Hepatitis B and C are the most dangerous,” explains Dr. Somnath Mukherjee, noting that these infections can silently progress to liver failure, cirrhosis, or even liver cancer if untreated.
While Hepatitis A and E typically spread through contaminated food or water—often in areas with poor sanitation—B and C are more commonly transmitted via unsafe blood transfusions, shared needles, or unprotected sex.
Symptoms, if they appear at all, might include fatigue, jaundice, dark urine, pale stools, abdominal swelling, or itching. “Waiting for symptoms is pointless,” he stresses, as most infections are asymptomatic.
The good news, however, is that hepatitis is preventable and treatable. Vaccines are available for Hepatitis A and B, and Hepatitis C is now curable with a three-month oral medication.
Though Hepatitis B isn’t curable yet, it is manageable with antiviral drugs. “Screening is crucial,” says Dr. Mukherjee, recommending simple blood tests like the Hepatitis B surface antigen (HBsAg) and Anti-HCV antibody, especially for those at higher risk.
College Student Beats Breast Cancer By Lifting Through Recovery - How Active Recovery Helped Her Treatment

(Credit-Miller School of Medicine)
‘Fight through cancer’, ‘you can’t let cancer kick you down’ are things survivors and people who have had recent cancer diagnosis. While it is a good sentiment, one must understand that cancer is difficult a difficult process to go through. However, this young college student did not let this stop her.
LaShae Rolle, a 27-year-old competitive powerlifter, can squat a massive 441 pounds, bench press 292 pounds, and deadlift 497 pounds. Last year, breast cancer threatened her dreams of competing against the best. But Rolle didn't let it stop her. She powered through her cancer treatment, maintaining an intense strength training program all along. And then, she wrote a study about her experience.
Lifting Through Treatment
Rolle, who is studying public health sciences at the University of Miami, became the subject of her own unique study. She documented her journey of elite-level strength training while undergoing chemotherapy, a mastectomy (breast removal surgery), and radiation.
Her study, published in the journal Lifestyle Medicine, challenges the common belief that cancer patients should only do low or moderate exercise. Rolle explained that strength training was key to her identity as an athlete and researcher. During her cancer journey, it helped her feel connected to herself and in control of her body and mind.
By the end of her treatment, Rolle had managed to keep almost all the strength she had before her cancer diagnosis. She proudly stated that she kept going, adapting her workouts around her chemotherapy cycles to train safely. This physical activity gave her a sense of normalcy when everything else felt uncertain.
Why This Research Matters
Previous studies have shown that moderate exercise can help cancer patients by reducing tiredness, improving physical ability, and easing treatment side effects. However, that research usually focused on average people doing regular workouts, not elite athletes trying to maintain high-intensity efforts during treatment.
In the Miller School of Medicine news release, Tracy Crane, a director at the University of Miami's Sylvester Comprehensive Cancer Center and Rolle's mentor, emphasized that Rolle's story is a powerful reminder that recovery from cancer isn't just about getting better; it's about regaining strength, identity, and purpose. She added that Rolle's commitment to powerlifting shows how movement can be a way to heal, empower, and advocate for oneself.
Rolle's Training Plan and Impressive Results
Rolle was diagnosed with stage 2B breast cancer in 2024. Her cancer was fueled by female hormones, and she didn't have a genetic link to the disease. Her colleagues at the University of Miami helped her create a strength training plan that fit around her chemotherapy schedule:
- High-intensity days were planned before her chemo sessions, focusing on squats, bench press, and deadlifts.
- Moderate days between chemo cycles included exercises like rows and shoulder presses.
- Recovery days immediately after chemo involved light movement and therapy.
By the end of her treatment, Rolle had retained an incredible 93% of her squat strength and 87% of her bench press and deadlift strength. These are remarkable numbers for someone going through chemotherapy. Rolle kept herself accountable by documenting everything with videos and in a training diary, which reminded her of her ongoing strength. She expressed amazement looking back at videos of herself lifting over 400 pounds while on chemotherapy.
Researchers note that these specific findings mainly apply to elite athletes who already have a background in high-intensity training, rather than the average cancer patient. However, Rolle believes her study highlights the importance of creating treatment plans tailored to each patient's needs. She is motivated to continue lifting and to advocate for evidence-based exercise as a key part of cancer care.
Grieving The Loss Of A Loved One Too Intensely Can Double The Risk Of Early Death

Grieving is different for everyone; some people grieve in private, while others grieve by sharing their love and stories with others. It is a natural process one goes through after a loss. While you are eventually expected to move on and find peace with the absence, it isn’t easy for many. Some people grieve for years and others spend their lifetimes looking for peace after the loss.
A new study reveals that people experiencing very strong grief after losing a loved one are almost twice as likely to die within ten years of that loss. This means their chances of dying early increase by 88%.
Long-Term Impact of Grief
The study, published in Frontiers in Public Health, looked at how grief affects people over a decade. It found that those with consistently high levels of grief in the first few years after a loss were not only more likely to die sooner but also:
- Nearly three times more likely to get mental health care, like talk therapy.
- Over five times more likely to be prescribed antidepressants.
- More than twice as likely to be given sedatives or anti-anxiety medications.
Researchers followed over 1,700 grieving men and women in Denmark. Their average age was 62. Most of them (66%) had lost their partner, 27% had lost a parent, and 7% had lost another close person.
Participants answered questions about their grief levels over the first three years after their loss. The study found that about 6% of people had very high grief that didn't lessen over time. In contrast, 38% had consistently low grief, and 47% experienced strong or moderate grief at first, which then slowly decreased.
How Does Grief Imapct Our Body?
According to the US National Institute of Aging, grief can affect you both physically and emotionally. As time goes by, you'll still miss your loved one, but for most people, the intense pain will slowly fade. You'll have good days and bad days. It's important to remember that feeling surprised or even guilty for laughing or enjoying time with friends is a common part of the grieving process. It's common to cry easily and experience things like:
- Trouble sleeping
- Lack of interest in food
- Difficulty concentrating
- Problems making decisions
Why Does Intense Grief Affect Mortality?
While the study clearly shows a link between strong, ongoing grief and an increased risk of early death, researchers aren't entirely sure why. Researchers mentioned that past research found connections between high grief and higher rates of heart disease, mental health problems, and even suicide, but more investigation is needed into the link with early death.
However, the study did offer a clue: people in the "high grief" group were more likely to have prescriptions for mental health conditions even before their loved one passed away. This suggests they might have been more emotionally vulnerable, making the loss even harder to cope with. They explained that these individuals also generally had less education.
What Does Intense Grief Mean?
It's normal to feel sad, numb, or lost for a while after a death. However, for some, grief can become so long-lasting or distressing that it turns into something unhealthy, known as complicated grief. People with this condition might struggle to understand or accept the loss, experience intense and ongoing sadness, and find it hard to get back to their daily life or plan for the future. Other signs include being overwhelmed by negative emotions, constantly thinking about the person who died or how they died, and feeling a lack of meaning or purpose in life.
Identifying Those at Risk
Complicated grief is a serious condition that may require extra help. If your sadness is making it difficult to live your daily life, please know that help is available. You can reach out to a support group, a mental health professional, or trusted loved ones. If cost is a concern, ask your doctor or healthcare provider about local programs or professionals who offer affordable or free help.
Doctors might be able to identify people at risk for severe and prolonged grief by looking for previous signs of depression or other serious mental health conditions. If a doctor spots these signs, they can offer specific support, such as tailored follow-up appointments, referrals to therapists, or dedicated grief counseling. This proactive approach could help those most vulnerable navigate their grief and potentially improve their long-term health outcomes.
PTSD In Combat Veterans Could Be Treated With This African Drug - Study Finds

(Credit-Canva)
Being in the military means you may witness things or be involved in combat or missions that are life-threatening and horrible to deal with. There are accidents, training injuries, or difficult situations that place them under immense stress. All of these things lead to PTSD, or post-traumatic stress disorder. According to the US National Center for PTSD, at some point in their lives, 7 out of 100 veterans will have PTSD. This number increases to 13 for the female veterans. Dealing with this can take a lifetime, with them experiencing symptoms for years.
Combat veterans also often struggle with anxiety, and depression after experiencing traumatic brain injuries (TBI). These struggles can leave them feeling hopeless and even suicidal. However, a surprising new treatment might offer hope: a psychedelic drug called ibogaine.
How Ibogaine Might Help
Ibogaine comes from the roots of an African shrub. A recent study, published in Nature Mental Health, suggests that this drug can safely and effectively treat the long-term effects of TBI in veterans. Thirty veterans took part in the study, traveling to Mexico for the treatment because ibogaine is not legal in the U.S.
Researchers discovered that ibogaine changes brain activity in ways that can reduce stress and help veterans better deal with their past trauma. A lead researcher from Stanford Medicine noted that no other drug has been able to ease the brain and mental health symptoms of TBI in this way. He called the results "dramatic" and plans to study the compound further.
What Ibogaine Is?
People who take ibogaine often say the experience is like a "waking dream," where they think about memories and see strong images. This compound is used in African religious ceremonies and has also been looked at as a possible treatment for depression and to help people overcome drug addiction.
Journey to Mexico and Positive Outcomes
For this study, researchers worked with a small group of 30 special operations veterans. These veterans had lasting symptoms from TBIs and had been exposed to many explosions. The veterans chose to receive ibogaine treatment at a clinic in Mexico on their own. The clinic gave them ibogaine by mouth, with medical supervision. They also received a dose of magnesium, which helps prevent heart problems sometimes linked to the drug.
Before the treatment, doctors from Stanford checked the veterans. Many had PTSD, anxiety, or issues with alcohol. About half had thought about suicide at some point, and some had even attempted it. Within just one month of ibogaine treatment, the improvements were significant:
- PTSD symptoms dropped by 88%
- Depression symptoms dropped by 87%
- Anxiety symptoms dropped by 81%
The veterans also reported less disability and better focus, thinking skills, memory, and impulse control. Another veteran in the study, who served in the U.S. Navy for 27 years, shared that his thinking abilities were "fully restored" after ibogaine, which helped him at work and improved his family life.
How Ibogaine Changes the Brain
Brain scans helped researchers understand why the drug might be effective. Veterans whose planning and organizing skills improved after treatment showed an increase in certain brain waves called theta rhythms. Stronger theta rhythms might help the brain adapt and be more flexible. Similarly, those with fewer PTSD symptoms showed less complicated brain activity, suggesting the drug helps calm the intense stress response associated with PTSD. These brain scans might also help doctors find out which patients would benefit most from ibogaine.
The study reported no serious side effects, and no heart problems occurred. Veterans did mention typical symptoms like headaches and nausea during treatment.
Partly because of these positive findings, Texas recently approved a $50 million plan to fund more studies of ibogaine. This program will help match private money for ibogaine trials, which could lead to the drug being approved by the U.S. Food and Drug Administration (FDA).
Researchers believe ibogaine could become a broader drug for brain recovery. They think it works on unique brain pathways and could help us better understand how to treat other forms of PTSD, anxiety, and depression that aren't necessarily connected to TBI.
© 2024 Bennett, Coleman & Company Limited

