- Health Conditions A-Z
- Health & Wellness
- Nutrition
- Fitness
- Health News
- Ayurveda
- Videos
- Medicine A-Z
- Parenting
- Web Stories
Man Dies After Tick Bite ‘Blew Up’ His Brain: What Kind Of Ticks Carry The Deadly Powassan Virus?

Credits: Canva
With summer season on, tick season begins—ushering in a new wave of concern for emerging infectious diseases. Among them is the Powassan virus (POWV), a rare but deadly tick-borne illness that recently claimed the life of 62-year-old Kevin Boyce from Massachusetts, sending shockwaves through the medical community and his grieving family. His story is not just tragic—it's a critical warning for the public as tick-borne illnesses quietly surge across the country.
In April 2024, Kevin Boyce experienced what he initially believed to be flu-like symptoms—headaches, vomiting, and body fatigue. Within days, those symptoms escalated dramatically. He collapsed in his home and was rushed to Massachusetts General Hospital, where doctors diagnosed him with Powassan virus, a rare virus transmitted by tick bites. Despite aggressive treatment, Kevin succumbed to the virus after his brain experienced severe swelling—an extreme complication known as encephalitis, or inflammation of the brain.
His family describes the ordeal as watching “his brain blow up,” underlining the silent danger of a virus that many Americans have never heard of.
What Is Powassan Virus?
The Powassan virus is named after the town of Powassan, Ontario, where it was first identified in 1958. Though rare, it is part of a group of viruses known as flaviviruses—the same family that includes Zika, dengue, and West Nile virus.
The virus is transmitted by the Ixodes scapularis, commonly known as the black-legged or deer tick, which is also responsible for the spread of Lyme disease. However, unlike Lyme, which typically requires more than 24 hours of tick attachment to transmit, Powassan virus can be transmitted in as little as 15 minutes, according to the Massachusetts Department of Health.
Symptoms of Powassan Virus carried in Ticks
Symptoms of Powassan virus typically appear between 7 to 30 days after a tick bite. These symptoms may include:
- Fever
- Headache
- Vomiting
- Weakness
- Confusion
- Loss of coordination
- Seizures
- Difficulty speaking
In severe cases, the virus causes encephalitis (brain inflammation) or myelitis (spinal cord inflammation), which can lead to permanent neurological damage. According to Yale Medicine, about 10% of these severe cases are fatal, and approximately 50% of survivors suffer from long-term neurological complications.
What Kind Of Ticks Carry The Powassan Virus?
The Powassan virus is primarily carried by two types of ticks in the United States:
Ixodes scapularis – commonly known as the black-legged tick or deer tick, found predominantly in the Northeast and upper Midwest.
Ixodes cookei – also known as the groundhog tick, which is more often found in wooded or rural areas, especially near wildlife like woodchucks and skunks.
Of these, the deer tick (Ixodes scapularis) poses the greater public health risk, as it also transmits Lyme disease, and it's more likely to bite humans. Powassan virus can be transmitted in as little as 15 minutes after the tick attaches—much faster than other tick-borne infections like Lyme.
Because of their size (as small as a poppy seed in the nymph stage) and tendency to attach in hard-to-notice areas, these ticks often go undetected, making early prevention and tick checks critical after spending time outdoors.
Is Prevention Is the Only Protection?
Perhaps the most concerning aspect of Powassan virus is the absence of any vaccine or antiviral treatment. Unlike Lyme disease, which can be treated with antibiotics, Powassan has no direct medical countermeasures. The only approach is preventative care—which makes awareness critical.
To avoid tick bites, the Centers for Disease Control and Prevention (CDC) and the National Institutes of Health (NIH) recommend the following:
- Wear long sleeves and pants when outdoors, preferably light-colored clothing to easily spot ticks
- Tuck pants into socks or use tape to seal clothing gaps
- Use insect repellents containing DEET, permethrin, or picaridin
- Stick to the center of hiking trails to avoid brushing against tick-laden bushes
- Check for ticks on your body, clothes, pets, and gear immediately after being outdoors
- Shower and wash clothes in hot water soon after returning inside
If a tick is found, remove it with fine-tipped tweezers as soon as possible
Recent findings from the University of Massachusetts Amherst’s New England Center of Excellence in Vector-Borne Diseases (NEWVEC) reveal a startling truth: while Powassan virus remains rare in reported cases, it may be significantly underdiagnosed.
A study published in Clinical Microbiology and Infection, led by microbiologist Stephen Rich, highlights that many people bitten by Powassan-positive ticks don’t develop symptoms or seek healthcare. In their passive surveillance study, none of the 38 people bitten by infected ticks reported subsequent illness, suggesting that mild or asymptomatic cases are flying under the radar.
The same research revealed that black-legged ticks bite over 1.36 million people annually in the U.S., based on data from the TickReport testing service in Massachusetts. While Lyme disease has a known high transmission rate, the estimated exposure to Powassan virus ranges from 3,000 to 5,000 people annually, many of whom may never realize they were infected.
Why Powassan Cases Are Rising?
Despite being rare historically, Powassan virus is on the rise in the United States, particularly in the Northeast and Midwest. In 2024 alone, 54 cases were reported nationwide, with 12 cases in Massachusetts. Over the last decade, human cases have increased fourfold, signaling that the threat is becoming more prevalent.
According to the CDC, since 2004, the U.S. has recorded 311 hospitalizations and 44 deaths due to Powassan virus, a number that experts warn may be just the tip of the iceberg.
The rise in infections may be fueled by:
- Climate change, which extends the tick season and habitat
- Growing deer populations, which host these ticks
- Human encroachment into wooded areas, increasing tick exposure
Co-Infections and Complexity
Even more concerning, ticks that test positive for Powassan virus are often co-infected with other dangerous pathogens, including:
- Borrelia burgdorferi (Lyme disease)
- Babesia microti (Babesiosis)
- Anaplasma phagocytophilum (Anaplasmosis)
- Borrelia miyamotoi
This means a single tick bite could expose a person to multiple serious illnesses, compounding the risk and complicating diagnosis.
IV Drip, COVID-19 Shot And Ozempic: How Different Injections Enter The Body In Different Ways
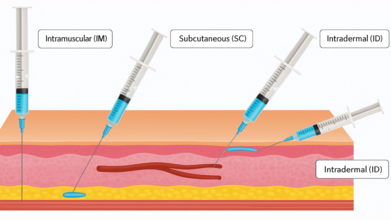
Credits: Canva and AI generated
Injections are one of the most direct and effective ways to deliver medications, nutrients, or fluids into the body. Unlike oral medicines, which must first pass through the digestive system, injections allow a substance to enter the bloodstream, muscle, or tissue directly, leading to faster or more controlled absorption.
There are several types of injections, but four are most widely used in healthcare practice: intravenous, intramuscular, subcutaneous, and intraosseous. Each has its own purpose, method, and site of administration.
Intravenous (IV) Injections

Intravenous injections deliver medication straight into a vein, allowing for rapid absorption and immediate action. Because the bloodstream is accessed directly, this type of injection is considered the fastest way to introduce drugs or fluids into the body.
Common Uses
IV injections or infusions are frequently used in:
- Providing fluids and electrolytes to treat dehydration
- Administering local or general anesthesia before surgery
- Delivering pain relief medications in emergency rooms
- Blood transfusions and iron supplementation
- Nutrition for severely malnourished patients
- Chemotherapy for cancer treatment
- Monoclonal antibodies for infections such as COVID-19
- Injecting contrast dye before imaging tests
Sites of Injection
Typical IV sites include veins on the back of the hands, forearms, or inside the elbow. In infants, doctors may use veins on the scalp or feet.
Intramuscular (IM) Injections
Intramuscular injections deliver medication into the muscle tissue, which has a rich blood supply that helps the drug absorb quickly, as noted by the Centers for Disease Control and Prevention, (CDC) guidelines.
Common Uses
- Most vaccines, such as flu shots
- Antibiotics like penicillin or streptomycin
- Corticosteroids for inflammation or allergic reactions
- Hormones such as testosterone or medroxyprogesterone
- Medications for patients unable to take oral drugs
Sites of Injection
Healthcare professionals usually administer IM shots in:
- The upper outer thigh muscle
- The deltoid (shoulder) muscle
- The hip area
Doctors generally avoid injecting into the buttock due to the risk of damaging the sciatic nerve.
Subcutaneous (SC) Injections

Subcutaneous injections are given into the fatty tissue just beneath the skin and above the muscle. They use a smaller needle to ensure the medication enters the fatty layer rather than muscle tissue. Unlike muscles, fatty tissue contains fewer blood vessels, which means the body absorbs medication more slowly—making it useful for drugs that require steady, prolonged release.
Common Uses
- Insulin for diabetes management
- Blood thinners like heparin
- Vaccines such as MMR (measles, mumps, rubella) and chickenpox
- Pain control medications in palliative care (e.g., morphine, fentanyl)
- Fertility medications and biologics such as Dupixent
Sites of Injection
Typical SC injection sites include:
- The outer or back part of the upper arm
- The front or outer side of the thigh
- The belly (at least a few centimeters away from the navel)
Subcutaneous injections are relatively less painful and carry a lower risk of infection. They are often preferred for patients who need to self-administer medication at home, such as those managing diabetes.
Intraosseous (IO) Injections

Intraosseous injections are less common but extremely valuable in emergency medicine. They involve puncturing the bone marrow with a specialized needle to deliver drugs or fluids directly into the rich blood supply of the marrow. Since the marrow connects directly to the circulatory system, this method is fast and effective when IV access is difficult.
Common Uses
IO injections are usually reserved for critical emergencies such as:
- Cardiac arrest
- Severe trauma or accident injuries
- Overdose or poisoning
- Sepsis or septic shock
- Stroke or seizures
- Obstetric complications (e.g., childbirth emergencies)
They can also be used to administer anesthesia in dental procedures or deliver palliative care pain relief when veins are inaccessible.
Sites of Injection
Common IO access points include:
- The shinbone (tibia)
- The thigh bone (femur)
- The upper arm bone (humerus)
Risks and Side Effects
While injections are generally safe when performed by trained professionals, there are some risks. The CDC notes that common side effects include temporary pain, redness, swelling, or bruising at the injection site. Rare but serious risks may involve nerve damage, abscess formation, bleeding, or infection. Safe handling of needles and proper technique are critical to minimizing complications.
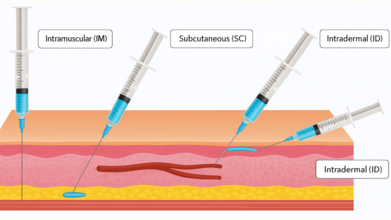
The Bizarre Foot Test That Could Point Towards A Heart Failure
Credits: Canva and Instagram
Thanks to Instagram and other such social media platforms, we know a lot about our health than before. In a video, a person presses on his lower leg, and instead of the skin bouncing back smoothly, it shows small pit-like impressions. The caption on the video reads: A Visible Sign Of Congestive Heart Failure.
A throbbing dorsalis pedis pulse, the artery running along the top of the foot, might appear harmless at first glance. However, doctors caution that such a finding can be an important clinical sign, often linked to conditions such as peripheral vascular changes or fluid overload. In particular, it may reflect elevated central venous pressure (CVP), a common feature of congestive heart failure (CHF).
Medical experts recommend that whenever this sign is seen, it should not be dismissed. Instead, patients should be assessed thoroughly, including checking bilateral pulses, looking for swelling in the legs or feet, and correlating these observations with blood pressure and a full cardiac examination.
Understanding Congestive Heart Failure
Congestive heart failure, also called simply heart failure, is a long-term condition where the heart cannot pump blood efficiently enough to meet the body’s needs. While the heart is still beating, it struggles to keep up with circulation demands. As a result, blood builds up in other parts of the body, most often in the lungs, legs, and feet.
Doctors often describe it with a relatable analogy: imagine a shipping department that is constantly behind schedule. Packages pile up because they cannot be dispatched on time. Similarly, in heart failure, fluid “packages” accumulate in the body, leading to symptoms and complications.
Different Types of Heart Failure
Heart failure is not a one-size-fits-all condition. It has different forms:
- Left-sided heart failure, where the left ventricle struggles to pump blood effectively.
- Right-sided heart failure, which often results from long-standing left-sided failure and leads to blood backing up in veins.
- High-output heart failure, a rare type where the heart pumps normally but the body demands more blood than it can provide.
- Right-sided heart failure is particularly linked to distended veins and visible pulsations, as seen in cases where fluid overload is present.
How Widespread Is the Problem?
Heart failure is alarmingly common. In the United States alone, more than six million people live with the condition, making it the leading cause of hospitalization among those older than 65. With aging populations and rising lifestyle-related diseases such as diabetes and hypertension, the burden of CHF is expected to grow further.
Common Symptoms Of Heart Failure
CHF can manifest in many ways, some subtle and others unmistakable. Typical symptoms include:
- Shortness of breath, especially during activity or at night
- Chest pain and palpitations
- Fatigue and weakness
- Swelling in the ankles, legs, and abdomen
- Weight gain and frequent nighttime urination
- A persistent, dry cough or bloating in the stomach
Some patients may experience only mild discomfort, while others face severe, life-limiting symptoms. Importantly, the condition tends to worsen over time if not managed.
Causes and Risk Factors
Several factors contribute to the development of heart failure, including:
- Coronary artery disease and heart attacks
- Long-standing high blood pressure
- Cardiomyopathy, often due to genetics or viral infections
- Diabetes and kidney disease
- Obesity, tobacco use, alcohol, or recreational drug use
- Certain medications, such as chemotherapy drugs
Risk increases with age, sedentary lifestyle, poor diet, and family history of heart disease. Left-sided heart failure is the most common trigger for right-sided failure, but lung diseases and other organ issues can also play a role.
Potential Complications
Unchecked heart failure can lead to serious complications such as irregular heart rhythms, sudden cardiac arrest, valve damage, fluid buildup in the lungs, kidney or liver failure, and malnutrition. These risks make early recognition of clinical signs, such as visible dorsalis pedis pulsation, critically important.
Diagnosing Heart Failure
Doctors use a combination of medical history, physical examinations, and diagnostic tests to confirm CHF. They typically ask about family history, lifestyle habits, medication use, and other medical conditions. Key tests include echocardiograms, ECGs, chest X-rays, MRIs, CT scans, stress tests, and blood work. In some cases, genetic testing may also be used.
Stages of Heart Failure
Heart failure is classified into four stages (A to D):
Stage A: High risk but no symptoms, often due to conditions like hypertension or diabetes.
Stage B: Structural heart problems but no outward symptoms.
Stage C: Clear symptoms alongside a confirmed diagnosis.
Stage D: Advanced heart failure with severe, treatment-resistant symptoms.
Why Medication Abortion Remains The Most Common And Safe Choice Even In 2025?

Credits: Health and me
In 2023, medication abortion emerged as the most common form of abortion in the United States, reflecting both the convenience and accessibility it offers. With evolving policies, telemedicine provision, and the continued demand for privacy and safety, understanding when and how medical abortion is recommended has become more critical than ever. Abortion in the United States has long been a controversial topic, but the increasing patchwork of state laws has made medical abortion all the more difficult to monitor.
Unlike surgical abortions that take place in clinics, medical abortions tend to occur in private locations with pills prescribed or even ordered over the internet something that makes it difficult to collect data. Throw in the recent round of restrictions and court battles, and researchers, policymakers, and clinicians are left with a distressing void: we just don't know how many medical abortions are being performed, where they are being performed, or what this looks like for women's health.
Although surgical abortion continues as a necessary procedure for specific circumstances, the growth of medication abortion has revolutionized reproductive health care by providing a safe and non-invasive alternative for termination during early pregnancy. This change also highlights the need for proper information, safe access, and quality follow-up care to provide positive health outcomes.
Latest figures from the Guttmacher Institute bring to fore that in the majority of U.S. states with less stringent abortion laws, medication abortion had represented 63% of total procedures offered during 2023. In Wyoming, as an example, 95% abortions were medication-related, with 84% taking the same route in Montana.
Even telemedicine is coming into play: an estimated 10% of medication abortions were provided solely online in states where telemedicine bans did not exist, with some states up to 60%. These trends highlight the importance of preserving and continuing access to abortion pills as an essential part of reproductive health care.
What is A Medical Abortion?
Medical abortion is a non-surgical and non-invasive procedure to end an early pregnancy, usually between 4 and 9 weeks. It uses a two-drug combination: mifepristone, to block progesterone required for continuing the pregnancy, and then misoprostol, which causes uterine contractions to pass the pregnancy. Dr. Rupali Mishra, sonologist and physician at Dr Rupali's Abortion Centre, describes, "Medical abortion is advised if the pregnancy is ensured to be intrauterine and the patient is medically fit".
This involves factors such as lack of severe anemia, bleeding disorders, chronic asthma, or allergies to drugs. She reiterates that availability of follow-up care, such as ultrasound scans to exclude retained products of conception (RPOC), is fundamental to the safe outcome.
When Is Medical Abortion Recommended By The Physician?
Medical abortion is most effective in the early weeks of pregnancy. For pregnancies nine weeks or less, the procedure may frequently be carried out outside of hospital facilities by trained health-care practitioners like gynecologists, nurse-midwives, or certified midwives. However, beyond nine weeks, medical abortion is carried out in hospitals with medical care because risks become greater and complications may arise. "Medical abortion is a convenient and non-invasive procedure, hence suitable for patients who value such factors," remarks Dr. Mishra.
The eligibility criteria too are medically oriented. The patient should not have ectopic pregnancy, severe chronic illnesses of heart, kidney, or liver function, or known contraindications to the medication. Written informed consent is legally mandatory in registered MTP centers to confirm understanding and safety of the patient.
Procedure and Follow-Up Care
After administration, patients can suffer from abdominal cramps, pain, and bleeding for 15–20 days. In most instances, there are no complications, but excessive bleeding, severe pain, or incomplete abortion can lead to a suction evacuation procedure. A follow-up ultrasound after about three weeks confirms the uterus is clear, marking the success of the procedure. Dr. Mishra states, "Even with high success rates, routine follow-up is critical to manage potential complications such as infection, prolonged bleeding, or retained tissue."
Safety Precautions and Possible Side Effects
Medical abortion is normally safe, but improper use or self-administration under unsupervised conditions can prove fatal. Heavy bleeding, incomplete abortion, infection, or, in exceptional cases, shock caused by undiagnosed ectopic pregnancy are serious side effects. Dr. Mishra cautions, "Selling abortion pills over the counter without a prescription is illegal and very risky. Medical supervision is a non-negotiable factor to avoid severe complications."
Medical Abortion vs. Surgical Abortion
Knowing the distinction between surgical and medical abortion enables proper patient decision-making. Surgical abortion is instant and appropriate for later gestation or incomplete medical abortion, whereas medication abortion is non-surgical and appropriate for early pregnancy. Both need follow-up for completion assurance and checking for complications.
What Role Telemedicine Play In Successful and Safe Abortion?
Telemedicine has revolutionized access to medication abortion, especially in states with less-restrictive laws. Virtual consultations with trained providers enable patients to get prescriptions and instructions without face-to-face visits, providing greater privacy and ease. However, according to Isabel DoCampo of the Guttmacher Institute, legal safeguards and access need to keep evolving in order to provide safe provision across states.
Medical abortion is safe, effective and becoming increasingly prevalent for the ending of early pregnancy if under qualified medical care.
Eligibility, procedure, and follow-up must be explained to patients so that safety and health can be assured. As reproductive health policy continues to change, maintaining access to safe abortion care—including medication and telemedicine—remains paramount. Open dialogue with objective medical professionals, coupled with adequate support and counseling, continues to be imperative for enabling individuals to make responsible decisions regarding their reproductive well-being.
Disclaimer: This article is provided for informational purposes and is not medical or legal advice. Readers are urged to seek advice from qualified healthcare providers for medical advice and to consult state or federal authoritative resources for updates on the laws of abortion in the United States.
© 2024 Bennett, Coleman & Company Limited



