- Health Conditions A-Z
- Health & Wellness
- Nutrition
- Fitness
- Health News
- Ayurveda
- Videos
- Medicine A-Z
- Parenting
Medical Memoir: The Accidental Development Of The Small Pox Vaccine
Credits: Canva
'Medical Memoir' is a Health & Me series where we delve into some of the most intriguing medical history and unveil how medical innovations have evolved overtime. Here, we trace the early stages of all things health, whether a vaccine, a treatment, a pill, or a cure.
As per the World Health Organization (WHO), smallpox was officially eradicated in 1980. The last naturally occurring case was diagnosed in Somalia in 1977. In 1980, the WHO declared it to be eradicates, along with the World Health Assembly, marking it as the first human infectious disease to be eradicated worldwide.
So, why are we topic about it today?
Well, for two reasons. What makes it very special is because it was the only human disease to be eradicated so far, mentions WHO. Secondly, the vaccine that worked for its eradication was developed by accident.
A Disease Centuries Old
For centuries, smallpox was humanity’s most merciless enemy — wiping out millions without regard for age, status or geography. It struck kings and commoners alike, killing at least one in every three it infected. In its deadliest form, the toll was even worse.
The disease didn’t just kill — it tortured. Victims first faced high fever, relentless vomiting, and painful mouth sores. Then came the hallmark: fluid-filled blisters that erupted across the body like a cruel constellation. Death often followed within two weeks. And for those who lived, the aftermath could be just as cruel — many were left blind, scarred, or infertile for life.
The disease was indeed deadly, it infected Mozart and also Abraham Lincoln.
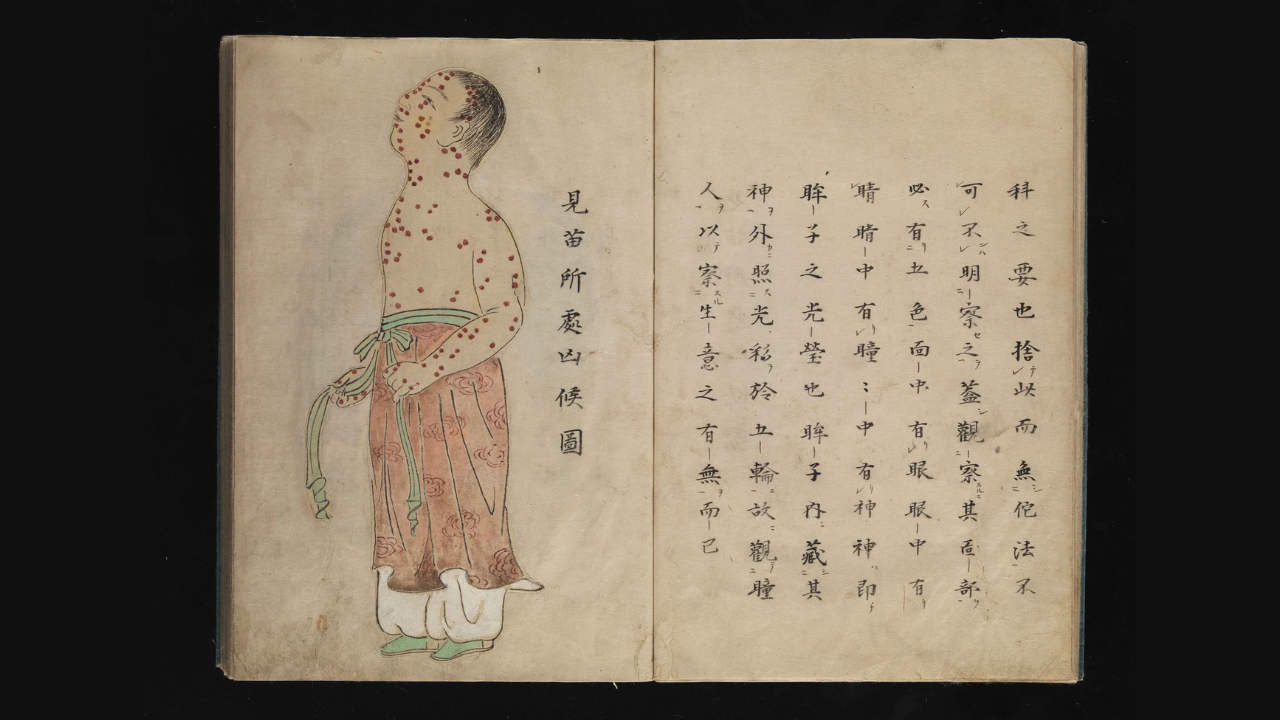
The worst part? No cure was known. It began as early as in the 1350 BCE, studied in Egyptian mummies. There were practices too in parts of Africa, called variolation, name for smallpox. We also find written accounts from China from the mid-1500s that also describe forms of variolation used in China, where smallpox scabs were dried, ground and blown into the nostril using a pipe. In India, a similar method known as inoculation involved pricking the skin of healthy children with a lancet or needle dipped in material from smallpox pustules. Historical records from the 18th century indicate that this practice had been in use for centuries.
An Accidental Observation That Saved Lives

It was not until May 1796, when the world's first smallpox vaccine had been demonstrated, using the same principle as variolation, but with a less dangerous viral source, cowpox.
It was an English physician Edward Jenner who noticed that milkmaids who had contracted cowpox appeared to be protected form smallpox. This led him to hypothesize that cowpox could be used to induce immunity against smallpox. In 1796, Jenner inoculated a young boy, James Phipps, and exposed him to smallpox. He did not develop the disease.
This is how Phipps became the first person in history to be vaccinated against smallpox.
While the experiment, absolutely against today's safety standards, proved the principle of vaccination and marked the very beginning of the chapter that ended smallpox.
Study Reveals The Worrying Reason You Should Protect Yourself From Scrub Typhus

Credit: Pixabay
In 2025, Andhra Pradesh reported 1,566 scrub typhus cases, and nine suspected deaths, according to data from the Integrated Health Information Platform, Integrated Disease Surveillance Programme (IDSP-IHIP) on 8 December. Followed by Karnataka with 1,870 cases, Tamil Nadu 7,308 cases, and Telangana, 309 cases. Scrub typhus cases have significantly increased from previous year. It is one of the deadliest infections affecting multiple organs, or even death. Early it was relevant to poeple working in fields, new studies show it migrating to human settlements.
What Is Scrub Typhus?
Scrub typhus, also known as bush typhus, is a bacterial infection caused by bacteria infection, caused by bacterium Orientia tsutsugamushi. It is spread through bites of infected larval mites, Chiggers.
Most cases of scrub typhus occur in rural areas of Southeast Asia, Indonesia, China, Japan, the Indian subcontinent and northern Australia. Until now, it was believed that chiggers only lurked in the tall grasses of remote paddy fields or dense forests. Due to this, it is commonly known as "farmers' disease", only confined to the fields.
However, new PLOS study data revealed the opposite. The study is led by researchers from Christian Medical College (CMC) Vellore and international collaborators and suggests that the bulk of infections are now even occurring within human settlements.
The study monitored over 32 000 people in Tamil Nadu, which led to the conclusion that agricultural activities, long considered the primary risk factor, were only weakly associated with the disease in high-prevalence areas.
How are Human Settlements A Prime Factor?
Risk for scrub typhus is significantly higher for those living in clustered houses or homes with fewer rooms. If the micro environment around the residence is unmaintained, gardens are patched, or even the damp corners of a courtyard, it could lead to breeding ground for the mites and the rodents that carry Chiggers.
Who Is At Most Risk?
It was once believed that working-age men were the most affected, but the new study tells otherwise. According to the new data, women over 60 are at the highest risk of infection.
As women spend most of their time in and around the home, due to household work, from the kitchen to the laundry, these activities are now the primary cross point of contact with infected mites.
What Is the Risk Factor Of Infection?
As initial symptoms of infection, such as fever, headache, and muscle pain, are the same as viral flu or dengue, many first seek help from untrained practitioners or local pharmacies.
By the time they reach the hospital, the disease has already progressed to severe complications like acute respiratory distress syndrome (ARDS), Kidney failure, or Meningoencephalitis, which is inflammation of your meninges and brain at the same time, a life-threatening condition.
Not only this, the researchers revealed that nearly 10 percent of affected households exceed 25 percent of their income in the treatment.
For severe cases, the cost of treatment can be up to approximately INR 110,000, a staggering sum for rural and peri-urban families earning a fraction of that monthly.
Prevention
- Do not let the grass grow tall around your house
- Tightly maintain kitchen gardens and remove piles of wood or debris where rodents (the primary hosts for mites) might nest.
- As chiggers are usually found close to the ground, do not sit directly on the grass or soil. Use chairs or mats. For children, make them wear socks and full- length trousers while playing in the yard.
- If you notice a small, dark, cigarette-burn-like mark, it is usually left behind by mites. It is most likely "Eschar". It is an important critical clue. As the bite is painless, it often goes unnoticed.
- Do a thorough skin check for an eschar, especially in warm, moist areas like the armpits, groin, or behind the knees.
Early intervention is necessary, as if a fever lasts more than two days, don't just treat it as "seasonal fever".
Consult a qualified doctor and specifically ask about scrub typhus. Infection can be treated with doxycycline common antibiotic, in the early stages. The case fatality rate in this study was 1.5 percent, hospital based studies in South India have previously recorded mortality rates as high 30 percent when treatment is delayed
Shingles Can Strike More Than Once, Vaccination Offers Protection, say experts

Credit: Canva
Shingles, caused by the reactivation of the varicella-zoster virus (the same virus that causes chickenpox), can strike more than once, especially in older adults and people with weakened immune systems. Vaccination against the virus is the most effective way to prevent shingles and related complications, said health experts as part of the Shingles Awareness Week.
The World Health Organization estimates that over 90 percent of individuals worldwide are infected with the varicella-zoster virus, indicating a high susceptibility to shingles.
Health experts explained that the varicella-zoster virus remains dormant in the nerves of the body after an attack of chickenpox.
Dr. Monica Mahajan, Senior Director – Internal Medicine, Max Multi Speciality Centre, Panchsheel Park, told HealthandMe that the virus can remain in an inactive state for two to five decades, or even longer.
When the immunity decreases, the virus can re-activate to cause shingles. The most common symptoms include a rash with sharp, shooting, or stabbing nerve pain.
While it is rare, shingles can recur as one episode of the disease doesn’t grant lifelong immunity.
“It is possible to get shingles infection more than once. An episode of shingles may not give lifelong immunity to the disease. Although it is a rare occurrence, people who have had shingles once can get it again. But those who get vaccinated after the first attack of shingles can prevent the second attack,” Dr. Mahajan said.
How Do Shingles Disrupt Life?
The common manifestation of shingles is a painful blister-like rash, which usually occurs only on one side of the body or face.
It is followed by post-herpetic neuralgia -- a nerve pain that arises in the areas where the rash was located, which often lasts for months or years after the rash has cleared up.
“It is severe and excruciating and is sometimes described as a pain that is worse than chronic cancer pain,” Dr. Chandani Jain Gupta, Dermatologist & Aesthetic Physician, Elantis Healthcare, New Delhi, told HealthandMe.
Dr. Gupta noted that shingles can also affect the eye, impacting the patient's ability to see.
Other less frequent complications of shingles are secondary bacterial infections of the rash, pneumonia, blindness, hearing loss, and neurological complications involving the brain. Fatigue, fever, and sensitivity to touch are other potential complications due to shingles.
Who Is At Risk Of Shingles?
As longevity increases, the phenomenon of ‘immunosenescence’ becomes more common. This means that as we age, our immunity declines, and this process generally starts at the age of 50 years.
"As life expectancy is increasing, more and more people live well beyond the age of 50 years. These people have lowered immunity and are at a higher risk of developing shingles," Dr. Mahajan said.
People who suffer from conditions such as diabetes, HIV, cancer, and patients with kidney or liver transplants are also at a higher risk of shingles because of lower immunity.
Patients who are on certain drugs called the ‘immunomodulators’ (used for conditions like arthritis, lupus, and some skin diseases) that reduce immunity are also more vulnerable to shingles.
How Do Vaccinations prevent Shingles? When to Get It
While some anti-viral medicines can reduce the intensity of the rash and the pain, these are effective only when given within three days of the first symptom. Despite medications, the outcome is not satisfactory in most patients.
But shingles can be prevented with vaccination.
- Adults 50 and older: The CDC recommends that all healthy adults aged 50 years and older receive two doses of the shingles vaccine. The second dose is typically given 2 to 6 months after the first.
- Adults 19 and older with weakened immune systems: If you are 19 or older and have a compromised immune system due to disease (like cancer or HIV) or treatments (like chemotherapy or immunosuppressive drugs). The second dose can be given 1 to 2 months after the first.
Pregnant Woman Left Shocked After Third Nipple Appears in Armpit

Credit: @gynaegirls/Instagram
A now-viral video has revealed how a new mother who believed she had grown excessive fat tissue instead discovered that her body had developed a third nipple under her armpit.
Jasmine, an American woman had given birth five days earlier when a lactation consultant visited her to giver her advice on breastfeeding. The new mother, who was still exhausted and recovering from childbirth, recalled mentioning that her armpits always carried what she believed was excess fat that darkened during pregnancy.
"I breastfed my first baby for one-and-a-half-years, so I'm thinking that there's nothing this nurse can say that's going to surprise me," Jasmine said.
However, after a careful examination, the expert told her that the swelling in her underarm was extra breast tissue and that she also had "a nipple” there.
"When you're pregnant, your nipples and areolas will get really dark, and I have noticed the same change with my armpits, so I was like 'Great! extra breast tissue, I already knew that.' And then the lactation consultant is like 'Let me see,' and I show her, and she goes, 'Oh! yeah... And that's a nipple'.
"You know how cows and puppies and kittens, they have that line of nipples? Yeah, humans have that, too. Tell me why she's telling me about someone that had an extra nipple on her thigh. Telling me I have a third nipple in my armpit before I even had my first postpartum poop is diabolical work,” she said, joking about how little sleep she’d had.
What Do Experts Say?
A third nipple, or a supernumerary nipple, is a fairly common condition in which you have an extra nipple. While researchers are yet o discover why they develop, they note that third nipples form during embryonic development. Some common variations include:- Polythelia: The third nipple is present by itself with no areola (the area of darker skin around your nipple) or underlying breast tissue. This is the most common type of supernumerary nipple.
- Polythelia areolaris: The have an areola present, but no nipple or breast tissue.
- Polythelia pilosa: The have a patch of hair only.
- Polymastia: The third nipple has an areola and has some underlying breast tissue.
- Supernumerary nipple: There is a third nipple that has breast tissue underneath it, but it doesn’t have an areola.
- Supernumerary nipple: There is some breast tissue and an areola, but no nipple is present.
- Aberrant glandular tissue: You have breast tissue, but no nipple or areola is present.
- Pseudomamma: Your third nipple has an areola around it, but instead of breast tissue, you have fatty tissue beneath
According to Dr Rooma Sinha, an obstetrician and gynaecologist at Apollo Hospitals in Hyderabad, Jasmine's third nipple is known as the axillary tail of the breast, a normal extension of breast glandular tissue that tapers into the underarm.
“Some women have axillary tail of the breast. This is probably that. It may produce milk if it has active mammary glands," she told Moneycontrol .
She also confirmed that humans can have supernumerary nipples along what is known as the “embryonic milk line,” extending from the armpit toward the chest. However, this line does not extend down to the thigh, as Jasmine recalled in her video.
According to experts, the axillary tail can feel like a lump or thickened area, particularly during hormonal changes such as pregnancy, breastfeeding or menstruation and may become tender or enlarged.
What Happened Next?
In a follow-up video, Jasmine showed her fans her “underarm boob", on popular demand and clarified that she never attempted to pump milk from the additional nipple because she did not want to stimulate the tissue.“Regular breast production is sufficient for me,” she said, noting that the extra tissue was painful and that she might consider surgically removing the tissue after she decides not to have more children.
© 2024 Bennett, Coleman & Company Limited

