- Health Conditions A-Z
- Health & Wellness
- Nutrition
- Fitness
- Health News
- Ayurveda
- Videos
- Medicine A-Z
- Parenting
How Often 'Or Not' Is Hormone Therapy Prescribed?

Only .1% children, aged between 8 and 17 who identify as transgender or gender-diverse are prescribed gender-afforming hormones or puberty blockers as per the study done by researchers at the Harvard University and FOLX Health, a healthcare provider for the LGBTQ+ community. This report was published in the JAMA Pediatrics, which analyzed 5 million private insurance claims filed between 2018 and 2022.
This is onset of the public uproar over teenagers and children changing their genders, transgender teenagers and children rarely getting the prescribed gender-affirming medication. The lead author Landon Hughes, a postdoctoral fellow at the university's school of public health said, "The politicization of gender-affirming care for transgender youth has been driven by a narrative that millions of children are using hormones and that this type of care is too freely given. Our findings reveal that is not the case."
What do the findings mean?
The findings also highlighted that no patients under 12 had received the gender-affirming hormones and higher rates of puberty blockers were prescribed for patients assigned female at birth.
Why is that the case?
This happens mostly in the condition called the 5-Alpha Reductace Deficiency. When the baby is in the fetus, the genital areas of both males and females remain the same. During the development of the genital, in such cases, the phallus does not full elongate and resembles something in between a clitoris and a penis head. The scrotum also remains split in two and urethral opening remains on the underside of the penis. The genetalia does not look male or female, however, due to non-fusion of the scrotum and urethral opening, the child is often assigned female at birth. Which could be one of the reasons why higher rates of puberty blockers were prescribed for patients assigned female at birth.
What the data says?
About 3.3% of US high school students identify as transgenders and an additional 2.2% have questioned if they were at the same point, as per the latest annual Youth Risk Behavior Survey conducted by the Centers for Disease Control and Prevention.
What do puberty blockers do?
Puberty blockers which were originally approved for children whose sexual development occurs too soon are now prescribed to delay the onset of puberty or to pause for those who do not identify with their assigned birth. These are called GnRH agonists, which stops the body from making hormones, such as testosterone and estrogen.
In individuals assigned male at birth, it slows down the growth of facial and body hairs and also prevents voice deepening and limits the growth of sex organs. Whereas in individual assigned female at birth, it limits breast development and stops menstruation.
Delaying puberty in transgender allows them more time to explore and integrate their identity. This is also helpful for those who experience gender dysphoria. It is a condition that describes a sense of unease that a person may have because of a mismatch between their biological sex and their gender identity. As per the National Health Service (NHS) UK, "Most people identify as "male" or "female". These are sometimes called "binary" identities. However, some people feel their gender identity is different from their biological sex. For example, some people may have male genitals and facial hair but do not identify as a male or feel masculine."
36% Of Rabies Death Comes From India: This Is What You Should Do After A Dog Bite, Explains Doctor

Credits: iStock
The World Health Organization (WHO), notes that 36% of world's rabies deaths come from India, and a 2024 Lancet study notes that the country accounts for over one-third of global rabies deaths. When we spoke to Dr Aniket Mule, Consultant Internal Medicine at KIMS Hospital, Thane, he said that it is not just dog bites that lead to rabies, but it could happen from any rabies-susceptible animal. The first line of defense after you clear your wound immediately is to get the rabies vaccine. "Rabies vaccination is required for bites or scratches from any rabies-susceptible animal, including cats, monkeys, bats, foxes, and other wild mammals," he pointed out. As the country's apex court ruled and issued directives on stray dogs, focusing on public safety by ordering their removal, global health organizations, including WHO point out that this is not the right way to deal with rabies issue. Comprehensive methods including evidence=based strategies that center on mass dog vaccination is the key to the problem.
However, before this could be implemented, here's what you should know about dog bites and rabies.
What To Do After A Dog Bites Or Scratches You?
Dr Mule points out that even when there are minor scratches, without bleeding, you must get a rabies shot. "Rabies can be contracted through broken skin. Such exposures still require medical evaluation and, in most cases, rabies vaccination."
Read: In An 'Exceptionally Rare' Case, Man Dies Of Rabies After Kidney Transplant
What Should One Do Immediately After Being Bitten Or Scratched?
- Wash the wound immediately for at least 15 minutes with soap and running water
- Apply an antiseptic such as povidone-iodine
- Do not apply home remedies like turmeric, chili or oil
- Seek medical care promptly for rabies vaccination and possible immunoglobin
Dr Mule points out that the rabies vaccine should be started as soon as possible. "Ideally within 24 hours of a bite or scratch. However, even if there is a delay of days or weeks, vaccination should still be started immediately as rabies has a variable incubation period," he says.
After the bite, the immediate medical attention involves rabies post-exposure prophylaxis or PEP, and with a tetanus booster. Some rabies vaccines also use saline water as the diluent to reconstitute the freeze-dried powder before injection.
Read: Australia Issues Advisory Warning Travelers Of Counterfeit Rabies Vaccines Found In India
The temperature of the vaccine matters. "Rabies vaccines are temperature-sensitive and must be stored between 2°C and 8°C. Exposure to heat or freezing can reduce vaccine potency. Poor cold-chain maintenance is a known reason for vaccine failure in rare cases," points out the doctor.
Cases Of Rabies Coming Back After Vaccination Course Has Been Done
Dr Mule points out that in order to avoid such things happening, one must ensure immediate wound washing, timely vaccination, and correct use of Rabies Immunoglobulin or RIG. Rabies can come back if these following things occur:
- Delay in starting vaccination
- Failure to administer Rabies Immunoglobulin (RIG) in severe (Category III) exposures
- Improper wound cleaning
- Incorrect injection site (gluteal region)
- Poor vaccine storage (cold-chain failure)
Dr Mule points out that the vaccine should be given intramuscularly in the deltoid or upper arms for adults, as gluteal or buttock injections could lead to inadequate absorption and reduce effectiveness.
How Many Doses Should One Get?
- For someone not previously vaccinated, the current standard is 4 doses on days 0, 3, 7, and 14 (intramuscular schedule).
- In some government programs or intradermal schedules, 3–4 doses may be advised.
- Previously vaccinated individuals require only 2 booster doses (days 0 and 3).
The exact schedule depends on vaccination history and the protocol followed.
Five Essential Health Tests to Consider This Winter, According To A Doctor

Credits: iStock
Winter in India is often associated with sardio ke laddoo, but also with increasingly sedentary lifestyle, worsening air pollution, all of which leads to more time spending home than to going out, taking a stroll, working out and more. This is why as winter sets in, India also sees a quiet but consistent rise in non communicable diseases, or NCDs, conditions that now account for nearly two thirds of all deaths in the country. Heart disease, diabetes, thyroid disorders, fatty liver disease and arthritis continue to rise across age groups, driven by sedentary lifestyles, dietary excess and delayed diagnosis.
Winter can further aggravate these risks. Physical activity drops, calorie dense foods become routine, sunlight exposure reduces and metabolism changes. Studies and hospital data in India have repeatedly shown that heart attacks and strokes tend to spike during colder months. Blood vessels constrict, blood viscosity increases and cholesterol levels often rise. Blood sugar control also becomes more challenging, while joint pain and stiffness worsen for many.
Dr. Mayanka Lodha Seth, Chief Pathologist at Redcliffe Labs, says the problem is not seasonal food but seasonal neglect. “Traditional winter foods are not harmful on their own. The real risk comes from consuming them without understanding what is happening inside the body,” she explains. “Winter tends to mask symptoms while quietly worsening internal imbalances.”
With India already home to over 100 million people living with diabetes and a similar number estimated to be prediabetic, preventive testing becomes crucial. Doctors recommend five key tests that can offer a clearer picture of health before winter indulgence begins.
Blood Sugar Levels
Diabetes is one of the fastest growing NCDs in India, and a large proportion of cases remain undiagnosed. Winter diets high in sugar and fat can trigger frequent glucose spikes. Testing fasting blood sugar and HbA1c helps identify early risk and prevents long term complications affecting nerves, kidneys and the heart.
Lipid Profile
High cholesterol is a major contributor to cardiovascular disease, which remains India’s leading cause of death. Reduced activity in winter often pushes lipid levels higher. A lipid profile helps assess heart risk and guides dietary and lifestyle moderation before damage sets in.
Liver Function Test
Non alcoholic fatty liver disease is increasingly common in India, even among younger adults. Excess sugar and fat intake during winter can worsen liver fat accumulation. Early liver testing can flag reversible changes before they progress to chronic liver disease.
Thyroid Function Test
Thyroid disorders affect millions in India, especially women, and often go unnoticed. Symptoms like weight gain, fatigue and cold intolerance are frequently brushed off as winter sluggishness. A simple thyroid test helps distinguish seasonal lethargy from hormonal imbalance.
Vitamin D and Vitamin B12 Levels
Vitamin D deficiency is widespread due to limited sun exposure in winter, while Vitamin B12 deficiency remains common because of dietary patterns. Both deficiencies are linked to low immunity, muscle pain, bone weakness and worsening joint discomfort.
Dr. Seth adds, “Preventive diagnostic testing allows people to make informed choices. It helps them enjoy winter foods in moderation without unknowingly worsening an underlying condition.”
As NCD related healthcare costs continue to rise in India, early testing offers both health and financial protection. Winter comfort does not have to come at the cost of long term health. Staying informed may be the most effective preventive step this season.
Tamiflu Isn't The Only Flu Medicine, Expert Shares Other Alternative
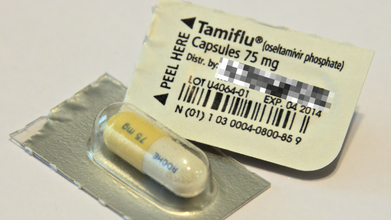
Credits: iStock
Flu season is hitting hard this year, and the symptoms could feel relentless. People are suffering from rising fever, hacking cough, blocked and stuffy nose and sore throat. While many people get relief from Tamiflu, which is a prescribed antiviral medication that is used to treat or even to prevent illness, there are other alternatives available too.
Dr Ari Brown, a Texas based pediatrician and the author of Baby411 book series told CNN health that one of the most common complaints that she gets to hear from Tamiflu is vomiting. A 2023 study published in the Pediatric Infectious Disease Journal notes that 18% of people experienced vomiting with Tamiflu, as compared to 5% with Xofluza, an alternative.
“I’ve also had a few pediatric patients experience moodiness with Tamiflu, which is reported in the literature,” she said.
Read: Adenovirus Cases Rise In UK, Health Authorities On Alert
Tamiflu is usually gives to treat flu in people ages 2 weeks and older and to reduce the chance of getting the flu in people 1 year and older. The medicine could be administered in both form, liquid and capsules and usually taken twice daily for five days straight. This is prescribed for when flu is to be treated. However, when used for prevention, it is typically taken once for 10 days.
What Are The Other Alternatives Available For Flu Treatment?
Xofluza: It is administered as a single dose tablet and is approved for ages 5 and older. This medicine can also be used to treat or to prevent the flu. While it costs nearly $200 for those without insurance, eligible patients can use coupons to lessen costs. Dr Brown points out that this medicine could have side effects like diarrhea and vomiting. However, the study aforementioned notes that for this, only 5% patients had vomiting symptoms, when compared with Tamiflu.
Dr Brown also said that Xofluza can stop viral shedding in one day, while Tamiflu could take up to three days. "Both antivirals will help reduce the duration of misery by couple of days," she pointed out.
Dr Brown also pointed out that overall, "Xofluza is rising in popularity over Tamiflu." “One dose. Fewer side effects. More insurances are covering the cost of it now and manufacturer coupon makes it less expensive than in previous years," she said.
Rapivab: This is another prescribed medication that is approved to treat flu. This could be administered for people ages 6 months and older. It has to be given by a health care provider, as it is given once as an intravenous infusion. It could cost up to $1,000 without insurance and most common reaction in adults is diarrhea.
Relenza: This flu medication is inhaled in powder form. It is administered through an inhaler device, which is to be used twice a day for five days straight. The prescribed drug is approved to treat flu in ages 7 and older and for preventative use, in ages 5 and older. It could cost about $90 without insurance.
It may have side effects like dizziness, allergic reaction, or irritation of the nose. It is not recommended for people who have breathing issues or have asthma.
© 2024 Bennett, Coleman & Company Limited

