- Health Conditions A-Z
- Health & Wellness
- Nutrition
- Fitness
- Health News
- Ayurveda
- Videos
- Medicine A-Z
- Parenting
- Web Stories
'I Broke Up With My Friend Because She Cancelled Lunch'- How BPD Turned A Simple No-Show Into Abandonment

Image Credit: Freepik
I wanted to reject the label. The term personality disorder felt heavy, almost damning. But as my therapist explained the cycles of fear, abandonment, and emotional intensity, I felt something shift inside me. It wasn’t just me overreacting. It wasn’t just me being too much. There was a reason my friendships, my jobs, my relationships always seemed to spiral. There was a reason I felt devastated when my best friend canceled lunch. And now, I had to figure out what that meant.
Tracey* had always felt out of place in most conversations with her friends and at work, when people had it all together (and so did she), it was just a battle in her mind. She had been in therapy for a year before her diagnosis of Borderline Personality Disorder (BPD). Owing to a the stigma with mental health, most people assume BPD to be a serious disorder with hospitalization or drastic shifts in emotions.
Borderline personality disorder (BPD) is more than just mood swings or impulsivity. It’s a relentless cycle of intense emotions, fear of abandonment, and self-doubt. To those who don’t live with it, their reactions can seem irrational, even extreme. To them, they feel like survival.
In an honest conversation about her diagnosis and experiences, Tracey shares how it felt when a simple lunch with a close friend got cancelled and all she could feel was, 'worthless'.
When my friend canceled lunch, I spiraled. Logically, I knew things came up. People got busy. Plans changed. But in that moment, it didn’t feel like a simple schedule conflict. It felt like rejection. It felt like she didn’t care. It felt like proof that I wasn’t important.
BPD warps everyday interactions, turning them into battlegrounds of self-worth. A delayed text reply can feel like being ignored. A shift in tone can signal impending abandonment. And when these emotions hit, they hit like a tidal wave—sudden, overwhelming, and consuming.
This emotional intensity has shaped my life in ways I never fully understood until my diagnosis. I’ve lost jobs because I lashed out at perceived slights. I’ve walked away from relationships over a single disagreement, convinced the other person secretly resented me. I’ve felt the highest highs of love and connection, only to be plunged into despair at the first sign of distance.
It’s not that I want to feel this way. If I could switch it off, I would. But BPD doesn’t give you that choice.
Daily Challenges of Living with BPD
One of the hallmarks of BPD is an intense fear of abandonment. This fear isn’t just about being alone; it’s about the overwhelming certainty that people will leave—and that when they do, it will be devastating.
When my friend texted, “Hey, I need to reschedule,” I didn’t read it as a simple change of plans. My mind raced: She doesn’t want to see me. I must have done something wrong. She’s pulling away.
I fought the urge to lash out. I wanted to tell her, Forget it. Don’t bother rescheduling. I wanted to cut her off before she could abandon me first. Instead, I sat with the discomfort. I reminded myself that her cancellation wasn’t proof of rejection. I tried to believe it.
BPD makes these moments feel like life or death, but therapy has helped me recognize the difference between feeling abandoned and actually being abandoned.
Black-and-White Thinking: No Room for Gray Areas
Another struggle is the tendency to see things in extremes. People are either good or bad. A relationship is either perfect or ruined. There is no in-between.
When my friend canceled lunch, I immediately shifted her from “amazing friend” to “someone who doesn’t care.” My brain didn’t allow for the possibility that she was just busy, that her cancelation had nothing to do with me.
This kind of thinking has led me to destroy relationships over minor misunderstandings. It’s something I’m working on—learning to challenge absolutes, to recognize nuance, to remind myself that people can be flawed and still love me.
Healing Is a Journey, Not a Destination
Borderline personality disorder doesn’t just disappear with a diagnosis. It’s something I have to manage every single day. Therapy, medication, mindfulness—these tools help, but they don’t erase the struggles.
What I’ve learned, though, is that I can have meaningful relationships. I can learn to sit with discomfort. I can remind myself that a canceled lunch is just that—a canceled lunch.
There are still days when the fear creeps in, when I feel unworthy, when I want to push people away before they can hurt me. But I’m learning to stay. To trust. To believe that not every no-show is abandonment.
BPD might shape how I experience the world, but it doesn’t have to define me. And maybe, just maybe, that’s enough.
TV’s ‘Nicest Judge’ Frank Caprio Shares Heartbreaking Cancer Update: ‘Keep Me In Your Prayers’
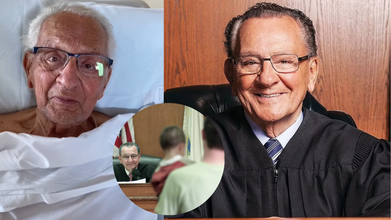
Credits: AP/Instagram@therealfrankcaprio
For over three decades, Judge Frank Caprio was hailed as "the world's kindest judge." From the bench of Providence Municipal Court, he warmed the hearts of millions with his compassion, impartiality, and uniquely human style of justice. With the Emmy-nominated series Caught in Providence, his moments of mercy went viral, transforming ordinary court appearances into acts of kindness that struck a chord that went far beyond the borders of Rhode Island.
Now, at age 88, the man famous for providing others with a second chance is grappling with his own greatest challenge: pancreatic cancer. And consistent with Caprio's style, he's confronting it with courage, humility, and a sincere plea for prayers.
For close to 40 years, Frank Caprio presided over hearings in Providence, Rhode Island, hearing everyday individuals frequently saddled by parking tickets, small infractions, and personal dilemmas. But in a departure from the most typical courtroom hearings, his remained chances for mercy.
He would waive fines for low-income families, tell jokes to calm worried defendants, and say that justice can be more than just punishment - it can also be compassion. His motto was straightforward, there is a human behind every case file.

That spirit made headlines around the world when Caught in Providence was broadcast. By 2017, videos of Caprio's moments in the courtroom went viral, garnering more than 15 million views on the internet. To many, he was a symbol of compassion within an otherwise brutal system.
Frank Caprio's Health Setback That Shook His Fans
In 2023, Caprio announced that he had been diagnosed with pancreatic cancer, the most aggressive type of the disease. In spite of the bleak prognosis attached to this diagnosis, he finished undergoing radiation treatments in 2024 and posted optimistic reports, even publishing a new book.
But in the earlier part of the year, Caprio returned to social media with some more sobering news. From his hospital bed, he gazed straight into the camera and once again requested prayers.
"Last year I asked you to pray for me, and it's very obvious that you did, because I came through a very difficult period," he stated. "Unfortunately I've had a setback and I'm back at the hospital."
Caprio's message was both honest and stoic. "I believe the almighty above is watching over us. So please remember me," he added.
For his millions of fans, the request was poignant—but it also captured the same humility and genuineness that had made him so popular on the bench.
What Is Pancreatic Cancer?
Pancreatic cancer arises in the pancreas, a small organ located behind the stomach that is an essential part of digestion and blood sugar management. Though comparatively uncommon, it has one of the lowest five-year survival rates of all major cancers. The American Cancer Society states the five-year survival rate at a mere 13%.
A recent poll conducted by The Ohio State University learned that misapprehensions concerning the disease continue to abound. Over half of Americans younger than 50 claimed that they would not realize early symptoms of pancreatic cancer. One third felt that only older people were susceptible, and 37% believed nothing could be done to reduce their risk.
The reality is more nuanced. While pancreatic cancer is disproportionately found among older adults—average age at diagnosis is 70—incidence among younger people is on the rise. Obesity, diabetes, and excessive alcohol consumption have been suggested as driving factors. Pancreatic cancer ranks among the biggest challenges faced due to the relative impossibility of finding it early. Symptoms tend to present themselves vague and easily dismissed. They can be:
- Unexplained weight loss
- Loss of appetite
- Abdominal or back pain
- Digestive problems
As the tumors increase, jaundice (yellowing of the eyes and skin) can occur, with dark urine, pale-colored stool, or pruritus (itchy skin) in some cases.
Since these symptoms are not overt, most individuals fail to seek medical attention until the illness is advanced. For anyone suffering from these symptoms, professionals advise immediate consultation with a healthcare provider.
Common Misconceptions And Real Risks About Pancreatic Cancer
The October survey highlights the disconnect between perception and fact:
Myth 1: Only elderly people develop pancreatic cancer. Although elderly people are still the most impacted, lifestyle is contributing to the development of cases among younger individuals.
Myth 2: There is nothing you can do to reduce your risk. Actually, lifestyle options like quitting smoking, avoiding too much alcohol, being at a healthy weight, and managing diabetes help decrease risk significantly.
Myth 3: Early symptoms are apparent. Pancreatic cancer symptoms are not like those for skin or breast cancer and are frequently nonspecific and may be confused with other illnesses.
Although no one can completely preclude developing pancreatic cancer, some measures can be taken:
Stop smoking: Pancreatic cancer risk is twofold in smokers but falls dramatically after quitting.
Be at a healthy weight: Obesity is associated with increased risk, and diet and exercise are key preventive strategies.
Control diabetes: Type 2 diabetes over the long term is a recognized risk factor; maintaining blood sugar under control could reduce risk.
Drink in moderation: Excessive alcohol consumption is associated with both pancreatitis and pancreatic cancer.
Learn your family history: Approximately 10% of cases are associated with inherited mutations like BRCA1, BRCA2, or Lynch syndrome. Genetic counseling is advised for those who are at high risk.
While Frank Caprio fights cancer, the support that's poured out is a testament to how deeply he has impacted lives beyond his courtroom. Posts and messages from across the globe continue to pour into his social media sites, saying thank you, stay strong, and praying for him.
Caprio’s story also serves as a broader reminder: health challenges, even for those who seem larger than life, are a human equalizer. His openness about his condition helps shine a light on pancreatic cancer—an often overlooked but deadly disease.
At 88, Judge Caprio continues to teach. Just as he asked for compassion in his courtroom, he now asks for awareness, empathy, and proactive health vigilance. And as he battles this fight, he reminds us that strength is not the absence of vulnerability it's the courage to seek help.
These 5 Medical Conditions Sound Too Weird To Be True - Pt 1

Credits: Canva
When it comes to health, most of us are familiar with the usual suspects: fevers, colds, maybe a sprain or two. But the human body and brain are capable of some truly strange malfunctions that sound more like plots from horror movies or fairy tales than real medical diagnoses. Yet, as odd as they may sound, these conditions are very real, with documented cases and medical research to back them up.
Here are five of the weirdest medical conditions that prove truth can sometimes be stranger than fiction.
Werewolf Syndrome (Hypertrichosis or Ambras Syndrome)
Imagine waking up one day with hair covering nearly every inch of your body, except your palms and the soles of your feet. That is what life can look like for people with Werewolf Syndrome. Officially known as Hypertrichosis or Ambras Syndrome, the condition leads to abnormal and excessive hair growth.
According to the Genetic and Rare Diseases Information Center, individuals may also develop a triangular face, a bulbous nose, or even suffer from missing teeth. It’s a rare genetic disorder, passed down as a dominant trait. So, if one parent has it, there’s a chance the child could inherit it too.
Cases of this syndrome have fueled myths and legends about wolf-men for centuries, and even inspired characters like Lon Chaney Jr.’s iconic “Wolf Man” in Hollywood. But for those living with it, it is a lifelong medical reality rather than a mythical curse.
Facial Blindness (Prosopagnosia)
Most of us forget names occasionally, but what if you couldn’t recognize faces at all—even those of close family or friends? That’s the reality for people with Prosopagnosia, commonly called facial blindness.
The condition stems from abnormalities or damage in the brain, often due to injury, stroke, or neurodegenerative diseases. In some cases, people are simply born with it, a form known as congenital prosopagnosia.
Prosopagnosia doesn’t mean poor memory in general. A person with it may recall voices, clothing, or mannerisms perfectly but be unable to identify someone by their face. In severe cases, some patients struggle to distinguish between a face and an inanimate object, or even fail to recognize their own reflection.
It’s a condition that can make everyday interactions complicated, sometimes isolating, as people often mistake it for rudeness or disinterest.
Sleeping Beauty Syndrome (Kleine-Levin Syndrome)
Fairy tales speak of Sleeping Beauty drifting into years of slumber. In reality, a rare disorder named Kleine-Levin Syndrome, also known as Sleeping Beauty Syndrome, causes people to sleep for extraordinarily long stretches of time.
Episodes can last days or even weeks, with affected individuals sleeping up to 20 hours a day. When awake, they may display unusual behaviors such as binge eating, hallucinating, or even acting childishly. Strikingly, the majority of those affected are adolescent males, according to the National Institute of Neurological Disorders and Stroke (NINDS).
There is no permanent cure, but stimulant medications may help manage symptoms. Fortunately, the episodes tend to decrease with age, often fading by adulthood. Still, for those experiencing it, life can feel like being trapped in a storybook, only without the happily-ever-after.
Mad Cow Disease and Its Human Counterpart
Most people have heard of Mad Cow Disease, scientifically known as Bovine Spongiform Encephalopathy (BSE), which affects the brain and spinal cord of cattle, causing them to behave erratically or aggressively.
While humans don’t catch BSE itself, a related illness called variant Creutzfeldt-Jakob Disease (vCJD) can occur. This rare but fatal brain disorder is thought to be linked to eating beef contaminated with infected tissue.
The U.S. Food and Drug Administration and the World Health Organization both note strong evidence connecting vCJD with mad cow outbreaks, though proving direct transmission remains complex. Infected brain tissue develops spongy holes, leading to memory loss, personality changes, and severe neurological decline.
Thankfully, the number of cases worldwide is small. Still, its very existence once sparked widespread fear about food safety, making it one of the most infamous “weird” diseases of modern times.
Alien Hand Syndrome
Of all the bizarre conditions, Alien Hand Syndrome may be the most unsettling. Imagine one of your hands moving on its own, buttoning a shirt, grabbing objects, or even hitting you, without your conscious control.
That is what people with Alien Hand Syndrome experience. The disorder arises from brain damage due to stroke, tumors, or neurodegenerative diseases. Patients often describe the rogue limb as if it has its own will, and some even give their “alien” hand a name.
While treatments exist, such as Botox injections, behavioral therapy, or simply keeping the hand occupied, there is no permanent cure. Pop culture famously depicted this in the movie Dr. Strangelove, where a character’s hand keeps saluting against his will.
7 Minutes Of Life: The Science Behind What Happens To Your Brain After You Die

Credits: Canva
What happens in the brain at the moment of death has fascinated doctors, philosophers, and ordinary people for centuries. Myths and religious traditions have long spoken of a “life review,” where your past flashes before your eyes. Modern science, for the first time, is beginning to catch glimpses of what really unfolds in the final minutes after the heart stops.
A widely discussed idea is that the brain may continue working for about seven minutes after death, potentially giving rise to vivid flashes of memory and awareness. Recent studies suggest this may not be just folklore.
Recording the Dying Brain
In 2022, doctors in Canada made a startling discovery. They were monitoring an 87-year-old patient with epilepsy when he suddenly suffered cardiac arrest. As his heart stopped, the electroencephalogram (EEG) kept recording his brain activity. What they saw was astonishing: rhythmic brain waves that resembled those seen during memory recall, dreaming, or meditation.
The researchers noted surges in gamma oscillations, which are linked to conscious processing, learning, and memory retrieval. It was as if the man’s brain was playing back moments of his life in a final act of reflection. This provided the first direct evidence that the dying brain may remain active, even organized, after the heart has stopped.
Also Read: What Happens To Human Bodies After Death?
Seven Minutes of Life
The “seven minutes of life” theory emerged from similar findings. When the heart ceases to beat, blood flow to the brain stops, but neurons do not die immediately. Instead, they enter a state of frantic activity as they are starved of oxygen. During this short window, electrical surges ripple across the cortex, creating what some scientists describe as a last burst of consciousness .
Some neurologists believe this window could be responsible for the life-flashing-before-your-eyes phenomenon reported in near-death experiences. Memories may be triggered by abnormal synchronization of neurons, creating vivid, movie-like recollections.
Near-Death Experiences and Life Reviews
The connection between this brain activity and near-death experiences (NDEs) is striking. Studies of cardiac arrest survivors show many report floating above their bodies, seeing tunnels of light, or meeting deceased loved ones. Others describe a panoramic replay of their life events, sometimes accompanied by feelings of peace and detachment.
Dr. Sam Parnia’s large-scale AWARE studies monitored hundreds of patients across multiple hospitals during cardiac arrest. While most did not survive, some who were revived reported precise details of events in the room while they were clinically dead, as well as intense memory flashbacks. These reports align with the idea that the brain, far from shutting down instantly, lingers in a state of heightened, unusual activity.
The Brain’s Last Burst
Neuroscientists suggest that this “last burst” could be explained by the physiology of dying neurons. As oxygen levels plummet, neurotransmitters like glutamate flood the brain. This overstimulates neurons, causing them to fire in abnormal, synchronized ways. Gamma oscillations may peak during this time, briefly sustaining complex conscious experiences.
In animal studies, rats that suffered cardiac arrest showed spikes of coherent brain activity within 30 seconds of death. Human data now confirm similar patterns. Although brief, this activity may be enough to produce vivid subjective experiences.
Consciousness After Death: Science or Spirituality?
These findings raise profound questions. If the brain continues to generate conscious-like activity minutes after death, does this blur the boundary between life and death? Is the “life review” a final, natural brain function, or does it hint at something beyond?
While many scientists caution against overinterpreting the results, others see the possibility of bridging neuroscience and spirituality. The universality of near-death reports across cultures suggests there may be common biological mechanisms at work, yet their meaning remains open to interpretation.
Some traditions describe this as the soul’s transition, while neurologists see it as a natural byproduct of oxygen-starved neurons. Either way, the dying brain appears far from silent.
Redefining Death
Traditionally, death was declared when the heart stopped beating. Today, medicine recognizes that death is a process rather than an instant. Brain activity may persist for minutes, and in rare cases of resuscitation, patients return with memories of those moments. This challenges both how we define death and how long doctors should wait before making the declaration.
Modern guidelines already recommend observing a patient for several minutes after cardiac arrest before pronouncing death. Discoveries about lingering brain activity add further weight to this caution.
© 2024 Bennett, Coleman & Company Limited

