- Health Conditions A-Z
- Health & Wellness
- Nutrition
- Fitness
- Health News
- Ayurveda
- Videos
- Medicine A-Z
- Parenting
Is There A Way To Detect Fatty Liver Without A Blood Test? Doctor Says Yes
Credits: Canva
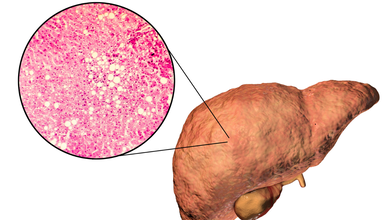
Fatty liver disease and insulin resistance often go hand in hand. It is almost like a vicious cycle. What actually happens is when the fat builds up in the liver, it interferes with the body' ability to use insulin effectively. This then triggers insulin resistance, which could fuel fat accumulation, inflammation, and then lead to liver damage. This for a long time could lead to nonalcoholic steatohepatitis (NASH), which is a severe form of fatty liver disease marked by liver inflammation and scarring.
Many experts, including diabetologist Dr Brijmohan Arora has pointed that there could be certain visible changes in your body that could help you detect the early signs of NASH, without having to take a blood test.
What Are The Signs You Should Not Ignore?
As per the doctor, who has over 24 years of experience and practices in Dwarka. He posted a video on Instagram titled ;How to detect a fatty liver without blood tests'. The signs he says include:
Excessive visceral fat — a hard, protruding belly or “belly paunch.”
- Skin tags: small, soft growths on the neck or armpits.
- Red or purple lines on the legs, especially near the ankles.
- A puffy or rounded face with less visible cheekbones.
- High blood pressure (readings above 140 mmHg).
These signs, he explained, can act as “clinical clues” for doctors, especially when patients refuse blood tests.
If You Have A Belly Paunch, It Is A Dangerous Sign
Dr Arora shared story of one of his patients who refused to undergo blood tests and wanted to know whether his liver was healthy. "He had fatty live once and managed to reverse it." However, the patient had returned to the doctor, but refused any testing, this is when the doctor conducted a full physical examination to assess him.
"If your stomach is very protruding and feels hard, it means fat has accumulated around and inside your organs. That is visceral fat. This is a strong indicator of fatty liver." He further added, "If you notice small warts or moles on your neck or armpits, these skin tags are often the number one sign of insulin resistance."
Are There Other Warning Signs Of Insulin Resistance?
Dr Arora also pointed out several other important indicators, including red or purple lines on the feet. He said, "If you see small red or purple lines on your feet, especially near your ankles, it may be a sign of insulin resistance. A puffy face, where your cheekbones are no longer visible, is another common clue."
He also noted that high blood pressure could be one of the most serious warning signs. "If your blood pressure is consistently above 140 or 145, that is quite dangerous. It is one of the most important clinical features of insulin resistance."
Why Is Early Detection Important?
Fatty liver disease and insulin resistance are not just metabolic issues, they can set the stage for type 2 diabetes, cardiovascular disease, and severe liver conditions like NASH. Detecting these early signs can help you take timely steps through diet, exercise, and medical consultation.
Experts recommend maintaining a healthy weight, managing blood sugar, and limiting processed foods and alcohol to protect your liver.
Note: This piece is based on an Instagram post by Dr Arora. Health And Me does not, in any way, promote diagnosis without proper medical testing.
Delhi AQI Stays ‘Very Poor’ As CM Rekha Gupta Holds Review Meet For Pollution

Credits: iStock
Delhi's air quality remained in "very poor" category, and the AQI stood at 342 at 8am, as per the Central Pollution Control Board. The 24-hour average AQI was logged at 412 under the "severe" category on Tuesday evening when Delhi's quality peaked to record the fourth severe air day in the month of December. With the air quality levels remaining continuously in the "very poor" category, Delhi's Chief Minister Rekha Gupta held a pollution review meet.
What Was Discussed In The Pollution Review Meet By Rekha Gupta?
A review meeting was held to discuss the rising air pollution levels in Delhi on Monday at the Delhi Secretariat. The meeting was attended by the officials from various departments, which also included the Public Works Department (PWD), Transport, Delhi Pollution Control Committee (DPCC), Environment, and others.
Post meeting, Delhi Environment Minister Manjinder Singh Sirsa said that the CM sought responses from multiple departments to discuss various aspects of pollution in the national capital. Sirsa also confirmed that a follow-up meeting will be scheduled on Thursday to continue the discussions on various steps that should be taken to bring down the levels of Delhi's AQI.
Rely On Public Transport - As A Solution To Delhi Pollution
On Sunday, a day before the meeting was held, Delhi's CM spoke on relying on public transport as a solution to Delhi's pollution. She said that the government aims to make the metro network "so comprehensive that people do not need to rely on private vehicles even for last-mile connectivity”.
Delhi's Pollution Is Now A Public Health Risk
An analysis by the Global Burden of Disease (GBD) 2023 found that air pollution is city's single largest health risk. The deaths rose from 15,786 in 2018 to 17,188 in 2023.
Another study published in Scientific Reports, a five-year study titled Respiratory Deposition of Particulate Matter in Delhi: A Five-Year Assessment of Exposure Patterns and Health Risks tracked how particulate matter settles inside the respiratory system and found that men's exposure can be up to 1.4 times higher, especially while walking or commuting. The study noted that men on average spend more time outdoors while working, commuting, or walking in traffic-heavy areas. This leads to an increase in exposure.
A different study published in Frontiers in Public Health, explored the data of 2,96,078 women and girls between the age of 16 to 55 years in Taiwan and correlated it with the long-term air pollution data between 2000 and 2013. None of these women had any history of dysmenorrhea before the survey had began.
Read: Is Delhi's Toxic Air Making Your Period Cramps More Painful? Here's What Study Says
Furthermore, a study published in Nature Communication notes that after four hours of exposure to particulate matter, it was found that people's ability to perform routine tasks and interpret emotions were highly impacted.
If Delhi is able to cut its local pollution by 50 per cent, the pollution too could drop by 50 per cent. The emission should happen across the airshed. However, the focus should be for a long-term action on the source of emission and not short-term optics like cloud seeding, smog towers, water sprinkling or air purifiers.
In fact, as per a study published in Sustainability (MDPI), an open access journal, which mapped Delhi's air quality between 1990 to 2022 and found that transports emit around 10 to 30% of pollution, whereas agricultural residue burning, which is a seasonal source of pollution leads to less than 3% of pollution, whereas firecrackers, another seasonal source, leads to less than 1% of pollution.
Do You Also Have An Awful Sore Throat? It Could Be The New Mysterious Adenovirus

Credits: iStock
Do you feel an awful soar in your throat? Have you noticed that anyone you speak to are also complaining of the same symptoms? All of them, and you, seem tired, have a sore throat and no energy for days and weeks to follow. This might be what people are called "mystery disease" or the "mystery throat virus". However, this is actually the adenovirus.
Most patients with bad throat, explain experts have adenovirus, which is a common virus that spreads throughout the year. However, unlike the flu and COVID, which now have their own prescribed medicines, adenovirus has none.
Read: This Mysterious New Virus Could Spread Faster Than Covid-19 And Flu
What Exactly Is Adenovirus?
Adenovirus is a virus that has more than 60 different strains, which is why it is able to cause a variety of symptoms. Adenovirus refers to a group of common viruses that usually trigger cold- or flu-like illness. It spreads easily because it is far more resilient than many other viruses. Ordinary soap, water, and standard disinfectants do not reliably destroy it, allowing it to persist in the environment. As a result, infections often cluster in places where people spend time close together, such as daycares and military barracks. The virus spreads through the respiratory tract, can be shed in stool, and can survive for some time on contaminated surfaces, according to the CDC.
The reason for its spread right now is due to the surge of flu cases in the southern hemisphere which has influenced the outbreaks in the northern hemisphere. Another reason is the lower flu vaccinate rates, which has now made a large number of population more vulnerable to infections, overall, including adenovirus.
What are The Symptoms Of Adenovirus And What Makes It Very Contagious?
While a lot of the symptoms mimics of those in flu or COVID, including shortness of breath, a sore throat and or a runny nose. However, there are certain unique symptoms of adenovirus that include:
- Diarrhea
- Pink Eye or conjunctivitis
- Ear infection or otitis media
- Swollen lymph nodes
- Pneumonia
- Stomach pain
- Nausea
- Vomiting
Other rare symptoms could also include impact on your bladder or nervous system. As viruses in your bladder can also cause urinary tract infections, and the same virus in your nervous system can cause condition that can affect your brain. These conditions also include encephalitis and meningitis.
Read: Unique Symptoms Of Mysterious Adenovirus And How Long Infection Now Last
What makes this virus unique is that it can spread through easily. Adenovirus is highly contagious. It can spread from one person to another through shaking hands, kissing, or even hugging. The virus could also spread through sneezing, coughing, and if by any other means respiratory droplets transfers to other person in air. It can also spread by touching contaminated surface, and you can get the virus by touching your eyes, nose, or mouths if you do not wash your hands.
The virus can also spread through stool of an infected person. For instance, you can be infected while changing your baby's diaper. It can also spread through unchlorinated water, and a person can be infected with the virus if he or she swims in a pool without adequate chlorine.
Adenoviruses are resistant to many common disinfectants. Therefore, they can remain infectious on surfaces for a long time.
When Should You See A Doctor?
If you are generally healthy, and feel a little down, but do not have shortness of breathe or a high fever, you are safe to go, with supportive care at home. However, pay close attention to those who are already on medical attention, or those who are immunocompromised, or are infants.
If you are sick, have a high fever, and experiencing shortness of breath, it is best to consult your doctor. However, do not show up to your doctor's office, call first.
Ben Sasse Health Announcement: Is His Cancer Terminal?

Credits: Wikimedia Commons
Ben Sasse, former Senator, on Tuesday shared that he has been diagnosed with pancreatic cancer. His diagnosis came at Stage 4.
Is Ben Sasse's Cancer Terminal?
The former two-term senator, 53, revealed this in a social media or X, message: “This is a hard note to write, but since many of you have already sensed something, I’ll get straight to it: Last week I was diagnosed with metastasized, stage-four pancreatic cancer, and I am going to die.”
Also Read: 2 Dead, 21 Injured After Pennsylvania Nursing Home Catches Fire
Stage 4 cancers are terminal and his terminal diagnosis was "hard for someone wired to work and build, but harder still as a husband and a dad," he said.
Stage 4 cancers are terminal because the cancer has metastasized, which means it has spread from its original site or the primary tumor to distant organs and tissues. This makes it extremely difficult to cure with localized treatments like surgery or radiation.
However, the American Oncology Institute does note that stage 4 cancer always does not have to be terminal, especially with breakthrough treatment options like targeted therapy, immunotherapy, or precision medicine. There are now also advanced surgical techniques that use minimal invasion procedures.
Also Read: Ben Sasse Diagnosed With Stage 4 Pancreatic Cancer: What We Know About His Diagnosis
What Is The Chance Of Survival In Stage 4 Cancer?
According to the American Cancer Society, pancreatic cancer makes up about 3 percent of all cancers in the United States but accounts for roughly 8 percent of cancer-related deaths. Most patients are diagnosed at Stage 4, and the disease is widely regarded as largely incurable. Prostate cancer, by contrast, is the second most common cancer among men, and the majority of those diagnosed do not die from it. The five-year relative survival rate for non-metastasized prostate cancer is 97.9 percent, dropping to about 38 percent once it spreads. These figures highlight how early detection and effective treatment options make prostate cancer far more survivable than pancreatic cancer.
What Are The Treatment Options For Ben Sasse At Stage 4 Cancer?
While treatments including chemotherapy, radiation, and in rare situations surgery are available, stage-four pancreatic cancer is still considered largely incurable. The absence of effective early screening contributes to delayed diagnosis, and although a small number of patients, such as Ruth Bader Ginsburg, have lived longer following surgery, these cases are rare. Well-known individuals including Alex Trebek and Aretha Franklin also battled the disease, which remains one of the deadliest cancers in the United States.
Former senator and former University of Florida president Ben Sasse announced on Tuesday, Dec. 23, that he has been diagnosed with terminal stage 4 cancer, as per CNN News.
In the deeply personal message, the former Republican lawmaker from Nebraska described the diagnosis as a “death sentence,” while expressing appreciation for the steady support of his family and close friends.
“I’m fortunate to have incredible siblings and half a dozen friends who are truly like brothers to me. As one of them said, ‘Yes, you’re on the clock, but all of us are.’ Death is a cruel thief, and none of us escape it,” he added.
© 2024 Bennett, Coleman & Company Limited

