- Health Conditions A-Z
- Health & Wellness
- Nutrition
- Fitness
- Health News
- Ayurveda
- Videos
- Medicine A-Z
- Parenting
Irregular Sleep, Drinking Caffeine After 3PM Could Raise Your Risk Of Heart Attack And Stroke

Irregular Sleep, Drinking Caffeine After 3PM Could Raise Your Risk Of Heart Attack And Stroke
I’ve always struggled with inconsistent sleep, staying up late and waking up at different times each day. My love for coffee was also on an all-time high with trying all the season specials. But it is only recently, I learned how this irregular sleep pattern and caffeine could increase my risk of heart attack and stroke. Now, I’m prioritizing a consistent sleep schedule and cutting out caffeine after 3 PM to protect my heart.
A new, shocking study shows that irregular sleep patterns can greatly increase the risk of heart attack and stroke. But that's not all: the timing of your caffeine intake could also play a critical role in your cardiovascular health. If you are struggling with inconsistent sleep patterns and regularly sipping on caffeinated beverages late in the day, you may be unknowingly putting yourself at risk for serious heart-related issues.
For most people, sleep is something of a given and we often only consider ourselves as long as we get our required seven to nine hours. However, according to a recent study conducted by researchers at the Children's Hospital of Eastern Ontario, it may not be that long after all. The study, which included more than 72,000 participants, found that people with irregular sleep patterns—those who fall asleep and wake up at vastly different times each day—face a 26% higher risk of experiencing a heart attack or stroke. This increased risk persisted even for those who managed to get enough sleep. The study followed up participants for eight years to track heart events such as heart attacks, strokes, and heart failure. The conclusions were clear: irregular sleep, even if it's sufficient in duration, is a major cardiovascular risk factor.
The researchers found that those whose sleep patterns were highly irregular had a significantly greater chance of life-threatening heart issues. The more erratic your sleep schedule, the greater the risk, regardless of how many hours you sleep. In fact, people with irregular sleep schedules showed worse cardiovascular health outcomes, including higher rates of high blood pressure, elevated stress hormones, and poor blood sugar and cholesterol management.
Senior scientist Dr. Jean-Philippe Chaput said "sleep regularity may be more relevant than sufficient sleep duration in modulating MACE [major adverse cardiovascular event] risk." In the study, it shows that our bodies are comfortable with consistency, and a varied sleep schedule may interfere with other processes that keep us healthy, especially the heart.
Is it Caffeine After 3 PM Causing Sleeplessness?
Another daily habit that may be putting your heart at risk is caffeine consumption after 3 PM. According to Dr. Chaput, the experts emphasize the need for a healthy sleep schedule and avoiding caffeine late in the day. Caffeine can stay in your blood for up to eight hours, and its consumption later in the afternoon can disrupt your sleep cycle.
Consistent, good-quality sleep is necessary for maintaining healthy cardiovascular function, and the disruption of this by late-day caffeine intake exacerbates the risks posed by irregular sleep. When you drink coffee, tea, or other caffeinated beverages too late, the stimulant effect on your nervous system makes it harder to fall asleep at a regular time. This can lead to inconsistent sleep patterns, which, as we have seen, can be harmful to heart health.
Dr Chaput insists that humans need to adopt practices that contribute to regularized sleep habits. This can be attained by establishing a proper sleeping and waking schedule, eliminating afternoon intake of stimulants such as caffeine, and making your body clock coincide with the lifestyle one leads.
How Does Poor Sleep Affect Heart Health?
According to the experts, the disturbance due to irregular sleep patterns impacts more than one physiological process involved in the maintenance of the healthy heart. For example, poor sleep can be associated with increased inflammation of the body, weakened immunity, and altered regulation of blood sugar and cholesterol, all of which contribute to increased blood pressure and weakening endothelial function, both associated with an increased risk for cardiovascular diseases. Sleep also plays a very important role in regulating stress hormones. Poor or disturbed sleep results in increased levels of cortisol, the stress hormone, which increases blood pressure and can have negative impacts on cardiovascular health over time.
Scientists hypothesize that these disturbances trigger a series of negative effects that enhance the risk of developing chronic heart conditions, including hypertension, atherosclerosis, or even heart failure.
Tips to Protect Your Heart and Improve Your Sleep
In order to protect your heart, experts recommend several proactive measures to improve your sleep patterns and lifestyle. First, maintain a regular sleep schedule whereby you go to bed and wake up at the same time every day, including weekends. Consistency will keep your body's internal clock in check.
Along with regulating your sleep, paying attention to your caffeine habits is just as important. To reduce your risk of heart disease and stroke, experts suggest avoiding caffeine after 3 PM. If you’re sensitive to caffeine, this rule becomes even more critical.
In addition, the introduction of stress-reducing activities like yoga or mindfulness can also be beneficial to lower cortisol levels, and therefore both sleep and heart health can improve. A diet rich in antioxidants, healthy fats, and low on processed sugars also helps maintain cholesterol levels and reduce inflammation.
Does Your Sleep Environment Also Has A Role To Play
Apart from the timing of caffeine and your sleep schedule, another very overlooked factor is the quality of your sleep environment. Scientists have long known that the environment in which you sleep has a huge impact on the quality of your rest. Poor quality of sleep, even if your sleep schedule is regular, can cause health risks that are very much the same as those that arise from irregular sleep patterns.
Here’s an additional tip: make sure your bedroom is conducive to restful sleep. This means keeping your room dark, quiet, and cool. A temperature of around 65°F (18°C) is ideal for most people. Consider investing in a comfortable mattress and pillows, and avoid screen time at least 30 minutes before bed to allow your brain to unwind.
Irregular sleep, in association with taking caffeine in late parts of the day, can risk heart attack and stroke, but a simple maintenance of a sleep schedule, the reduction of consumption of afternoon caffeine, and sleep environmental awareness can definitely safeguard one's heart along with total health.
Your sleep is more than just a time for rest; it's a vital component of your long-term health, and maintaining consistency in your sleep habits is one of the best things you can do for your heart.
Cutting Back on Sugary Drinks Can Improve Teen Anxiety

Credit: Canva
A new study suggests that drinking sugary drinks can increase anxiety, among other mental issues, in adolescents by 34 percent.
Sugary drinks are known to be more harmful due to their low fiber, protein, or fat, which typically slow down digestion in solid foods. This means liquid sugar gets into your bloodstream very quickly, causing a sudden jump in blood sugar and insulin levels.
Hyper-fast intake of such drinks can also make it hard for your liver to process the sugar, especially the fructose part. n large amounts, fructose turns into fat in your liver. This buildup of fat is linked to metabolic problems that lead to Type 2 diabetes.
Apart from this, a Bournemouth University, UK literature review analyzed people aged between ten and 19 who drank fizzy drinks, colas, sweetened fruit juices, sweetened milk drinks, energy drinks, and sweetened tea or coffee and found multiple links between the beverages and anxiety diagnosis.
The gut-brain axis — the connection between the brain and the gut — may help explain the link between sugary drinks and anxiety. But gut health is influenced by many factors, including diet, stress, and sleep, which are also linked to anxiety.
Overall, the study suggests that cutting back on sugary drinks could help support teenagers’ mental health. While many studies have looked at how reducing sugary drinks improves physical health, more research is needed to see if it also benefits mental health.
READ MORE: Smoking Cannabis Can Lead To Mental Illnesses In Teenagers, Study Finds
WHO Asks Countries To Tax Sugary Drinks
The World Health Organization is asking countries across the world to increase taxes on sugary drinks and alcohol to reduce cases of chronic conditions such as Type 2 diabetes, obesity, heart disease and fatty liver.
In a January 13 virtual conference, WHO Director-General Dr Tedros Adhanom Ghebreyesus said: "Health taxes have been shown to reduce consumption of these harmful products, helping to prevent disease and reduce the burden on health systems.
"At the same time, they generate an income stream that governments can use to invest in health, education and social protection."
According to a recent report on sugar-sweetened beverages taxes, at least 116 countries tax sugary drinks, including sodas or carbonated canned drinks, but other high-sugar products, such as 100 per cent fruit juices, sweetened milk drinks and ready-to-drink coffees and teas, escape taxation.
Additionally, another report on alcohol taxes shows that even though 167 countries levy taxes on liquor, wine and beer, alcohol has become more affordable or remained unchanged in price in most countries since 2022, as taxes do not get adjusted for inflation and income growth.
How To Cut Back On Sugary Drinks?
Sugary drinks can feel addictive. If you find yourself hooked, try to slowly reduce how much you drink, just like you would with alcohol or tobacco. It helps to plan ahead for when you usually crave a soda.
You can start by mixing plain sparkling water with an equal amount of fruit juice or soda. Then, week by week, slowly reduce the amount of the sugary drink until you're mostly just drinking sparkling water. If it helps, add a little lemon or lime juice for flavor.
Running Ultra-Marathons Harms Your Red Blood Cells, Study Says

Credit: Canva
Participating in ultra-marathons can cause damage to your red blood cells' flexibility and hamper their oxygen-carrying capacity, a study suggests.
A study published in the American Society of Hematology’s journal Blood Red Cells & Iron notes that extreme forms of exercise may harm, rather than support, overall health.
In the case of ultra-marathons, runners experience breakdown of normal red blood cells during races. Over time, their red blood cells become less flexible and potentially reduce their ability to efficiently carry oxygen, nutrients and waste products throughout the body.
Travis Nemkov, associate professor in the department of biochemistry and molecular genetics at the University of Colorado Anschutz and the study’s lead author said of the results: “Participating in events like these can cause general inflammation in the body and damage red blood cells.
“Based on these data, we don’t have guidance as to whether people should or should not participate in these types of events; what we can say is, when they do, that persistent stress is damaging the most abundant cell in the body.”
Red blood cells transport oxygen and waste throughout the body and must be flexible enough to squeeze through small blood vessels. When red blood cells become inflexible or rigid, they lose their ability to deform and navigate through the body's smallest vessels, leading to impaired oxygen delivery, blockage of blood flow, and rapid destruction by the body's filtration system.
This can lead to low hemoglobin and anemia which can pave the way for diseases like Sickle Cell Disease (SCD), thalassemia, hereditary spherocytosis, and, in some cases, the "storage lesion" of blood in transfusion banks.
READ MORE: Ultra Marathoner Sufiya Sufi Runner: The Woman Who Set 5 Guinness World Records
What Is Low Hemoglobin?
Hemoglobin is the oxygen-carrying protein in red blood cells. Adequate hemoglobin levels are essential for keeping organs and tissues properly supplied with oxygen. Without enough of it, the body begins to struggle to meet its basic energy needs.
Low hemoglobin is usually identified through a blood test. It is most often measured as part of a complete blood count (CBC), which checks different components of the blood, including red and white blood cells and platelets, as per Healthline.
While exact reference ranges can vary slightly between laboratories, healthy adult hemoglobin levels usually fall within the ranges listed below. These values are different for babies, children, and teenagers:
- Normal Hemoglobin Count in Grams per Deciliter (g/dL) | Normal Hemoglobin Count in Grams per Liter (g/L)
- Adult Males: 13.8–17.2 | 138–172
- Adult Females: 12.1–15.1 | 121–151
Any reading below these ranges in adults is considered low hemoglobin and suggests that oxygen delivery in the body may be reduced, as per Mayo Clinic.
Is Low Hemoglobin Ever Dangerous?
Low hemoglobin is not always an emergency. In many cases, it develops gradually and can be managed with treatment. That said, very low levels can be dangerous. A hemoglobin level below 5.0 g/dL has been linked to serious complications, including heart failure and even death. Levels under 6.5 g/dL may be considered life-threatening and require urgent medical care.
What Causes Low Hemoglobin?
One of the most common reasons for low hemoglobin is anemia. Anemia occurs when the body does not have enough healthy red blood cells. The most frequent type is iron-deficiency anemia, which develops when the body lacks enough iron to produce hemoglobin.
Other forms of anemia include pernicious anemia, which occurs when the body cannot properly absorb vitamin B12, and hemolytic anemia, where red blood cells are destroyed faster than they are produced.
Low hemoglobin can also be caused by:
- Blood loss or internal bleeding
- Certain cancers, including leukemia, lymphoma, multiple myeloma, and cancers that spread to the bone marrow
- Chronic kidney disease
- Deficiencies of folate or vitamin B12
- Hypothyroidism
- Liver disease
- Poor nutrition or malnutrition
- Myelodysplastic syndrome (MDS)
- Sarcoidosis
- Sickle cell disease and other inherited blood disorders
- Systemic lupus erythematosus
- Thalassemia, a genetic condition that reduces hemoglobin production
- Excess fluid in the body
- Cancer treatments such as chemotherapy and radiation can also lower hemoglobin levels, particularly in adults over the age of 65.
What Does Having Low Hemoglobin Feel Like?
Some people with mildly low hemoglobin may not notice any symptoms at first. Others may begin to feel unwell as levels drop further or remain low over time. Common signs and symptoms include:- Feeling dizzy or lightheaded, sometimes fainting
- Muscle weakness
- Ongoing fatigue or low energy
- Pale or washed-out skin
- Frequent headaches
How Is Low Hemoglobin Treated?
Treatment depends entirely on what is causing the low hemoglobin. A healthcare provider will first identify the underlying reason before recommending treatment. Possible treatment options include:
- Blood transfusion: If hemoglobin is low due to heavy blood loss, a transfusion may be needed to restore levels quickly.
- Vitamin supplements: When nutritional deficiencies are the cause, iron, folate, or vitamin B12 supplements are often prescribed. Hemoglobin levels usually begin to improve within six to eight weeks.
- Intravenous (IV) therapy: In cases where iron or B12 levels need to be raised rapidly, IV infusions may be recommended.
- Bone marrow transplant: This may be required when low hemoglobin is linked to certain cancers or bone marrow disorders.
If a long-term illness is responsible, managing that condition becomes the key part of treatment, alongside monitoring hemoglobin levels regularly.
Danish Study Links Hidden Bacteria In The Gut To Colorectal Cancer
Researchers from Denmark and Australia have discovered a new virus in the gut that can contribute to the development of colorectal cancer in the body, one of the leading causes of death in the world.
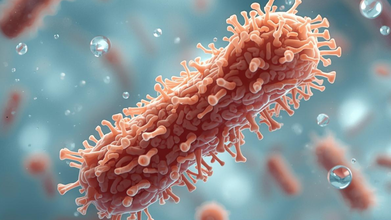
Using genetic sequencing, researchers studied the gut bacteria of cancer patients in a large Danish study and found that Bacteroides fragilis, an anaerobic, gram-negative, pleomorphic to rod-shaped bacterium, often carried a bacteriophage — a virus that infects and reproduces inside bacteria.
This allows it to produce a toxin (BFT) in the colon, promoting chronic inflammation, cell proliferation and tumor growth in the region.
People with colorectal cancer were twice as likely to have this bacteriophage in their gut bacteria. The virus also appears to be previously unknown and does not match any recorded type so far.
Although the first finding came from a small group, it was later confirmed in a larger study of 877 people with and without colorectal cancer. The results suggest that viruses hiding inside B. fragilis may play a role in cancer development.
Microbiologist Flemming Damgaard, from Odense University Hospital in Denmark: "It has been a paradox that we repeatedly find the same bacterium in connection with colorectal cancer, while at the same time it is a completely normal part of the gut in healthy people.
"We have discovered a virus that has not previously been described and which appears to be closely linked to the bacteria we find in patients with colorectal cancer."
What Is Colon Cancer?
Colon cancer develops from polyps in the colon or rectum, often taking years to show symptoms. The cancer begins when small growths called polyps form on the inner lining of the colon or rectum. Over time, changes in the DNA of these cells can cause the polyps to become cancerous.
As abnormal cells multiply, they replace healthy cells and eventually form a mass known as a tumor. This process develops slowly, often taking up to ten years for a precancerous polyp to turn into cancer and begin showing symptoms.
The American Cancer Society notes that colorectal cancer impacts around 1.9 million people every year.. In India, it is the fourth most common cancer among both men and women. In 2022, there were 64,863 new cases and 38,367 deaths.
Projections suggest that incidence will continue to rise by 2026, reflecting both lifestyle changes and improved detection.
Colon cancer can be difficult to detect because it often develops without obvious symptoms. According to experts , these are the three things you should do to protect yourself:
1. Timely risk screening
2. Knowing your cancer family history
3. Acting on early symptoms
What Early Symptoms Should You Look Out For?
Colon cancer rarely announces its presence with dramatic symptoms. More often, it whispers — through changes in bowel habits, subtle abdominal discomfort, or unexplained weight loss.
Some of the most commonly missed early signs include:
- Persistent changes in bowel movements: Chronic constipation or diarrhea often dismissed as dietary effects.
- Blood in stool: Bright red or dark blood should not be ignored.
- Unexplained weight loss: Especially when unintentional.
- Abdominal cramps or bloating: Misinterpreted as common digestive issues.
Persistent changes in bowel habits, especially if they last more than a few days, must be taken seriously. Narrow or ribbon-shaped stools may indicate a tumor partially blocking the colon.
© 2024 Bennett, Coleman & Company Limited

