- Health Conditions A-Z
- Health & Wellness
- Nutrition
- Fitness
- Health News
- Ayurveda
- Videos
- Medicine A-Z
- Parenting
- Web Stories
India’s Male Infertility Crisis Affects 27.5 Million Men, Doctors Reveal Shocking Rise In Azoospermia

Credits: Canva
Infertility has traditionally been seen from a woman's health perspective, particularly in nations such as India. However, medical professionals are now shining a light on an unpublicized yet grave crisis: male infertility. An astonishing 27.5 million Indian men are now impacted, representing up to 50% of total cases of infertility, based on recent statistics. Perhaps the most disturbing trend among this surge is the growth of azoospermia — a state where there is no sperm in the ejaculate.
According to the UNFPA 2025 State of World Population report, India's fertility rate has fallen to 1.9 children per woman. While most of the popular debate continues to be focused on women, physicians point out that male infertility, usually brought on by lifestyle diseases, pollution, stress, and waning semen quality, is being the principal factor in this national trend.
Male infertility in India is not openly talked about despite the enormous prevalence. The stigma leads to men avoiding diagnosis and treatment, frequently blaming their female partners for being the only cause of infertilty. Experts maintain that prompt diagnosis, genetic testing, and exposure to advanced reproductive technology have the potential to alter the course of many such afflicted couples.
Dr. Gauri Agarwal, fertility expert presents an interesting case of a couple facing primary infertility because of azoospermia. Genetic tests, i.e., Y chromosome microdeletion analysis, showed normal AZF gene regions. Despite the male partner's absence of sperm in his ejaculate and structural defects in the seminal vesicle and epididymis, physicians were able to obtain sperm surgically, and IVF resulted in a normal pregnancy.
"India is seeing a concerning fall in fertility rates, and male infertility is one of the key drivers behind this trend," stated Dr. Agarwal. "Genetic screening early on, home semen analysis, and online fertility consultations are revolutionizing the field by making it more accessible and stigmatism-free."
What Causes Male Infertility?
Men's infertility is caused by a number of different factors, most frequently being sperm disorders. These may be from low sperm levels to a lack of motility and are most often associated with tendencies such as smoking, drinking, and diet.
The WHO states that India's present rate of infertility is between 3.9% to 16.8%, of which male infertility accounts for 40%.
Dr. Ranjana Mishra, who is a Senior Consultant in Medical Genetics, highlights that even though azoospermia can be overwhelming, evidence-based diagnostics and focused interventions can provide hope. "This case highlights how sophisticated diagnostics and microsurgical skills can make fatherhood possible for men with apparently irreversible infertility."
The following are some of the major factors contributing to the surge in Indian male infertility:
Imbalances in hormones: Usually a result of chronic stress and obesity.
Varicocele: A silent and curable cause of venous dilation in the scrotum that lowers sperm quality.
Infection: Infectious conditions such as HIV or epididymitis can damage sperm production.
Chromosomal disorders: They disrupt male organ development and functioning.
Radiation or chemotherapy exposure: Prevalent in cancer patients, resulting in defective sperm production.
What is Azoospermia?
Azoospermia is one of the most important yet most underemphasized causes of infertility in men. It is a condition where a man's semen has no measurable sperm. Normally, the testicles release the sperm, which pass through the reproductive system and blend with other fluids to create semen—the thick, whitish fluid ejaculated during orgasm.
Azoospermia affects roughly 5% to 10% of men undergoing fertility evaluations. It can be a congenital issue (present at birth) or develop later in life due to various medical, genetic, or environmental factors. Despite its prevalence, azoospermia often goes undiagnosed until couples face difficulty conceiving, making awareness and early testing critical.
Azoospermia affects 5% to 10% of men being evaluated for infertility. There are two types:
Azoospermia due to obstructive azoospermia – when sperm production is normal but the reproductive pathway is blocked.
Azoospermia due to nonobstructive azoospermia – when sperm production is defective, usually because of hormonal or genetic factors.
Treatment varies according to diagnosis. For obstruction, minimally invasive microsurgeries can be used to reestablish sperm flow. For nonobstructive cases, hormone therapy or surgical sperm retrieval and IVF or ICSI (intracytoplasmic sperm injection) may be required.
Dr. Agarwal points out that in the case highlighted, an IVF success was achievable through intervention at an early stage and utilization of sophisticated sperm extraction methods such as TESE (Testicular Sperm Extraction).
How IVF and Genetic Testing Are Can Improve Fertility Care?
With the advent of individualized treatment protocols and genetic technologies, IVF is easier and more effective in cases of male infertility. Methods such as sperm mapping and advanced embryo screening are boosting success rates and cutting back on unnecessary cycles.
"Semen analysis should be the initial step in any couple facing conception delays. It provides us with a snapshot in time of a man's fertility potential and can direct further intervention," said Dr. Mishra.
Additionally, preconception screening for inherited diseases such as beta-thalassemia is becoming increasingly important in determining reproductive choices, so that couples can better prepare themselves.
The cultural silence regarding male reproductive health in India needs to be shattering. With infertility touching almost one out of five Indian couples, and men being responsible for half of them, awareness becomes paramount. Experts are calling on public health agencies, educators, and health professionals to normalize male fertility testing and increase access to diagnostic and treatment resources.
Treating male infertility is not merely about assisting couples to conceive. It is about empowering men to own up to their reproductive well-being, overcome outmoded shame, and adopt science-driven solutions.
Dr. Gauri Agarwal, Founder, Seeds Of Innocens.
Lung Cancer Prognosis In Women Are Not The Same As Men - Why Are Doctors Are Still Missing The Signs?

One of the most common cancers in the world, it is the leading cause of cancer related deaths in the world. It accounts for the highest mortality rates among men and women. However, this has become a rising issue among women. A 2014 study published in the Seminars in Thoracic and Cardiovascular Surgery journal explained that historically lung cancer was mainly studied in men because it was very rare in women. However, as social habits changed and more women started smoking, the number of lung cancer cases in women increased. They mentioned that lung cancer often behaves differently in women than it does in men, especially in non-smokers. This review looks at these differences, including risk factors, how the disease develops, and treatment options.
Lung Cancer in Women
In the United States, lung cancer is the second most common cancer in women and the top cause of cancer-related death. Here are some important statistics from 2012:
- There were an estimated 109,690 new diagnoses in women.
- Lung cancer caused an estimated 72,590 deaths in women, which was more than the number of deaths from breast and colon cancer combined.
- The 5-year survival rate for women is about 18%, which is slightly better than the 14% rate for men, but it is still very low.
- Globally, lung cancer cases and deaths in women are still on the rise, especially in countries where more women are starting to smoke.
What Are Some Risk Factors Other Than Smoking?
Smoking is still the biggest cause of lung cancer in women, responsible for 80-90% of cases. However, a significant number of women who get lung cancer have never smoked.
- Women married to men who smoke have a 25-29% higher risk of getting lung cancer.
- Burning cooking oil or other fuels indoors in areas with poor airflow, especially in developing countries, is a major risk factor.
- A family history of lung cancer increases a woman's risk more than a man's.
- Hormones like estrogen may play a role in the development of lung cancer.
- Studies in some women, particularly in East Asia, have linked the human papillomavirus (HPV) to lung cancer.
What Are Some Challenges Women Face With Lung Cancer Diagnosis?
According to Lungevity, women often face delays and hurdles in getting a lung cancer diagnosis, which can worsen their chances of survival.
Diagnosis Delays
Women are less likely to seek help for early symptoms and can experience longer waiting times between initial doctor visits and a final diagnosis. This can allow the disease to progress before treatment even begins.
Lack of Screening
Many women are not offered lung cancer screening. A study found that women of color who are eligible for screening are six times less likely to be offered it than their male counterparts.
Outdated Rules
Even with recent updates to screening guidelines in the Center of Disease Control and Prevention, which now include people aged 50 and older and with a smoking history of at least 20 pack-years, many women still don't qualify. This is a major issue because a large number of women with lung cancer have a limited smoking history, which means they are often overlooked.
What Other Ways Does Lung Cancer Affect Women
The impact of lung cancer on a woman's well-being is often ignored, yet research shows it's a significant burden.
Psychological Distress
Women with lung cancer have higher rates of depression and anxiety than men. This stress is often made worse by the stigma of the disease, with many women reporting judgmental comments about smoking, regardless of whether they have a smoking history.
Sexual Health
Sexual health is often an overlooked part of cancer care for women. A study of 249 women with lung cancer found that 77% experienced moderate to severe sexual dysfunction. The women reported issues like fatigue and shortness of breath during intimacy, as well as vaginal dryness and pain.
Lack of Women in Clinical Trials
A long-standing problem in healthcare is the low number of women in clinical trials. This makes it difficult to know how effective a treatment is for women specifically.
Low Participation
Women make up only 40% of participants in clinical trials for diseases that affect them, like cancer. For non-small cell lung cancer, this number has not changed much over the past two decades.
Unique Barriers
Women face extra challenges in participating in trials, such as being primary caregivers, which limits their time. There are also gender biases from doctors who may assume women are less interested in research.
Safety Concerns
The lack of female representation is a safety issue. One study found that women were 25% more likely to have severe side effects from cancer treatments, but another study found that they were less likely to report these issues.
More Heat, More Hospital Visits: Climate Change’s Growing Toll On Californians
Credits: Canva
As climate change accelerates, California is bracing for an alarming increase in emergency room (ER) visits, mainly due to rising daily temperatures, according to a new study by researchers from UC San Diego and Stanford University.
While the warming trend may result in fewer deaths from extreme cold, the study warns that this benefit will be overshadowed by a surge in heat-related health issues requiring emergency care.
Warmer Weather Means More ER Visits
“Heat can harm health even when it doesn’t kill,” explained Carlos Gould, lead author of the study and assistant professor of public health at UC San Diego. “Warmer temperatures were consistently associated with more trips to the emergency department, so studies and planning that only consider mortality miss a big slice of the burden.”
Researchers analyzed health and temperature data across California from 2006 to 2017. By projecting these trends to 2050, they estimated a sharp increase in emergency department visits as hot days become more frequent. While the study did note a potential 53,500 fewer deaths due to milder winters, this does not compensate for the wave of new ER visits tied to heat-related health issues.
It’s Not Just Heatstroke
Contrary to popular belief, heatstroke won’t be the only culprit driving people to the ER. “We often think about only the most extreme health impacts of heat waves: deaths,” said co-author Alexandra Heaney, also from UCSD. “This work is showing that many things we may not think about being sensitive to extreme heat are, like poisonings, endocrine disorders, injuries, and digestive issues.”
Mental health problems and physical injuries are expected to increase, particularly on hotter days. Heat can exacerbate existing medical conditions, trigger accidents, and even affect medication absorption and metabolism, making everyday health management more complicated.
Younger People May Suffer More from Heat
The study also found that different age groups will face different types of risks. “Age plays a critical role in shaping health risks from temperatures,” said Gould. “Older adults are particularly vulnerable to cold temperatures, whereas younger adults and children are more affected by heat.”
This means that as heat waves increase, younger populations may start seeing more ER trips for conditions that weren't previously associated with climate risks, creating an evolving and unpredictable healthcare challenge.
An Urgent Need for Planning and Collaboration
Experts involved in the study are calling for hospitals, insurance providers, and public health agencies to act now. Marshall Burke, a co-author and associate professor at Stanford University, emphasized that targeted communication and preparation are critical.
“Understanding who is affected, how, and at what temperatures is critical for planning appropriate responses to protect health,” Burke said. “This is true with or without climate change, but a warming climate makes it more important and alters who is exposed to what.”
With California already battling issues like drought, wildfires, and poor air quality, this looming healthcare burden adds another layer of urgency to climate preparedness efforts.
The findings were published on July 30 in the journal Science Advances. As the climate continues to shift, healthcare systems across the U.S, and especially in heat-prone states like California, will need to brace for a hotter, more hazardous future.
180 Years After The Original Vaginal Speculum Was Invented, It Gets Redesigned: How Does The New 'Lilly-inspired' Device Ease Pain And Fear?

Credits: AFP
For nearly 180 years, the vaginal speculum has remained largely unchanged: cold, metallic, and intimidating. Invented by Dr. James Marion Sims in the mid-19th century and originally tested unethically on enslaved women, the speculum’s history alone is enough to cause discomfort for many. However, it’s not just its past that’s problematic, patients frequently report physical pain, emotional distress, and anxiety linked to the device’s design and clinical use.
While many clinicians have considered it a necessary evil, a growing wave of medical designers, engineers, and gynecologists are challenging that notion, advocating for innovation that centers the patient’s emotional and physical well-being.
The Flower That May Redefine Pelvic Exams
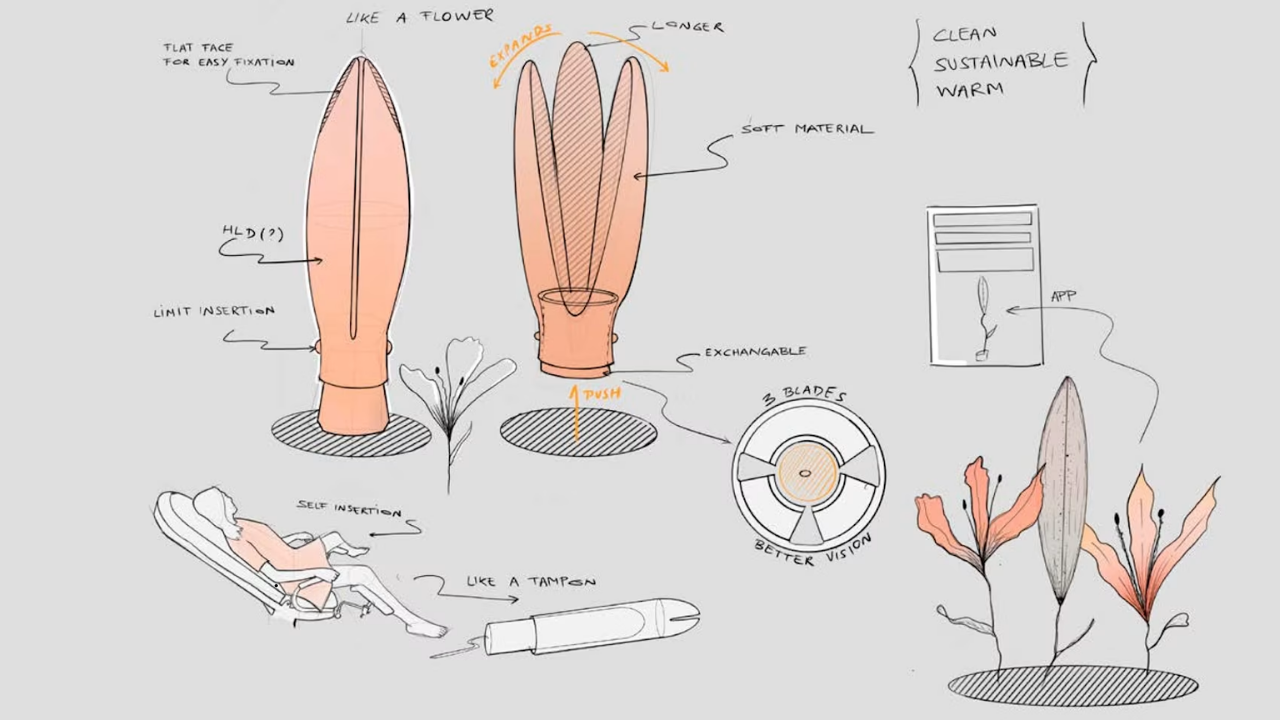
Enter the Lilium, a new, flower-inspired speculum design created by two engineers from Delft University of Technology in the Netherlands: Tamara Hoveling and Ariadna Izcara Gual.
Designed to resemble a blooming lily, the Lilium was conceived as a direct response to the emotional and physical discomfort women often feel during pelvic exams.
Made with soft plastic and featuring an applicator similar to a tampon, the Lilium is shaped to open like a flower, providing better visibility for clinicians while being significantly less intimidating for patients. It also eliminates the harsh clicking sounds and rigid, cold sensation associated with the traditional metal models.
“The aim was to create something familiar, symbolic of the reproductive system, and emotionally safe,” Hoveling said, emphasizing that trauma-informed design can make all the difference in encouraging routine screening.
What the Experts Say
Dr. Archana Dhawan Bajaj, Gynaecologist and IVF Expert at Nurture, strongly supports the redesign. Speaking to Health and Me, she shared how many patients, especially first-timers or trauma survivors, avoid gynecological exams purely because of how threatening the traditional speculum appears.
“It’s cold, mechanical, and terrifying. Many women skip vital preventive exams like Pap smears simply due to fear. A gentler, flower-like design like Lilium not only reduces pain but also the stigma and fear surrounding such check-ups,” said Dr. Bajaj.
She believes the Lilium offers more than aesthetic comfort, it symbolizes empathy in care. “Its soft texture, warmer material, and symbolism of blooming can help women associate pelvic exams with care rather than dread,” she added.
It’s Not Just Physical, It’s Emotional
Pain during pelvic exams isn’t solely physical. Dr. Bajaj explains that anxiety, fear of discomfort, and past trauma often make the experience worse.
“The cycle of fear leads to muscle tension, which increases pain. And that pain only reinforces the fear,” she said. “A redesign like this breaks that cycle. It helps the patient relax, trust the process, and stay engaged with their reproductive health.”
Such emotional consideration is especially crucial for survivors of sexual trauma and post-menopausal women, for whom speculum insertion can be especially distressing.
A History of Redesign Attempts
Lilium isn’t the first attempt at a redesign. Over the years, several models have tried to address comfort:
FemSpec (2005): An inflatable speculum that mimicked a blood pressure cuff. Though it got FDA approval, it was withdrawn in 2008 due to clinical impracticality and physician resistance.
Callascope: A tampon-sized device with a built-in camera for cervical visualization. It bypasses the need for dilation but still faces challenges in physician acceptance and cost-effectiveness.
Nella and Yona: Ergonomic updates to the traditional model. Nella introduced quieter operations and smoother polymers, while the Yona design, developed by San Francisco firm Frog, experimented with a 105-degree angled handle, silicone materials, and a softer, less intimidating shape inspired by sex toy design.
Despite these efforts, none have received the kind of widespread support that Lilium is beginning to garner, thanks, in part, to its empathetic approach and viral crowdfunding campaign, which raised over €100,000 in just two days.
Beyond Design: Why Empathy Matters
The redesign of gynecological tools like the speculum isn’t just about comfort, it’s about dignity, access, and trust. According to Dr. Bajaj:
“Empathetic instruments say something powerful: we value your emotional well-being as much as your physical health.”
This matters. Studies and surveys show that a significant portion of women avoid screenings due to fear or discomfort. In fact, a 2020 study found that 13.6% of women skipped cervical smears due to painful past experiences with speculums.
By designing tools that prioritize empathy and accessibility, we don’t just change devices, we change behaviors. More women are likely to attend screenings, leading to earlier diagnosis, more open conversations about reproductive health, and ultimately, lives saved.
Lilium is still undergoing ergonomic testing, human trials, and regulatory review. But its success so far is an important signal.
“This is not just about a speculum, it’s a symbol of progress in how medicine treats women,” says Dr. Bajaj. “It invites patients in, rather than scaring them off. That’s the future of gynecological care.”
© 2024 Bennett, Coleman & Company Limited

