- Health Conditions A-Z
- Health & Wellness
- Nutrition
- Fitness
- Health News
- Ayurveda
- Videos
- Medicine A-Z
- Parenting
- Web Stories
Is Delhi’s Toxic Air Giving You Migraines? Experts Say It’s Possible

Credits: Gemini
After a short spell of clearer skies, Delhi’s air quality worsened again on Thursday, with the city’s overall AQI climbing to 264, squarely in the “poor” category, according to the Central Pollution Control Board (CPCB). Unfortunately, forecasts suggest that the situation will deteriorate further to the “very poor” zone in the coming days.
A dense layer of smog has settled over much of the capital, and pollution-related illnesses are being reported every day. Many residents have also complained of migraine attacks over the past week, prompting the question: can pollution trigger migraines?
To understand this better, we spoke to Dr. Khusboo Hatekar, Assistant Professor, Department of Neurology, DPU Super Specialty Hospital, Pimpri Pune.
What’s Behind Delhi’s Rising Air Pollution?
Meteorologists attribute the worsening pollution to a western disturbance that has slowed wind speed and created atmospheric stagnation, ideal conditions for pollutants to accumulate.
This stagnant air has intensified health risks, especially for vulnerable groups such as children, senior citizens, and people with chronic respiratory conditions. Doctors have urged Delhiites to reduce outdoor exposure, particularly during early morning and late evening hours when pollution levels are at their peak.
What Is a Migraine?
A migraine is a neurological condition marked by severe, throbbing pain, usually on one side of the head. It often comes with nausea, vomiting, and extreme sensitivity to light or sound. Attacks can last anywhere from a few hours to several days, often disrupting daily routines.
In some individuals, warning signs known as auras appear before or during a migraine episode. These may include visual disturbances like flashes of light or blind spots, as well as tingling sensations on one side of the face or body and even temporary difficulty speaking, as described by the Cleveland Clinic.
Can Air Pollution Trigger Migraines?
Air pollution is now increasingly recognised as a powerful environmental trigger for migraine — a complex neurological disorder that causes recurring, often debilitating headaches. The connection lies in how pollutants interact with the brain’s blood vessels and nerves, setting off inflammatory reactions that heighten pain sensitivity.
The Neurological Link
According to Dr. Khusboo Hatekar, “Migraine pathophysiology primarily involves activation of the trigemino-vascular system. This system includes the trigeminal nerve and associated blood vessels in the meninges.”Under normal circumstances, this system remains stable. But when it becomes overactive, it releases neuropeptides such as substance P and calcitonin gene-related peptide (CGRP). These chemicals cause inflammation and dilation of blood vessels, leading to the throbbing pain typical of migraines.
How Polluted Air Affects the Brain?
Common air pollutants like fine particulate matter (PM2.5), nitrogen dioxide (NO₂), ozone (O₃), carbon monoxide (CO), and sulphur dioxide (SO₂) can activate this same system. When inhaled, these pollutants enter the body through the lungs or nasal passages and create oxidative stress and inflammation in the nervous system.
Dr Hatekar said, “This process triggers immune cells in the brain known as microglia, which then release pro-inflammatory molecules that heighten nerve sensitivity and increase the likelihood of migraine attacks.”
Beyond the Brain: Blood Flow and Hormones
Air pollution can also disturb normal cerebral blood flow and alter levels of neurotransmitters like serotonin, a key regulator of mood and pain. At the same time, exposure to polluted air stimulates the sympathetic nervous system, the body’s stress response network, which further interacts with the trigeminal system to intensify symptoms.
Research has shown a clear association between spikes in air pollution and higher numbers of migraine-related emergency room visits, underlining how environmental conditions can influence neurological health.
The Role of Weather and Genetic Sensitivity
Weather changes often accompany high pollution days, and together, they can worsen the risk of migraines. Fluctuations in barometric pressure, temperature, and humidity, combined with exposure to pollutants, can make certain individuals more prone to attacks.
Some people may also be genetically predisposed to this heightened sensitivity, which explains why not everyone responds to pollution in the same way.
The Broader Health Impact
Dr Hatekar suggested, for people who frequently suffer from migraines, exposure to polluted air can lead to more frequent and intense episodes. This not only reduces their quality of life but also increases the burden on healthcare systems due to repeated consultations and treatments.
Experts believe that improving air quality through strong public health measures could significantly reduce migraine cases in heavily polluted urban regions.
Air pollution appears to trigger migraines through a mix of neuroinflammatory, vascular, and autonomic mechanisms. It activates the trigemino-vascular system, increases oxidative stress, and disrupts the body’s natural balance.
This growing understanding reveals how deeply environmental factors influence neurological conditions and why controlling pollution is not only a matter of clean air but also of reducing the hidden toll it takes on our brains.
Bruce Willis Does Not Have Alzheimer's, According to Wife Emma Hemmings; More Details Inside

(Credit-Brucewillisbw/Instagram)
Sharing a health update of the beloved actor Bruce Willis, his wife Emma Hemmings opened up about how the condition is affecting the actor. In an interview with NewsNation, she spoke on the misconception that the Die-Hard superstar had Alzheimer’s.
“FTD isn’t Alzheimer’s,” she stressed. She clarified that while Frontotemporal Dementia (FTD) affects his ability to communicate and behave, “Bruce doesn’t have Alzheimer’s. So, he does know who we are.”
She noted that while he struggles to verbalize his love, words are not necessary for their family. "We don’t need words," she said. "We have a very deep connection, and we have learned to sort of meet him where he’s at." FTD symptoms can include difficulty with speech, changes in personality, and slow movements, and there is currently no cure.
The Alzheimer’s Research Association explains that dementia is an "umbrella term" used to describe problems with memory, thinking, and reasoning. It's not a single disease. Instead, diseases like Frontotemporal Dementia (FTD) and Alzheimer's are two different causes that lead to similar, but different symptoms.
It is very important for doctors to know the differences between FTD and Alzheimer's. Getting the correct diagnosis early helps patients get the right treatment sooner. This can greatly improve their health and overall quality of life.
How Is FTD Different from Alzheimer’s Disease?
The biggest difference between these two conditions is which part of the brain they damage first. This difference explains why the early symptoms are so distinct.
What Part of the Brain Does FTD affect?
Frontotemporal Dementia (FTD), as its name suggests, mainly affects the front (frontal) and sides (temporal) of the brain. These areas are like the control center for your personality, behavior, and language skills. For example, the frontal lobe handles judgment and controlling your emotions, and the temporal lobe helps you process what you hear and form memories.
What Part of the Brain Does Alzheimer’s Affect?
In contrast, Alzheimer's disease usually starts by damaging areas crucial for memory, such as the hippocampus. These are the parts of the brain that help you learn new things and retrieve old memories. As Alzheimer's gets worse, the damage spreads to more areas of the brain, affecting memory, behavior, language, and even how you see things.
What Ages Do FTD and Alzheimer’s Typically Start?
Another key difference is when people usually start showing symptoms.
FTD often begins when people are younger, typically between 40 and 60 years old. This is why it's sometimes called an earlier-onset dementia.
Alzheimer's is much more common in older adults, usually affecting people who are 65 and over. Getting older is the biggest risk factor for Alzheimer's, but remember, it is not a normal part of getting older or healthy aging.
How Are The Symptoms of FTD different from Alzheimer’s?
While both diseases cause dementia, the first symptoms are usually very distinct, which helps doctors tell them apart.
In early Alzheimer's, the main symptom is memory loss.
- Often forgetting recent conversations or events.
- Having trouble with spatial orientation, which means they might get lost in places they know well.
- Struggle to find the right word, their ability to speak clearly and understand others usually stays better for longer than in FTD.
- Delusions or hallucinations also happen more often as Alzheimer's gets worse.
In early FTD, the initial signs are usually behavioral changes or language problems.
- Acting impulsively
- Lose their filter in conversation
- Become very withdrawn.
This is common in the most frequent type of FTD, called behavioral variant FTD (bvFTD). In another type of FTD called Primary Progressive Aphasia (PPA), the first problem is a difficulty with,
- Speaking
- Understanding language
- Writing.
- While people with advanced FTD will eventually have memory loss, it's not the primary symptom at the beginning.
How Has FTD Affected Bruce Willis?
In the interview Emma Hemmings admitted Bruce is unaware of his frontotemporal dementia (FTD) diagnosis.
She explained that it is a part of the disease itself for the person not to realize their health is declining. When asked about a fear that Willis might have voiced his distress about his condition, she confirmed:
"The person doesn’t realize that they are experiencing a decline in their health. So it’s not denial; this is just a part of the disease. So, it’s a blessing and a curse. But I am grateful that Bruce never tapped into the idea that he had FTD.”
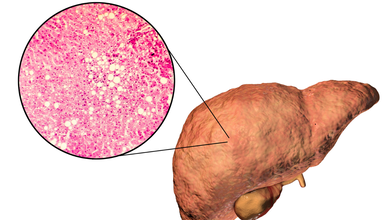
Is There A Way To Detect Fatty Liver Without A Blood Test? Doctor Says Yes
Credits: Canva
Fatty liver disease and insulin resistance often go hand in hand. It is almost like a vicious cycle. What actually happens is when the fat builds up in the liver, it interferes with the body' ability to use insulin effectively. This then triggers insulin resistance, which could fuel fat accumulation, inflammation, and then lead to liver damage. This for a long time could lead to nonalcoholic steatohepatitis (NASH), which is a severe form of fatty liver disease marked by liver inflammation and scarring.
Many experts, including diabetologist Dr Brijmohan Arora has pointed that there could be certain visible changes in your body that could help you detect the early signs of NASH, without having to take a blood test.
What Are The Signs You Should Not Ignore?
As per the doctor, who has over 24 years of experience and practices in Dwarka. He posted a video on Instagram titled ;How to detect a fatty liver without blood tests'. The signs he says include:
Excessive visceral fat — a hard, protruding belly or “belly paunch.”
- Skin tags: small, soft growths on the neck or armpits.
- Red or purple lines on the legs, especially near the ankles.
- A puffy or rounded face with less visible cheekbones.
- High blood pressure (readings above 140 mmHg).
These signs, he explained, can act as “clinical clues” for doctors, especially when patients refuse blood tests.
If You Have A Belly Paunch, It Is A Dangerous Sign
Dr Arora shared story of one of his patients who refused to undergo blood tests and wanted to know whether his liver was healthy. "He had fatty live once and managed to reverse it." However, the patient had returned to the doctor, but refused any testing, this is when the doctor conducted a full physical examination to assess him.
"If your stomach is very protruding and feels hard, it means fat has accumulated around and inside your organs. That is visceral fat. This is a strong indicator of fatty liver." He further added, "If you notice small warts or moles on your neck or armpits, these skin tags are often the number one sign of insulin resistance."
Are There Other Warning Signs Of Insulin Resistance?
Dr Arora also pointed out several other important indicators, including red or purple lines on the feet. He said, "If you see small red or purple lines on your feet, especially near your ankles, it may be a sign of insulin resistance. A puffy face, where your cheekbones are no longer visible, is another common clue."
He also noted that high blood pressure could be one of the most serious warning signs. "If your blood pressure is consistently above 140 or 145, that is quite dangerous. It is one of the most important clinical features of insulin resistance."
Why Is Early Detection Important?
Fatty liver disease and insulin resistance are not just metabolic issues, they can set the stage for type 2 diabetes, cardiovascular disease, and severe liver conditions like NASH. Detecting these early signs can help you take timely steps through diet, exercise, and medical consultation.
Experts recommend maintaining a healthy weight, managing blood sugar, and limiting processed foods and alcohol to protect your liver.
Note: This piece is based on an Instagram post by Dr Arora. Health And Me does not, in any way, promote diagnosis without proper medical testing.
Melatonin and Heart Failure: Could This “Natural” Sleep Supplement Be Causing Adverse Effects on Your Heart?

Credits: Canva
What's making headlines up recently is a new study, which yet has not been peer reviewed about how sleep medicine could have adverse affects on your cardiovascular health. Melatonin, which is a hormone produced naturally by the body to regulate the sleep-wake cycle, is also sold as dietary supplement, typically made synthetically, has been linked to causing heart failure.
The research is from an unpublished study that is set to be presented at the American Heart Association's scientific conference in New Orleans next week. The research notes that the sleep supplement could be linked to 90% increase in heart failure. This has drawn mixed reactions from sleep medicine experts and cardiologists. The experts have urged the public not to panic, and have called for more research into using melatonin for longer duration. Experts who have reviewed the study have noted for the limitations, which has made it challenging to determine whether and how long-term use of the sleep supplement could lead to heart failure. This happens when your heart is not pumping as well as it should.
As per Muhammad Rishi, an associate professor of clinical medicine and spokesperson for the American Academy of Sleep Medicine, "The findings are certainly provocative and warrant attention, especially given the widespread perception of melatonin as a benign, ‘natural’ sleep aid. However, the study is observational and based on electronic health record data, which limits its ability to establish causality."
What Is The Relation Between Melatonin And Heart?
Melatonin is secreted by brain's pineal gland in the evening, and it signals the body for sleep time. However, there are doctors who do not recommend using the supplement to treat chronic insomnia, reports the Washington Post. The reason being that the evidence for its efficacy is limited and inconsistent. The experts note that there is lack of data on its long-term usage.
In the US, melatonin does not require any prescription, however, experts have pointed out that it can only help people to treat sleep-timing problems due to jet lag or shift work, on low doses. Without being prescribed, these medicines could be procured over-the-counter, and could be used to treat chronic sleep disorders without proper guidance.
The new study that analyzed the international database of health records from five years of over 130,000 adults diagnosed with insomnia was able to recognize 65,000 participants who had been prescribed the supplement at least once for one year. The study noted that over the course of five years, around 3,000 people who took had melatonin experienced heart failure.
People who had already been diagnosed with heart failure, or were prescribed other sleep medicines, were excluded from the study.
The patients who took melatonin, were then compared with the ones who did not have melatonin, but had insomnia. The researchers found that this comparison allowed them to account for a variety of factors that could link a person's risk for heart failure, including other health conditions.
Ekenedilichukwu Nnadi, the lead author of the new report and chief resident in internal medicine at SUNY Downstate/Kings County Primary Care in Brooklyn, said, "What stood out most was that we found any association at all."
Nnadi said, "Melatonin is generally viewed as a very safe supplement, as something people, and even physicians, don’t usually worry much about, so we honestly didn’t expect to see a clear signal linking long-term use with higher rates of heart failure, hospitalizations and death.” However, the lead author did emphasize that the findings only showed association and not causation.
He said that the study does not prove that melatonin directly causes heart failure. “It simply shows that people with chronic insomnia who took melatonin long term were more likely to experience these outcomes. It’s an unexpected and important signal that needs to be studied further, ideally in randomized trials.”
© 2024 Bennett, Coleman & Company Limited

