- Health Conditions A-Z
- Health & Wellness
- Nutrition
- Fitness
- Health News
- Ayurveda
- Videos
- Medicine A-Z
- Parenting
- Web Stories
Ortho Surgeon Reveals The Real Reason Behind This 29-Year-Old Woman's Stage 3 Fatty Liver Diagnosis - It Wasn't Alcohol
(Credit - Canva)
Just like any other office worker, this 29-year-old woman, followed the same routine, long working hours, morning coffee runs and often ordering out due to exhaustion, “The way she described it, it sounded normal. And that’s what worried me the most.” What her tests revealed shocked even her doctor, with alarming rates of liver enzymes, her ultrasound showed stage 3 fatty liver. The kicker is, she never touched alcohol in her entire life!
Dr Obaidur Rahman, ortho & sports surgeon, shared this story on his social media handle, to help spread awareness about nonalcoholic fatty liver disease (NAFLD) and the growing rates of the disease among young adults. NAFLD is also known as MASLD or fatty liver disease according to British Liver Trust.
While many people believe it is a disease on people who drink alcohol are susceptible to, this common misconception leads to many people overlooking the signs and symptoms, until it is too late.
What Are The Early Symptoms of Fatty Liver?
In the video caption, Dr Obaidur mentioned that the patient had faint yellow eyes, swollen legs that left deep impressions when pressed as well as slow unsure steps. He explained how these symptoms would be more in line with a patient decades older than the 29 year-old. According to UK National Health Services, most people who have it don't experience any symptoms and don't even know they have it. When symptoms do appear, they can include:
- Feeling very tired
- General discomfort or feeling unwell
- Pain in the upper right side of your abdomen, under your ribs
Can Bad Lifestyle Habits Cause MASLD?
MASLD is when fat builds up in your liver because of extra body weight, high blood sugar, high cholesterol or high blood pressure (John Hopkins Medicine). While doctors don't know the exact cause of MASLD, it is strongly linked to several common health issues.
Obesity: Carrying extra weight, especially around the belly, is a major factor.
Insulin resistance and Type 2 diabetes: This is when your body doesn't use insulin properly, causing blood sugar levels to rise.
Metabolic syndrome: A combination of conditions that include high blood pressure, high blood sugar, excess body fat around the waist, and abnormal cholesterol or triglyceride levels.
High cholesterol and high triglycerides: These are types of fats in your blood that, when too high, can contribute to liver fat.
Who Is At Risk for MASLD?
According to the American Liver Foundation, about 100 million people, which is around 25% in the US have been estimated to have MASLD. It is very common and certain factors make you more likely to get it. “Fuelled by sugar-laden “healthy” drinks, long hours of sitting, processed foods, and constant low-grade inflammation” Dr Obaidur details. Anyone could be at risk, some factors that determine that are:
- Are overweight, especially with a lot of fat around your stomach.
- Have a poor diet or don't get much physical activity.
- Have type 2 diabetes, high blood pressure, or high cholesterol.
- Are over 50 years old.
- Have polycystic ovary syndrome (PCOS).
What is the Treatment and Lifestyle Changes Needed for Fatty Liver?
The best way to treat MASLD is by making healthy lifestyle changes. These changes can help reduce liver fat and even repair some damage. They also lower your risk of other related health problems like heart disease and diabetes. Here's what you should do:
- Eat a healthy, balanced diet.
- Exercise regularly, aiming for at least 150 minutes a week.
- Lose weight if you are overweight.
Here's what you should avoid:
- Don't drink too much alcohol. Stick to the recommended limit of no more than 14 units per week.
- Don't smoke.
Russian President Putin Carries A 'Poop Suitcase' With Him: What Does Stool Reveal About One's Health?

Credits: AP and Canva
When Russian President Vladimir Putin travelled to Alaska last week for the Russia-US summit, reports noted a rather unusual detail. Along with his security entourage and official staff, Putin’s guards carried a special ‘poop suitcase’, a container meant to collect and secure the President’s fecal matter.
According to French magazine Paris Match, investigative journalists Regis Gente and Mikhail Rubin revealed that members of Putin’s Federal Protection Service (FPS) have been tasked for years with gathering his waste during foreign trips. The collected matter is then discreetly transported back to Russia.
The practice, which dates back to Putin’s rise to power in 1999, was also reported by BBC journalist Farida Rustamova, who noted that during past trips, including a visit to France in 2017, the Russian leader relied on portable toilets.
The reason? Preventing foreign intelligence agencies from accessing his stool, reports The Week. Experts speculate that even a small sample of bodily waste could provide sensitive information about a leader’s health.
While the security angle is unusual, it highlights an important fact: our poop says a lot about our health. Doctors routinely recommend stool tests, which can reveal infections, digestive issues, and even early signs of cancer.
What Does A Poop Tell About Your Health: Why Do You Need A Stool Test?
A stool test involves analyzing a sample of feces to detect potential health problems. Doctors use it to check for pathogens such as bacteria, viruses, or parasites that can make a person sick.
These tests can also detect hidden blood, fat, or DNA changes, clues that something more serious might be happening inside the body.
Healthcare providers often recommend stool tests when symptoms appear, such as:
- Blood or mucus in stool
- Persistent diarrhea
- Severe stomach pain or cramping
- Nausea or vomiting lasting several days
- Fever with digestive distress
- Conditions a Stool Test Can Detect
Stool analysis is a diagnostic tool because it offers a non-invasive look into the gastrointestinal system. Conditions that can be identified include:
Infections: Bacterial, viral, or parasitic infections often show up in stool cultures.
Colorectal cancer: Hidden blood or DNA mutations in stool can suggest early cancer.
Anemia: Blood loss in the digestive tract can signal anemia.
Inflammatory bowel disease (IBD): Chronic irritation of the digestive tract may be detected.
Gastrointestinal bleeding: Even small traces of blood can be found through stool testing.
Digestive disorders: Conditions like celiac disease, pancreatitis, or malabsorption syndromes leave clear signs in stool composition.
Also Read: What Is Alkaptonuria? The Rare Disease That Turns Your Pee Black – Here’s Why
Types of Stool Tests
Not all stool tests are the same. Doctors choose based on a patient’s symptoms and risk factors:
Fecal occult blood test (FOBT): Detects hidden blood in stool, which may indicate ulcers, cancer, or bleeding in the gut.
Fecal immunochemical test (FIT) and FIT-DNA: Checks for tiny amounts of blood and abnormal DNA that may point to precancerous conditions.
Tests for infections: Includes microscopic analysis, cultures, or DNA-based tests to identify harmful microbes.
What Stool Appearance Can Signal
Doctors often remind patients that simple changes in poop, its color, texture, or shape, can provide important health insights:
Oily or greasy stools: May mean fat isn’t being digested properly, possibly due to celiac disease or pancreatic problems.
Pencil-thin stools: If persistent, could signal an obstruction in the colon or irritable bowel syndrome.
Color changes: Food and gut bacteria often affect color, but black or bloody stool should never be ignored, as it may indicate bleeding or cancer.
Rocks and pebbles: Hard, lumpy stools point to constipation, often caused by dehydration, poor diet, or sluggish intestinal movement.
Why Does My Stomach Hurt After Eating? Unique Symptoms Of Peptic Ulcer Causing Burning Pain

Credits: Canva
We have all been there. You polish off a hearty meal, lean back with satisfaction and then comes that all-too-familiar burn in your stomach. For most people, the quick fix is to blame the food and pop an antacid. But what if that nagging pain is not just about what you ate?
According to Dr Akash Chaudhary, Clinical Director and Sr Consultant Medical Gastroenterology at Care Hospitals, Hyderabad, “That familiar burn after a meal might seem harmless at first. But when it starts showing up regularly, especially during long gaps between meals or waking you up at night, it could be your body signalling something more serious, like a peptic ulcer.”
What Is a Peptic Ulcer?
A peptic ulcer is basically a sore that develops on the inner lining of your stomach or the upper part of your small intestine. These sores form when the protective lining of the stomach wears down. “This kind of damage is often due to an H. pylori infection or the regular use of pain-relief medication like NSAIDs,” Dr Chaudhary explains. Without that protective cushion, the very acid that digests your food ends up irritating and damaging your stomach instead.
Unique Symptoms of Peptic Ulcer You Might Miss
Ulcers do not always announce themselves with big warning signs. Dr Pavan Reddy Thondapu, HOD of Medical Gastroenterology at Arete Hospitals, says that what often begins as “minor digestive discomfort, a burning sensation, early satiety, or bloating after meals can sometimes signal something more serious if ignored.”
Other tell-tale but easily overlooked signs include:
- Upper abdominal pain that keeps coming back, often worse after meals
- Unexpected nausea or changes in appetite
- Feeling unusually full too quickly (early satiety)
- Black, tarry stools or vomiting blood in advanced cases
- Unexplained tiredness, weight loss, or loss of appetite
Most people dismiss these symptoms as routine acidity or indigestion. But as Dr Chaudhary warns, “When the real cause goes unnoticed, ulcers can quietly progress, sometimes leading to bleeding or even a tear in the stomach lining.”
Why Antacids Do Not Always Cut It
Reaching for an antacid may calm the discomfort for a few hours, but it does not solve the underlying issue. “It is not uncommon for patients to self-medicate and ignore early symptoms, but that often delays recovery and increases risk,” Dr Thondapu points out. Antacids mask the pain, but the ulcer continues its work quietly in the background, setting the stage for bigger problems.
When to See a Doctor
The golden rule, if the burning pain keeps returning, especially after meals or early in the morning, is to not wait it out. According to Dr Chaudhary, “If someone experiences persistent burning pain after meals, they shouldn’t delay medical attention. What feels like a routine gastric issue may be a more serious condition silently progressing in the background.”
Red flag symptoms that warrant immediate medical evaluation include:
- Vomiting blood or black stools
- Difficulty swallowing
- Severe, persistent upper abdominal pain
- Unexplained weight loss or fatigue
How Doctors Get to the Bottom of It
Thankfully, diagnosing a peptic ulcer is not as scary as it sounds. “We usually diagnose peptic ulcers through simple procedures like an upper GI endoscopy or a breath test for H. pylori,” says Dr Thondapu. An endoscopy gives a direct look at the stomach lining, while non-invasive tests can quickly confirm an infection.
The Road to Healing
Ulcers are highly treatable once detected. Treatment usually involves:
- Acid-suppressing medications to give the stomach lining a chance to heal
- Antibiotics if H. pylori is detected
- Stopping or adjusting long-term NSAID use
- Simple but powerful lifestyle shifts
Dr Chaudhary emphasises that “with the right medicines and a few mindful shifts in daily eating habits, most people begin to feel better within weeks.”
Important Lifestyle Tweaks
Treatment is not just about pills; how you live day to day plays a big role in preventing recurrence. Dr Thondapu recommends:
- Eating meals on time instead of long gaps or binge-eating sessions
- Cutting back on alcohol and tobacco
- Avoiding overly spicy, oily, or processed foods
- Managing stress through exercise, yoga, or mindfulness
These shifts help protect the stomach lining and keep acid levels in check, making ulcers less likely to return. In a nutshell, stomach pain after meals does not always mean you overdid it on the food. Sometimes it is your body’s way of flagging a deeper issue. As both experts stress, ignoring persistent burning pain or bloating is not worth the risk. Early diagnosis makes ulcers easy to treat, while delay can lead to serious complications.
Watch: The Exact Moment A Human Embryo Implants In Real-Time
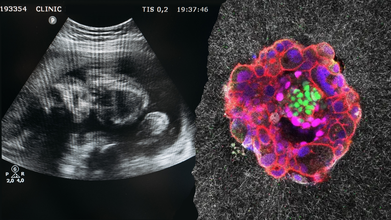
Credits: Canva/Institute for Bioengineering of Catalonia (IBEC)
For the first time in history, scientists have captured on film the moment a human embryo implants itself—an elusive biological milestone that has long been considered a “black box” in early human development. The breakthrough, published in Science Advances, not only offers a rare window into the earliest stages of life but also carries profound implications for fertility science and reproductive medicine.
Before any of us became who we are, we were once a fragile cluster of cells adrift, searching for a home inside the uterus. That critical moment—when the embryo anchors itself into the uterine lining, is known as implantation. It is a make-or-break step for pregnancy.
Yet until now, scientists had little more than snapshots of the process. Ultrasounds only detect pregnancies weeks later, and the act of implantation itself occurs deep within the womb, hidden from view. Roughly 60 percent of pregnancy losses occur during or shortly after implantation, making it a critical bottleneck to life.
Dr. Samuel Ojosnegros, senior author and bioengineer at the Barcelona Institute of Science and Technology (BIST), explains the importance, “For the first time, we’ve been able to watch human embryo implantation unfold dynamically. We’ve opened a window into a stage of development that was previously hidden.”
How Scientists Filmed the "Hidden" Process?
Since it would be too risky to disrupt implantation inside a living uterus, researchers had to recreate the process in the lab. Using embryos donated by couples undergoing IVF, Ojosnegros and his team built a model of the uterine environment.
The embryos were placed into a collagen-based gel designed to mimic the structure and nutrients of uterine tissue. With advanced microscopy and fluorescence imaging, researchers recorded time-lapse videos showing the embryos penetrating the gel.
What they saw was surprisingly forceful. Unlike mouse embryos, which invaded only superficially, human embryos drilled deep, burrowing aggressively and reshaping the surrounding environment.
The footage revealed the embryo not as a passive passenger but as an active architect, exerting mechanical force, releasing enzymes to break down tissues, and remodeling its new home.
Watching The Surprising Force of Early Life
Implantation is not a delicate nudge. It’s invasive. The embryo pulls surrounding collagen fibers toward itself, digs deep into the tissue, and begins to prepare the foundation for the placenta.
“The embryo opens a path through this structure and begins to form specialized tissues that connect to the mother’s blood vessels,” Ojosnegros explains. “It is a surprisingly invasive process.”
In fact, this burrowing behavior underscores how different human embryos are from animal models. For decades, most implantation studies have relied on mice. But what happens in mice only loosely reflects the human experience. This research shows that human embryos go much further, both physically and biologically.
Why The “Goldilocks zone” Of Uterus Plays A Critical Role?
The study also raises new questions about the uterus itself. The maternal environment is far more than a passive host. The human uterus contracts one to two times per minute on average, and the frequency of these contractions changes throughout the menstrual cycle.
Some research suggests that too many or too few contractions on the day of embryo transfer in IVF can reduce the chances of success. The right rhythm, what some scientists call the “Goldilocks zone” of contractions may improve implantation rates.
Amélie Luise Godeau, lead author of the study, says the embryo appears to interact with these external forces as it burrows in, “We hypothesize that contractions occurring in vivo may influence embryo implantation.” Understanding this delicate rhythm between embryo and uterus could prove pivotal for advancing fertility treatments.
What Are The Implications for Fertility Science?
Implantation failure is one of the main reasons IVF doesn’t work. Despite technological advances, many embryos fail to attach, leaving patients and clinicians frustrated. By uncovering the mechanics of implantation, this research may open new paths to improve success rates.
Through their spin-off company Serabiotics, Ojosnegros and his colleagues are already working with pharmaceutical partner Grifols on protein supplements that could enhance implantation in clinics.
The model developed in the lab also offers flexibility. Since the matrix of collagen can be manipulated, researchers can experiment and see how embryos react under various conditions, nutrients, or drugs. That is, researchers can observe not just why implantation fails but also how to make it succeed.
What Are The Ethical and Biological Limits?
It's also worth noting that the model employed in this study is not a complete imitation of the uterus. It doesn't have human uterine cells, so the interaction is only half the story. Nevertheless, this restriction is also a chance—it enables scientists to manipulate the environment in ways that are impossible within the human body.
Ethically, the study stayed within the strict rules, employing donated embryos with informed consent. None of the embryos were brought to a point beyond reproductive law and ethical boundaries.
Since decades ago, the process of implantation has been told as one of biology's biggest mysteries. Now, thanks to this live footage, scientists are reauthoring the book on how life gets started.
It's not merely intellectual curiosity. For the millions of individuals around the globe who are infertile, the results might mean more targeted fertility treatments and better IVF success rates. For researchers, it provides a new method to explore the very beginnings of human existence.
Ojosnegros and his colleagues hope to refine their model further, study how embryos engage with the maternal environment, and look for signs that might some day prevent early pregnancy loss.
What this research establishes is that implantation is not a passive handoff between embryo and uterus. It's an active, forceful, highly coordinated process in which both partners—the embryo and maternal tissue are both key players.
© 2024 Bennett, Coleman & Company Limited

