- Health Conditions A-Z
- Health & Wellness
- Nutrition
- Fitness
- Health News
- Ayurveda
- Videos
- Medicine A-Z
- Parenting
- Web Stories
Monsoon Hair Woes: How To Tackle Frizz, Fall, And Flatness In Humid Weather

Credits: Canva
The monsoon season brings with it a much-needed breather from the blazing summer heat. The cooler breeze, the scent of wet earth, and the sound of raindrops can feel almost magical. But let’s be real—while we enjoy the rains, our hair doesn’t always feel the same way. If you're noticing that your hair has suddenly become frizzy, limp, or is falling more than usual, you're definitely not alone.
There are three major hair concerns most people face during the monsoon: frizz, hair fall, and limpness. And surprisingly, they all stem from one root cause—humidity. The excessive moisture in the air plays havoc with your hair's structure and strength.
Let’s break it down.
Why Does The Frizz Happen?
Frizz happens because your hair shaft absorbs the moisture from the air, causing it to swell up and lose its natural pattern. The result? Hair that’s all over the place and hard to manage. Hair fall increases because the roots become soft and weak due to all the dampness, making your strands more prone to falling or breaking. And limp hair is a result of the hair holding too much moisture, which adds weight and flattens your natural volume.
Now, while we can’t do much about the weather, what we can do is change how we care for our hair during this season. And the good news is—it doesn’t have to be complicated.
Time To Rethink Your Shampoo Routine
Start with your shampoo routine. During the monsoon, it’s perfectly okay to wash your hair more frequently—especially if you’re sweating, dealing with oily roots, or getting drenched in the rain. But always choose a gentle, sulfate-free shampoo. These help clean your scalp without stripping away the natural oils your hair actually needs. Harsh shampoos may feel squeaky clean but end up drying out your scalp and making things worse.
Next, don’t skip the conditioner, but go easy on it. This isn’t the time for thick, heavy masks that coat your hair and make it feel greasy or weighed down. Instead, opt for a lightweight conditioner—something that adds moisture without flattening your hair even more. And always apply it only from the mid-lengths to the ends. Avoid the roots, especially during this season.
When To Style?
Styling is another area where less is definitely more. Your hair is already reacting to the humidity, so it’s best to avoid heat styling tools as much as possible. If you need to dry your hair quickly, use a cool setting on your blow dryer, or better yet, let your hair air-dry naturally. And as tempting as it might be to reach for gels, serums, or sprays to control the frizz—be careful. Many of these contain alcohol, which can actually dry out your hair further and make frizz worse in the long run.
Here’s a mindset tip that can really help: try not to fight your hair. Some things, like the weather, are beyond our control. So instead of forcing your hair into behaving a certain way, work with it. This is the perfect season to explore tied-up hairstyles. Think braids, top knots, low buns, or ponytails. They not only keep your hair protected but can also look super stylish with the right accessories.
At the end of the day, monsoon hair care doesn’t have to be a battle. With just a few small changes to your routine and a little bit of patience, your hair can stay healthy, manageable, and maybe even a little bit fabulous—rain or shine.
Because while the weather might be unpredictable, your hair care doesn’t have to be.
Diagnostic Anomaly: This Man’s Brain Began Bleeding After A Regular Dental Checkup
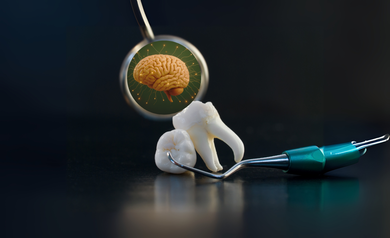
Credits: Canva
'Diagnostic Anomaly' is a Health And Me Series, where we dive deep into some of the rarest of rare diseases. Here, we trace such diseases and what causes them. We also try to bring case studies around the same.
A routine dentist appointment turned into a medical emergency for a man in his late 60s living in Australia. Just 30 minutes after having two teeth extracted, he began experiencing sudden and alarming symptoms — dizziness, vomiting, and a bizarre distortion in his vision, where the world appeared rotated 90 degrees counterclockwise.
These were not trivial side effects of anesthesia or stress. The symptoms were pointing to something much worse. When he came to the emergency room, physicians observed strange signs: abnormal eye movement to the left and a tendency to fall to the right when walking. A brain scan validated their suspicion he was having an intracerebral hemorrhage (ICH), a potentially fatal form of stroke due to bleeding in the brain.
Intracerebral hemorrhage constitutes 10–15% of all strokes and entails a ruptured vessel bleeding into the brain tissue. Ischemic strokes caused by obstructions do not need such immediate intervention, while ICH needs to be urgently treated to stop bleeding, reduce brain pressure, and avoid irreversible neurological injury.
In this patient, the bleeding was in the lower-left side of his brain — a region that affects balance, coordination, and vision. His health care team reacted quickly to treat the hemorrhage, decrease his blood pressure, and relieve intracranial pressure. Thankfully, after receiving immediate treatment, he was stabilized and released with medication to regulate his blood pressure.
Three months after that, he made a dramatic recovery. His eyesight was back to normal, and his balance also considerably improved. To prevent future strokes over the long term, he was put on aspirin, which prevents narrowing of the blood vessels in the brain by keeping the blood thin.
Although clinically managing the case was according to typical stroke procedure, what makes this case uncommon is the suspected etiology: a simple dental treatment.
The man’s symptoms began just half an hour after his tooth extraction. Medical literature contains a few rare reports of individuals experiencing ICH following dental procedures, possibly due to sharp spikes in blood pressure triggered by pain, anxiety, or physiological stress. In this case, the working theory is that the dental procedure, coupled with an undiagnosed underlying condition, created the perfect storm for a stroke.
What Is White Matter Disease?
As the medical staff delved deeper into his background, they discovered further hints. Only six weeks earlier, the man had received neurological tests for potential Parkinson's disease. Scans at the time had already indicated signs of white matter disease — abnormalities in the network of wiring in the brain, which can cause thought to be slower, lead to loss of balance, and predispose to stroke and dementia.
White matter disease targets the brain's "communication highways," the nerve fibers (axons) that carry signals between different areas of the brain and spinal cord. The fibers need a continuous supply of oxygen and nutrients. When blood flow is slowed — because of age, high blood pressure, or damaged vessels — the white matter breaks down, creating lesions that are seen on MRI scans.
Symptoms of white matter disease may range from memory loss, difficulty with coordination, sluggish movement, mood changes, and even urinary incontinence. The symptoms are worse if the damage is more extensive.
But the story didn't end there. Genetic studies of the man revealed he had an uncommon mutation associated with CADASIL-Cerebral Autosomal Dominant Arteriopathy with Subcortical Infarcts and Leukoencephalopathy. This inherited disorder is found in approximately 2 in 100,000 and causes blood vessel walls to thicken. This compromise results in reduced flow of blood into the brain and a drastically increased risk of stroke.
Other research implies ICH can be an complication of CADASIL, particularly when added on top of other influences such as high blood pressure or physical stress.
The course of events now makes sense. The patient's existing white matter disease already compromising brain connectivity and his unknown CADASIL mutation had left his brain's blood vessels particularly susceptible.
The dental removal, though apparently innocuous, perhaps triggered an increase in blood pressure due to stress or pain, a normal physiological reaction in a medical context. For a person with healthy blood vessels, this may not have resulted in anything. But with a brain containing constricted, weakened vessels, the pressure was sufficient to rupture a vessel resulting in an intracerebral hemorrhage.
How Small Triggers Meet Big Risks
This case is an admonition regarding the intricate intersection of genetics, chronic illness, and acute medical stressors. It also highlights the need for recognition and control of risk factors such as hypertension, white matter disease, and unrecognized genetic disorders that affect brain function.
For individuals with cardiovascular risk factors — for example, diabetes, hypertension, or high cholesterol — regular procedures, including dental treatment, might necessitate closer follow-up. Preventive interventions, such as brain imaging in individuals with neurological symptoms and a history of stroke or dementia in first-degree relatives, might detect conditions such as CADASIL before complications arise.
Can White Matter Disease Be Prevented?
Although some white matter changes are inevitable with aging, progression can be slowed down. Good management of heart and vascular health is key. Here's what doctors say:
- Keep blood pressure under control
- Manage high cholesterol and diabetes
- Stop smoking
- Be physically active
- Eat a heart-healthy diet (such as the Mediterranean diet)
Studies have established that lowering cardiovascular risk has been proven to reduce white matter lesions, thus reducing stroke, dementia, and physical disability risks later in life.
A routine dentist visit triggered a series of events that almost resulted in a catastrophe for this Australian man but with timely rescue and extensive diagnostic procedures, not only did he recover well, but the doctors also discovered a rare genetic disorder that might have been a future threat.
Occasionally, the body's reaction to less invasive procedures can expose deep-rooted problems. Paying attention to your body, reporting new symptoms, and being proactive about brain and heart health can be the difference-maker — particularly when the indicators are easy to miss.
Pop Star Ella Henderson Talks About Her Painfully 'Devastating' Diagnosis After Years Of Struggle

Credits: Instagram/ellahendersonofficial
Pop star Ella Henderson’s voice has filled arenas across the UK and beyond, but her latest message isn’t a chart-topper—it’s a powerful, deeply personal disclosure that’s resonating with millions. In a recent Instagram video, the 29-year-old singer revealed she was diagnosed with endometriosis earlier this year, after struggling for years with intense stomach bloating, pelvic pain, and emotional distress.
What Henderson didn’t expect was how long and difficult her journey to a diagnosis would be—and how sharing it would help shine a spotlight on one of the most misunderstood chronic conditions affecting people assigned female at birth.
“For the last few years, it's been a bit of a rollercoaster, to say the least,” Henderson confessed in her video. While fans watched her perform and thrive in the spotlight, behind the scenes she was quietly battling unrelenting symptoms. She describes how she was plagued by stomach bloating, pelvic discomfort, and deep emotional turmoil—made worse by not being taken seriously.
“I thought at one point that this was just all in my head,” she said. “I wasn’t really believed.”
For many with endometriosis, that experience is painfully familiar.
After undergoing a laparoscopy—a minimally invasive surgical procedure used to diagnose and sometimes treat endometriosis—Henderson received confirmation that she wasn’t imagining anything. The procedure uncovered severe endometrial growths and scarring behind her uterus, affecting her bladder and bowel.
“Although the diagnosis was devastating, it was also validating,” she explained. “I could finally take control of my body.”
That moment of clarity often takes years for patients. According to Endometriosis UK, it takes an average of eight to nine years from symptom onset to diagnosis in the UK. Many people, like Henderson, suffer in silence, cycling through misdiagnoses while trying to manage what often becomes debilitating chronic pain.
What makes it harder is that some people have severe symptoms, while others may be asymptomatic. The severity of symptoms doesn't always align with the extent of the disease. Henderson spoke openly about how her physical struggles snowballed into mental health challenges. Living with constant pain, while being dismissed or misdiagnosed, took a toll.
“Not being believed led to periods of depression, isolation, and anxiety,” she said. “If health practitioners had recognised my symptoms sooner, all that might have been spared.”
This psychological burden is common among endometriosis patients. According to studies, mental health disorders, including anxiety and depression, occur at higher rates in those living with chronic pain from endometriosis. And yet, mental health support is rarely part of routine treatment plans.
Though there’s no cure for endometriosis, Henderson’s surgery helped ease her symptoms significantly. She’s now committed to long-term management, including lifestyle adjustments, possible hormonal therapy, and regular medical monitoring.
She’s also using her platform to advocate for awareness. In partnership with Endometriosis UK, Henderson is promoting tools to help others recognize symptoms early. One tool allows users to check symptoms in under a minute and generate a personalized letter for their healthcare provider—a small step that could dramatically shorten the diagnostic timeline for many.
Emma Cox, CEO of Endometriosis UK, praised Henderson’s courage in going public:
“Ella’s willingness to share her story will no doubt help others in their diagnosis journey,” she said. “Highlighting the significant and detrimental impact the condition can have on all aspects of someone’s life.”
And she’s right, endometriosis affects 1 in 10 women and people assigned female at birth—that’s over 1.5 million in the UK alone. Yet, stigma, misinformation, and delays in care are still the norm.
What is Endometriosis?
Endometriosis is a medical condition in which tissue that resembles the lining of the uterus grows outside the womb. These renegade cells are able to adhere to organs such as the ovaries, bladder, bowel, or even below the pelvis, responding to hormonal shifts similarly to uterine tissue—thickening, deteriorating, and bleeding with every menstrual cycle but unlike during a normal period, this tissue has no place to go, leading to inflammation, scarring, organ damage, and extreme discomfort.
Symptoms are diverse but frequently include:
- Heavy or painful periods
- Pelvic pain that is chronic
- Discomfort during intercourse
- Bowel and urinary discomfort
- Inability to conceive
- Severe bloating, also referred to as "endo belly"
- Excessive fatigue
Types of Endometriosis
There are four primary forms of endometriosis:
Peritoneal (superficial): On the thin layer of the pelvis.
Ovarian (endometriomas): Ovarian cysts packed with old blood.
Deep endometriosis: Deep tissue like in the bowel or bladder.
Extra-pelvic endometriosis: Uncommon instances where lesions occur in the lungs or surgical incisions.
Associated conditions such as adenomyosis, in which endometrial tissue invades the uterine wall, tend to exist concurrently with endometriosis, further complicating diagnosis and treatment.
While treatment involves hormonal therapies, analgesics, physical therapy, and surgery in some cases, there is no silver bullet, and most patients have to try a series of methods before experiencing relief.
And though Ella's celebrity generates publicity, the struggle for recognition, treatment, and compassion is that of every woman, girl, and individual touched by this frequently hidden disease.
If you or someone you know is experiencing symptoms of endometriosis, don’t wait. Speak with a healthcare professional and explore resources like Endometriosis UK or the Endometriosis Foundation of America because the sooner we stop doubting women’s pain, the sooner we start healing.
How A Painful Discharging Lesion In Back Turned Out To Be a Rare Taligut Cyst

Credits: Radipaedia
For over eight years, a 37-year-old, Delhi-based woman silently battled a painful, discharging lesion on her lower back. The condition, located in the sacrococcygeal region near her tailbone, was repeatedly mistaken for a common infected sinus or abscess.
Despite undergoing multiple incision and drainage (I&D) procedures, the lesion persisted—causing chronic pain, swelling, and periodic discharge.
Strikingly, the patient exhibited no symptoms related to digestion or bowel movement, further complicating the clinical picture. The misdiagnoses and unsuccessful treatments continued for years, with little improvement in her quality of life. That was until a recent evaluation led to a breakthrough discovery.
How Did The Diagnosis Happen?
The patient’s condition took a dramatic turn when her case was referred to Redcliffe Labs, which is a pan-India diagnostic services provider. The consultant pathologist, Dr. Mayanka Seth, led the team that reviewed the case with a renewed perspective.
Initial clinical assumptions continued to point toward common conditions such as pilonidal sinus or subcutaneous abscess. However, upon detailed examination, the team noted that the lesion was unusually deep and showed no communication with the anal canal. This prompted surgical intervention for complete removal of the cystic structure.
Subsequent histopathological analysis confirmed a rare and unexpected diagnosis: subcutaneous tailgut cyst—a congenital lesion that arises from embryonic remnants of the hindgut.
While tailgut cysts are rare in themselves, their typical location is deep within the pelvis. In this case, the cyst had developed just under the skin near the tailbone, making it an extremely rare presentation and a diagnostic challenge.
The case also been documented and published in the Indian Journal of Case Reports. This has contributed to medical literature on rare congenital anomalies.
Treatment and Complete Recovery
Following the complete surgical excision of the cyst, the patient experienced relief from her chronic symptoms. With no further discharge, pain, or swelling, her quality of life also improved.
“This case throws light on the importance of considering rare congenital lesions when conventional treatments fail to provide results,” said Dr. Mayanka Seth. “Subcutaneous tailgut cysts are easily misdiagnosed due to their resemblance to more common infections in the sacrococcygeal area. Accurate diagnosis often hinges on thorough clinical evaluation and timely histopathological examination.”
What Are Tailgut Cysts?
As per Radippaedia, a peer-reviewed, open-edit radiology resource, Taligut cysts, also referred to as retrorectal cystic hamartomas are rare congenital growths believed to develop from remnants of the embryonic hindgut. These lesions are typically found in the retrorectal or presacral space, although extremely rare cases have been reported in unusual locations such as the perirenal region or subcutaneous tissues.
Who Is Affected?
Tailgut cysts show a strong female predominance and are most commonly diagnosed between the ages of 30 and 60. However, they can occur at any age.
Symptoms
In many cases, tailgut cysts are discovered incidentally during imaging or unrelated examinations. When symptoms do occur, about half of the patients report perirectal discomfort, which may include pelvic pain or constipation.On gross examination, these cysts usually appear as multiloculated (multi-chambered), thin-walled masses with a shiny internal lining. They are typically filled with mucoid (gel-like) material. A distinguishing feature of tailgut cysts is their varied epithelial lining, which may include ciliated columnar cells, mucin-secreting columnar epithelium, transitional epithelium, and squamous cells.
These lesions generally measure a few centimeters in size. Occasionally, they may be associated with defects in the sacral bone or exhibit internal calcifications.
© 2024 Bennett, Coleman & Company Limited

