- Health Conditions A-Z
- Health & Wellness
- Nutrition
- Fitness
- Health News
- Ayurveda
- Videos
- Medicine A-Z
- Parenting
- Web Stories
Kardashians Take Biological Age Test: Know How It Works

The Kardashians took the biological age test (Image: FreePik)
The Kardashians have lately covered plenty of medical drama, from Kris Jenner's hysterectomy to Kim Kardashian breaking the tip of her finger in an accident. Now, in the latest episode of The Kardashians, Kim, Kris, Khloé Kardashian, and Scott Disick took the groundbreaking 'Horvath test' to determine their biological ages. The test, which measures cellular aging, revealed that 40-year-old Khloé has the cellular age of a 28-year-old. While Kim, 43, has the biological age of 35 and 68-year-old Kris is at a cellular age of 64. These results shocked the Kardashians as well. Khloe, who was visibly surprised said, "Never in a million years! If I had to bet money, I would’ve never bet on myself... Kim is livid, by the way."
What is biological age?
Biological age differs from chronological age, reflecting how old a person seems at a cellular level. There are a lot of factors that influence biological age which include genetics, lifestyle, environment, and health conditions. Tests like the Horvath test offer insights into one's aging process and may prompt lifestyle changes aimed at healthier aging.But how does the test work?
These tests analyze DNA methylation patterns by collecting a blood sample and examining it in a lab. Techniques include measuring telomere length, evaluating biomarkers in blood, and assessing overall health functions. Dr. Shrinidhi Nathany from Fortis Memorial Research Institute explains that AI-powered software compares the results with population data to assess aging speed and potential health risks.
Is it available in India?
The Horvath test is not available in India, however, similar tests including Meand32 test, are offered by diagnostic labs and wellness centers such as Dr Lal PathLabs and SRL Diagnostics. However, the tests are expensive, with costs ranging from Rs 1-3 lakh, due to advanced techniques and the nascent stage of the field. Dr. Basavaraj S Kumbar of Aster Whitefield Hospital notes that high costs and uncertain accuracy, as these tests are still developing, pose significant barriers.While biological age tests offer intriguing insights, they cannot reverse aging. To look younger, experts advise focusing on healthy living practices such as a balanced diet, regular exercise, and stress management over worrying about test results.
From Infants To Elderly: There Is No Age To Get Your Heart Checked, According To Doctors
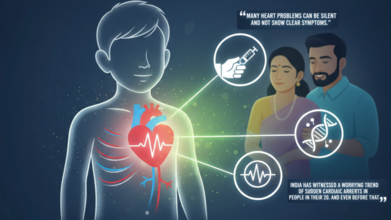
Credits: AI generated and Canva
Every year on September 29, the world observes World Heart Day, while we all talk about the ways one can protect their hearts, changes in food, and lifestyle, we often leave one very vulnerable group - the younger generation, or those below 18. As per the American College of Cardiology, young Indians have a fatigued heart, with 40% of them being between the ages of 13 to 35.
For children in India, this oversight is turning into a public health crisis. Pediatric heart screening is no longer a luxury reserved for the symptomatic; it is a fundamental, proactive check required to combat a rising wave of congenital defects and early-onset, lifestyle-driven heart disease.
What is Pediatric Heart Screening and Why is it the need of the hour?
Pediatric heart screening is fundamentally a medical check-up done to look for heart problems in children. It is an essential health assessment that helps doctors find conditions like heart defects, irregular heartbeat, or the risk of future heart disease at an early stage.
The importance of this check-up is underscored by the silent nature of many cardiac issues in young people. Dr. Bharath A P, Consultant, Paediatric Cardiology, Aster CMI Hospital, Bengaluru, emphasizes the gravity of the situation: “It is very important to get heart screenings done at a young age because many heart problems can be silent and not show clear symptoms”.
He explains that these checks are crucial because “Early screening can find hidden issues like heart defects, abnormal rhythms, or high blood pressure before they become serious”.
Adding a metabolic dimension to this urgency, Dr Mayanka Lodha Seth, Chief Pathologist, Redcliffe Labs, notes that the environmental factors are making the problem worse. She states, “over the years we have seen the lifestyle and eating habits are deteriorating with each passing day, and the reason is easily accessible junk available while sitting at home in just 15 minutes, so getting the overall health screening at a young age, including heart health screening has been, extremely important”.
If these conditions, whether structural or lifestyle-related—are detected early, doctors can give the right treatment and prevent future, often fatal, complications. The ultimate benefit? Early detection helps doctors treat conditions before they become serious , prevent emergencies, improve the child’s growth and activity, and reduce the risk of future heart disease.
Clinical vs. Pathology-Based Screening
Pediatric heart screening must be viewed as a layered approach that combines the traditional clinical assessment of the heart's function and structure with modern pathology-based testing that uncovers metabolic risk factors.
Clinical Screening
From a cardiologist’s perspective, the screening involves direct assessments of the heart’s mechanics. Dr. Bharath A P details the components: “The screening can include listening to the heartbeat, checking blood pressure, and doing tests like ECG or echocardiogram to see how the heart is working”. These clinical checks are particularly useful for children who already display symptoms like chest pain, fainting, or breathing problems. They are also vital for children with a known family history of heart disease.
Pathology-Based Screening
The modern threats to heart health: obesity, high cholesterol, and inflammation, often start silently and require blood tests to uncover. This is the domain of pathology-based screening.
Dr. Mayanka Lodha Seth stresses the importance of this method, particularly in light of modern lifestyle disorders.
“With the increasing incidences of lifestyle related disorders,” she says, “it is recommended to start with preventive screening at an early age starting with pathology-based screenings of blood sugar levels, lipid profile, vitamin deficiencies, and inflammation markers”.
A pediatric screening report can reveal hidden risk markers that might otherwise go unnoticed, such as high LDL cholesterol, high triglycerides, elevated CRP (a marker of inflammation), or abnormal blood sugar levels. This approach can detect congenital abnormalities in infants, but also identify metabolic or lifestyle-linked risks in older children like high cholesterol, insulin resistance, or even early signs of fatty liver. These conditions may not show visible symptoms but can silently progress if undiagnosed.
The two methods work in tandem:
“If these [pathology results] indicate abnormalities, more advanced evaluations like ECGs or echocardiography can be advised in consultation with a pediatric cardiologist,” explains Dr. Mayanka. The biggest advantage of this combined approach is, quite simply, prevention.
The Alarming Indian Context: Congenital Burden and Acquired Risks
The urgency for widespread pediatric heart screening is magnified by the severe burden of heart disease among India's young population.
Dr. Mayanka highlights the scale of the congenital issue: “In India, the burden of pediatric heart disease has been rising congenital heart disease (CHD) is the most common birth defect, affecting nearly 2 lakh babies every year”. To put this into perspective, medical studies and organizations like Children's HeartLink estimate that more than 200,000 children are born each year in India with Congenital Heart Defects (CHD), making it a leading cause of infant mortality.
Equally concerning is the rapid rise in acquired risk factors. Dr. Mayanka adds, “What is equally concerning is the increase in acquired heart risks among children, linked to obesity, sedentary lifestyle, poor diet, and even air pollution”. This trend is not anecdotal; she points out that “recent studies suggest that risk factors like childhood obesity and elevated cholesterol are climbing steadily in urban India, setting the stage for cardiovascular problems much earlier than before”. Early screening can help identify these silent risk factors before they manifest as clinical disease.
Screening from the Womb: The Youngest Age to Start
The question of when screening should begin has a clear answer from cardiology: often, before the child is even born.
Dr. Bharath A P confirms that “Heart screening can be done at any age, even in newborn babies, if there is a need”. Infants can certainly get it done, especially if they show signs like bluish skin, trouble feeding, or fast breathing, or if there is a family history of heart disease. Basic heart checks are part of routine newborn care, and special tests like an echocardiogram can help find heart defects early.
“So yes, infants can have heart screening if doctors suspect a problem or for early detection,” he concludes. For healthy children without symptoms, screening is usually done later during regular check-ups or before starting sports.
For acquired conditions, the timeline differs. Dr. Mayanka notes. “For acquired conditions, pathology-based screenings can begin from school-going age, especially if there’s a family history of diabetes, high cholesterol, hypertension, or sudden cardiac events”. However, she stresses that it is not appropriate to set a minimum age, as “there is no harm in getting the preventive checkups done as they are completely non-invasive and have zero side-effects, so they can be for anyone and everyone”.
The Inherited Risk: Genetics and Family History
For families with a history of heart disease, heart screening transcends prevention and becomes a crucial tool for genetic surveillance.
Dr. Bharath A P emphasizes that if a parent or a close family member has a history of heart disease, “genetic testing and early heart screening for their child become very important”. Some heart problems can be inherited, and checking the child early can help detect issues before symptoms appear.
The power of combining clinical and genetic studies is undeniable. Dr. Bharath confirms, “Yes, paediatric heart screenings combined with genetic studies can help identify inherited heart conditions like hypertrophic cardiomyopathy or arrhythmia syndromes”.
- Screenings like ECG, echocardiogram, and physical exams detect early signs of a heart structure or rhythm problem.
- Genetic testing finds changes in genes that significantly increase the risk of these conditions, even before symptoms appear.
“Knowing about these risks early allows doctors to monitor the child closely, start treatment if needed, and give advice on safe activities,” says Dr. Bharath. Ultimately, combining both methods gives the best chance to prevent serious complications and helps families take timely steps to protect the child’s heart health.
Preventing the Unthinkable: Screening and Sudden Cardiac Arrest
The most compelling argument for pediatric heart screening is its direct link to reducing the devastating rise of Sudden Cardiac Arrest (SCA) in young adults.
Dr. Mayanka Lodha Seth warns, “India has witnessed a worrying trend of sudden cardiac arrests in people in their 20s and even before that”. This is not always a random tragedy;
“Many of these are linked to risk factors that begin silently in childhood like obesity, diabetes, and high cholesterol”. By screening early, parents ensure timely intervention that may help reduce the likelihood of such tragic events later in life.
The role of the pathologist’s report is vital here. Screening allows for the timely detection of conditions like abnormal lipid levels, inflammation markers, vitamin D deficiency, or thyroid dysfunction, all of which can influence heart health. Early interventions, such as lifestyle changes, dietary improvements, or medical management, can significantly reduce the long-term risk of a major cardiac event.
A Non-Favorable Report is a Roadmap, Not a Life Sentence
What happens when a child’s heart screening reveals a risk factor, such as high cholesterol or elevated inflammation? The doctors’ shared advice is clear: avoid panic and embrace action.
Dr Mayanka Lodha Seth has a definitive perspective: “A non-favorable report is not a life sentence it’s a roadmap.” She goes further to challenge the societal perception of health checks:
“We should be scared of detecting chronic conditions at later stages and not identifying it at early stage that allows us to take charge, but don’t know why the society has built it otherwise”. She reminds us that a healthcare journey doesn’t end, but “starts with diagnosis”.
For parents receiving a challenging report, the focus must shift immediately to lifestyle corrections.
“Infact, parents can focus on lifestyle corrections balanced diets, regular physical activity, limiting processed foods, and ensuring adequate sleep,” she advises. In most cases, these steps can significantly improve outcomes. Medical guidance should always be followed, but “panic only delays practical action and wellness”.
Furthermore, Dr. Mayanka highlights the immense long-term benefit of this early intervention: “Also, if prevention is introduced at an early stage, it will become a lifestyle for children making their overall life healthy and filled with wellness”.
For parents worried about exposing their children to hospitals and testing labs, accessibility is no longer an excuse.
“This is where home collection services by Redcliffe Labs help. Health checkups are highly accessible,” says Dr. Mayanka. Trained phlebotomists can collect samples at home with minimal or no discomfort , and reports are shared digitally, effectively reducing both hospital exposure and anxiety for families.
As Dr. Bharath A P summarizes, “If these are detected early, doctors can give the right treatment and prevent future complications”. By embracing the dual approach of clinical and pathology-based screening, parents and doctors can work together to give every child the best possible defense against the rising tide of cardiac risk.
Unusual Hoarse Voice, Cases Surge, New Covid Strain In UK: Here's All We Know About It

Credits: Canva
New Covid Strain: As we enter autumn, rates of respiratory illnesses start to rise and people ask how the most common current lineages, or groups of genetically similar viruses, compare to previous COVID-19 variants.
What Have We Seen So Far?
As autumn settles in, health officials across the UK are reporting an increase in Covid-19 cases. The latest concern is the rise of the Stratus variant, scientifically labelled XFG, and its sub-lineages like XFG.3. Alongside Stratus, the Nimbus variant (NB.1.8.1) is also circulating, but Stratus is quickly becoming the dominant strain.
Genomic surveillance data from the UK Health Security Agency (UKHSA) shows that last month:
- 35% of cases were classified as XFG.3
- 28% as XFG
- 11% as NB.1.8.1
- 7% as XFG.5
- 7% as XFG.3.4.1
Positivity rates for Covid-19 have jumped from 7.6% to 8.4% in just a week, and hospital admissions have also increased from 2.00 to 2.73 per 100,000 people. While current data suggests the illness is not more severe than previous strains, its rapid spread and unusual symptoms are raising concerns.
A Distinctive Symptom: The Hoarse Voice
One feature setting the Stratus variant apart from earlier forms of Covid-19 is a hoarse, croaky voice that often appears early in infection. Many patients report a raspy throat and significant soreness, making it easy to confuse with common colds or seasonal allergies.
According to doctors, while typical Covid symptoms like cough, fever, and fatigue remain, this hoarseness is becoming a standout marker of Stratus infections. Dr Nye, speaking to The Mirror, noted: “In most ways, it’s almost identical. However, people with this version tend to get very sore throats and a hoarse voice, compared with the other more general symptoms.”
Other associated symptoms include:
- Nasal congestion
- Stomach upset
- Severe tiredness
This subtle shift complicates diagnosis, especially as flu and RSV (respiratory syncytial virus) also circulate at the same time.
The Threat of a “Tripledemic”
Public health experts warn that the UK may be heading into a “tripledemic”, a seasonal wave where Covid-19, flu, and RSV spread simultaneously. Each presents with overlapping signs such as cough, fever, and body aches, making it difficult to know which infection a person has without testing.
RSV typically causes cold-like symptoms such as a runny nose, sneezing, and mild cough but can lead to pneumonia in vulnerable groups. Flu usually strikes suddenly with chills, fever, and severe fatigue. Covid-19 overlaps heavily with both, but the hoarse voice linked to Stratus could be one of the few distinguishing features.
Vaccination Drive Intensifies
To combat this surge, the UKHSA, NHS England, and the Department of Health have launched a campaign under the banner “Stay Strong. Get Vaccinated.” The initiative spans television, radio, outdoor billboards, and social media, urging people to get protected before cases climb higher in winter.
For the first time, flu vaccines are being offered to toddlers in community pharmacies in the form of a nasal spray. Covid-19 and RSV vaccines are being prioritized for pregnant women, older adults, and people with weakened immune systems. Most groups will be able to book appointments from 1 October, ensuring early protection before peak transmission season.
Dr Jamie Lopez Bernal, Consultant Epidemiologist at UKHSA, emphasized:
“Flu and COVID-19 levels are starting to slowly increase. While this is expected at this time of year, now is the time for people to come forward for their winter vaccines if they’re eligible, before these viruses circulate more widely.”
What Should You Do If You Feel Unwell?
The UKHSA guidance remains clear: if you develop symptoms of a respiratory infection and feel too unwell to continue normal activities, stay at home if possible and avoid close contact with vulnerable individuals.
For those who cannot stay at home, steps to reduce transmission include:
- Wearing a well-fitted face mask in public spaces
- Avoiding crowded or poorly ventilated areas
- Exercising outdoors instead of indoors
- Covering your mouth and nose when coughing or sneezing
- Washing hands frequently with soap or sanitizer
- Avoiding touching your face unnecessarily
These measures, though familiar from earlier pandemic waves, remain highly effective in curbing spread.
Red Flag Symptoms to Watch For
Doctors advise paying close attention to the nature of your cough. Dr Amir Khan, a regular medical contributor, explains that:
- A dry, tickly cough is often viral.
- A persistent, chesty cough producing phlegm could indicate a deeper infection.
Seek urgent medical advice if you experience:
- A cough lasting more than three weeks
- Coughing up blood
- Unexplained weight loss
- Chest pain
- Breathlessness
Such symptoms may indicate complications that need immediate attention.
Surveillance and What Lies Ahead
The UK continues to rely on robust surveillance systems, including the UKHSA data dashboard, hospital admissions monitoring, and genome sequencing, to track the behavior of new variants. These tools help experts assess transmission potential and guide public health responses.
While the Stratus variant is not currently linked to more severe illness than earlier variants, its rapid spread and distinctive hoarse voice symptom have made it a focal point of this autumn’s Covid-19 landscape.
The bottom line? Vaccination, vigilance, and common-sense precautions remain our strongest defenses. With flu, RSV, and Covid-19 all rising, experts stress that protecting yourself early, especially with seasonal jabs, will reduce both individual risk and pressure on the health system in the coming months.
Doctors Answer The Most Googled Rabies-Related Questions For You

Credits: Canva
Rabies is one of the oldest and deadliest viral diseases known to humankind. Despite being 100% preventable, it still kills nearly 59,000 people worldwide each year, with India accounting for almost one-third of these deaths, according to the World Health Organization (WHO). The virus is carried in the saliva of infected animals and spreads through bites, scratches, or even licks on broken skin. Once clinical symptoms appear, rabies is almost always fatal, making timely prevention the only real protection.
On World Rabies Day, which falls on September 28, doctors remind us of the importance of awareness, timely treatment, and complete vaccination in preventing rabies-related deaths.
Where Should the Vaccine Be Given?
Rabies vaccines can be injected in different body sites depending on age and type of vaccine. Dr. Pooja Pillai, Consultant, Internal Medicine, Aster CMI Hospital, explains:
“Modern rabies vaccines are usually given as an intramuscular injection in the deltoid muscle of the upper arm because it has good blood supply and allows the vaccine to work effectively. In children, the thigh is preferred as their arm muscle may be too small. Earlier practices of using the buttocks are now avoided since fat in that area reduces vaccine effectiveness.”
Dr. Ravi N. Sangapur, Consultant Physician and Diabetologist, also emphasizes: “In adults, the best site is the arm because it produces better immunogenicity.”
Why Do People Still Die Even After Getting the Vaccine?
Reports of rabies deaths despite vaccination often point to lapses in treatment. “One major reason is improper wound care,” notes Dr. Pillai. Thorough washing with soap and water for at least 15 minutes is the very first step after a bite or scratch. Missing vaccine doses, wrong injection site, or use of poor-quality vaccines can also fail to protect.
Dr. Sangapur adds: “Failure to administer immunoglobulins in Category III cases or issues in immunocompromised patients can lead to inadequate immune response and death.”
How Many Doses Are Needed?
The vaccination schedule differs depending on exposure.
Post-exposure prophylaxis (PEP): For those never vaccinated, WHO recommends five doses on Day 0 (the day of the bite), Day 3, Day 7, Day 14, and Day 28. In severe bites, rabies immunoglobulin (RIG) should also be given on Day 0 around the wound.
Pre-exposure prophylaxis (PrEP): For veterinarians, animal handlers, or those at high risk, two doses on Day 0 and Day 7, with a booster on Day 21 or 28, are given to build long-term protection.
“Following the correct schedule is very important to ensure full protection against rabies,” stresses Dr. Pillai.
How Soon Should the Vaccine Be Taken?
Both doctors agree on urgency. “The vaccine should be taken as soon as possible after exposure,” says Dr. Sangapur. Even if delayed, it may still work, but the sooner it starts, the higher the chances of preventing infection. Dr. Pillai highlights that ideally, the first dose should be given within hours of the bite, along with proper wound washing and antiseptic application.
Do Scratches Carry Risk Too?
A common misconception is that only deep bites are dangerous. In reality, scratches also carry risk if the skin is broken.
“Rabies virus is present in the saliva of infected animals, and their nails may carry it from grooming,” explains Dr. Pillai. “Even minor scratches or licks on broken skin can transmit rabies. They must never be ignored.”
Dr. Sangapur agrees: “Such cases should also take the vaccine.”
Is It Just About Dogs?
While dogs remain the most common carriers, other animals can transmit the virus too. Cats, monkeys, mongoose, foxes, jackals, wolves, and in some countries, bats, have all been documented as carriers.
“Any bite or scratch from a mammal should be taken seriously,” says Dr. Pillai. “Thinking only dog bites are dangerous is risky.”
What If You Get Bitten Again After Vaccination?
If a person is re-exposed within three months of completing the vaccine schedule, Dr. Sangapur explains that revaccination is not needed, only proper wound care suffices. However, if exposure happens after three months, two additional booster doses on Day 0 and Day 7 are recommended.Doctors Answer The Most Googled Rabies-Related Questions For You
Dr. Pillai adds that the body develops immune memory after a full vaccination course, providing long-lasting protection, but boosters strengthen the response during re-exposure.
A Preventable Tragedy
Rabies continues to claim lives despite the availability of effective vaccines and treatment. Every bite or scratch from a potentially infected animal must be treated as an emergency. Washing the wound, seeking medical help immediately, and completing the prescribed vaccine schedule can save lives.
© 2024 Bennett, Coleman & Company Limited

