- Health Conditions A-Z
- Health & Wellness
- Nutrition
- Fitness
- Health News
- Ayurveda
- Videos
- Medicine A-Z
- Parenting
- Web Stories
Plastics Shouldn't Be Near Your Genitals, Here's What Makes Them Toxic And Fatal

Plastics have revolutionized the way we live, offering convenience and durability in nearly every facet of modern life. From food containers to personal care products, plastic has become an inescapable part of daily routines. However, when it comes to our health- particularly reproductive health—plastic’s ubiquitous presence might pose serious risks.
The issue takes on added urgency when discussing the proximity of plastics to genital organs, where heightened vascularity increases absorption. This absorption can lead to a range of reproductive and fertility issues, including polycystic ovary syndrome (PCOS), endometriosis, and even cancer.
Plastic is everywhere-in bowls, wraps, bottles, and bags used to store foods and beverages. Its prevalence often makes it difficult to question its safety. But over recent years, concerns have grown about the potential harm of exposing our bodies to plastics, particularly in sensitive areas such as the genital region.
Take menstrual products, for example- a typical menstruating individual will have an estimated lifetime use of 11,000 tampons, sanitary pads, panty liners, and more, equaling five years of exposure if they applied them continually. This level of contact alone is a good reason why knowing the dangers of plastics in such products matters.
Hidden Chemicals in Menstrual Products
Evidence uncovered by research about the chemical content of menstrual products is quite alarming. Such chemicals include:
1. Phthalates (Plasticizers)
The chemical has been found to increase the flexibility of plastics, and it is known as an endocrine disruptor.
2. PFAS (Perfluoroalkyl and Polyfluoroalkyl Substances)
Such chemicals are referred to as "forever chemicals," which have been used due to their non-stick and water-resistant properties but have been linked with hormonal imbalances.
3. Volatile Organic Compounds (VOCs)
Often present in fragrances or as off-gas from many products, VOCs can interfere with the body's natural regulatory systems.
These chemicals interfere with the endocrine system, which is a network that helps to regulate sexual development, metabolism, mood, sleep, and much more. Since the genital area has an increased absorptive capacity, intimate contact with these substances can be particularly worrying.
Health Effects of Chemicals Associated with Plastics
These chemicals can cause a chain reaction of health problems through absorption by the vaginal lining or skin.
Fertility Problems
Phthalates and PFAS have been associated with decreased fertility as they affect hormone production and balance.
Polycystic Ovary Syndrome (PCOS)
Studies indicate that endocrine-disrupting chemicals can worsen hormonal imbalances, which can contribute to PCOS, a common cause of infertility.
Endometriosis
Prolonged exposure to these plastics has been linked to chronic inflammation and abnormal tissue formation, symptoms often characterized endometriosis.
Cancer Risk
Exposing the reproductive system for long periods through plasticizers and other toxic materials increases cancer risk, in this case, ovarian and cervical cancers.
Arsenic and Lead in Menstrual Products
A recent pilot study has added another layer of concern. The study has found traces of arsenic and lead in both organic and non-organic tampons. Those levels were small, though, and it is worth reminding that no amount of lead exposure is considered safe: according to the US Environmental Protection Agency.
These findings raise critical questions about the regulation of menstrual products. While the US Food and Drug Administration (FDA) categorizes tampons and pads as medical devices, the regulatory framework does not always extend to every chemical component used in manufacturing.
What makes the genital region specially vulnerable to the effects of plastics and their associated chemicals? It is because of the anatomy of this area. The genital area is very vascular, or rich in blood vessels just below the surface. That's what increases absorption, giving chemicals easy access to the bloodstream.
Unlike the digestive system, where enzymes and acids can break down harmful substances, the vaginal and genital tissues lack these protective barriers. As such, harmful chemicals in tampons, pads, and other plastic-containing products have a direct pathway to systemic circulation.
Are there any Safer Alternatives to Use?
Given the growing body of evidence, individuals can take steps to reduce their exposure to harmful plastics:
- Opt for Organic Products: Select tampons, pads, or menstrual cups that are labeled organic or chemical-free.
- Avoid Fragranced Products: Fragrances contain VOCs and phthalates. Choose unscented products.
- Check Certifications: Opt for products certified by organizations such as GOTS (Global Organic Textile Standard) or OEKO-TEX.
- Limit Plastic Use in Intimate Areas: Avoid plastic-based contraceptives, lubricants, and other personal care items in favor of safer, non-toxic alternatives.
In many parts of the world, regulation of menstrual and intimate care products remains insufficient. Advocacy for stricter standards is needed to ensure that harmful chemicals are either eliminated or disclosed. Transparency in product labeling and robust testing of materials can help consumers make informed decisions about their health.
The convenience of plastic comes at a hidden cost, especially when it comes into contact with the most sensitive areas of our bodies. The risks of plastic-related chemicals, from endocrine disruption to cancer, are too significant to ignore. By understanding these dangers and advocating for safer alternatives and stricter regulations, we can protect not just our reproductive health but our overall well-being.
Menstrual Products as a Source of Environmental Chemical Exposure: A Review from the Epidemiologic Perspective. Curr Environ Health Rep. 2022
Asthma Risk Could Increase For Women Who Work Night Shifts: Study

(Credit-Canva)
As our economy and connectivity evolved, many companies and professionals have moved onto working 24/7. To make this happen, people have come up with shift schedules that will allow some people to work during the day, while others work night shifts. However, an issue people face is that night shifts are unconventional and can impact your health. It changes the way your body functions and can have a severe impact on your body.
A study published on June 16 in ERJ Open Research found that women who consistently work night shifts have a 50% increased risk of moderate to severe asthma compared to women who workday shifts. Interestingly, this connection wasn't observed in men.
Researchers from the University of Manchester in the U.K., explained that while the study doesn't pinpoint why this link exists, it might be due to disruptions in the body's natural clock, which can affect hormone levels.
Hormonal Connections and Increased Risk
The idea that hormones play a role is supported by a key finding: postmenopausal women on the night shift who were not using hormone replacement therapy (HRT) saw their risk of moderate to severe asthma nearly double.
Researchers noted that asthma already affects women more severely than men, leading to higher hospitalization and death rates for women. Previous studies have also linked night shift work to more severe asthma in general. This led the team to investigate if night shifts would further increase asthma risk specifically for women.
Study Details and Findings
The study tracked the health of nearly 275,000 working individuals in the U.K. Biobank, a large health research project. Over 5% of these workers had asthma, with 2% suffering from severe asthma requiring a rescue inhaler.
The results clearly showed that women working only night shifts had 50% higher odds of moderate to severe asthma. This risk jumped to 89% higher for postmenopausal women on the night shift who were not taking HRT.
Researchers suggested that HRT might offer some protection against asthma for night shift workers, but he stressed that more research is needed to confirm this. He also speculated that higher testosterone levels in men might protect them from asthma, as testosterone has previously been linked to asthma protection.
Unanswered Questions and Future Steps
While the study highlights a strong association, it can't definitively prove that night shifts cause asthma in women. Other factors, like the different types of jobs men and women hold on night shifts, could also contribute to the risk.
Experts pointed out that it's often not easy for workers to simply change their shifts. She emphasized the need for further research to fully understand this link and to find ways to reduce the risk for women who work night shifts.
What Are Some Other Long-Term Effects Of Night Shifts?
Shift work, especially at night, seriously disrupts your body's natural 24-hour cycle, called the circadian rhythm, leading to various health challenges. Here are some long-term health issues that may arise from it, according to UCLA health.
Cancer
Disrupted circadian rhythm impacts cell function, DNA repair, and cell death, potentially leading to cancer, as reported by the National Toxicology Program. Reduced melatonin from irregular light/dark exposure hinders cell repair, making cancer progression easier.
Cardiovascular Disease
Working unusual hours increases heart disease and stroke risk. A European Society of Cardiology-linked study found women with five-plus years of rotating night shifts faced higher death risk, tied to stress, high blood pressure, and metabolic factors.
Gastrointestinal Disorders
Shift workers often experience digestive issues like abdominal discomfort, constipation, diarrhea, and IBS. These gut problems stem from sleep deprivation and unhealthy, processed food diets common in shift work, altering gut bacteria.
Mental Health Disorders
Nonstandard hours make maintaining relationships difficult, leading to isolation, stress, depression, and anxiety. A large study in The Lancet Psychiatry found shift work directly linked to higher risks of depression and anxiety, increasing with shift frequency.
Metabolic Disorders
Shift work disrupts circadian rhythm and hormones, raising risks for obesity, metabolic syndrome, and Type 2 diabetes. It's linked to higher BMI, hormonal imbalances affecting appetite/weight, and unhealthy lifestyle choices like smoking and poor diet.
Dementia Caregivers Have A Higher Chance Of Getting Dementia Themselves

(Credit-Canva)
Taking care of a sick person is a taxing job not many people can fullfill. Patients with mental health issues like dementia require specialized care and not everyone is equipped to handle these situations. Many times, people with dementia have emotional outbursts, difficulty communicating as well as doing normal lifestyle activities. Caring for people with dementia requires a team of people, sometimes 24/7 care with rotations for staff, so that the patient is not left unattended for an extended period of time. However, does this extensive routine affect the caregiver’s health? A new study has found concerning future implications for dementia caregivers.
Caring for someone with dementia might put caregivers at higher risk for their own brain aging and future dementia, a new study suggests. This is largely due to certain lifestyle factors.
Caregivers' Hidden Risk
A recent report from the Public Health Center of Excellence on Dementia Caregiving, released on June 12, found that nearly 3 out of 5 dementia caregivers (59%) have at least one risk factor that increases their chances of developing dementia over time. Even more concerning, about 1 in 4 (24%) have two or more of these risk factors.
Matthew Baumgart, senior vice president of health policy for the Alzheimer's Association, called this analysis a "wake-up call." He noted that caregivers are often so focused on their loved ones that they neglect their own health. This highlights a critical need for public health strategies to support these vulnerable individuals.
Key Risk Factors Identified
Researchers analyzed health data from caregivers across 47 states in 2021 and 2022. They found that caregivers were more likely than the average person to have five things that aren't good for brain health:
Smoking
Caregivers were 30% more likely to smoke. Smoking is bad for your overall health, including your brain.
High Blood Pressure
They were 27% more likely to have high blood pressure. High blood pressure can damage blood vessels, including those in the brain.Poor Sleep
21% more likely to say they didn't sleep well. Not getting enough good sleep can affect how your brain works and ages.Diabetes
They had a 12% higher chance of having diabetes. Diabetes can lead to problems with blood flow and brain function.Obesity
Caregivers were 8% more likely to be overweight or obese. Being overweight is linked to many health problems, including some that affect the brain.Interestingly, there was one good piece of news: caregivers were actually less likely to be inactive (meaning they moved around more) compared to others. This might be because looking after someone with dementia often involves a lot of moving around.
Younger Caregivers Face Greater Vulnerability
This part focuses on younger caregivers, and the news isn't great for them. The study found that younger people who care for someone with dementia are at an even higher risk.
- 40% more likely to have many of these risk factors at once, compared to other people their age.
- 86% more likely to smoke. That's a huge difference!
- 46% more likely to have high blood pressure.
- 29% more likely to get less than six hours of sleep each night compared to their friends who aren't caregivers.
The researchers explained that knowing which groups of caregivers are most at risk, public health officials can better plan and offer help. Instead of a one-size-fits-all approach, they can create specific programs and resources for the groups that need it most.
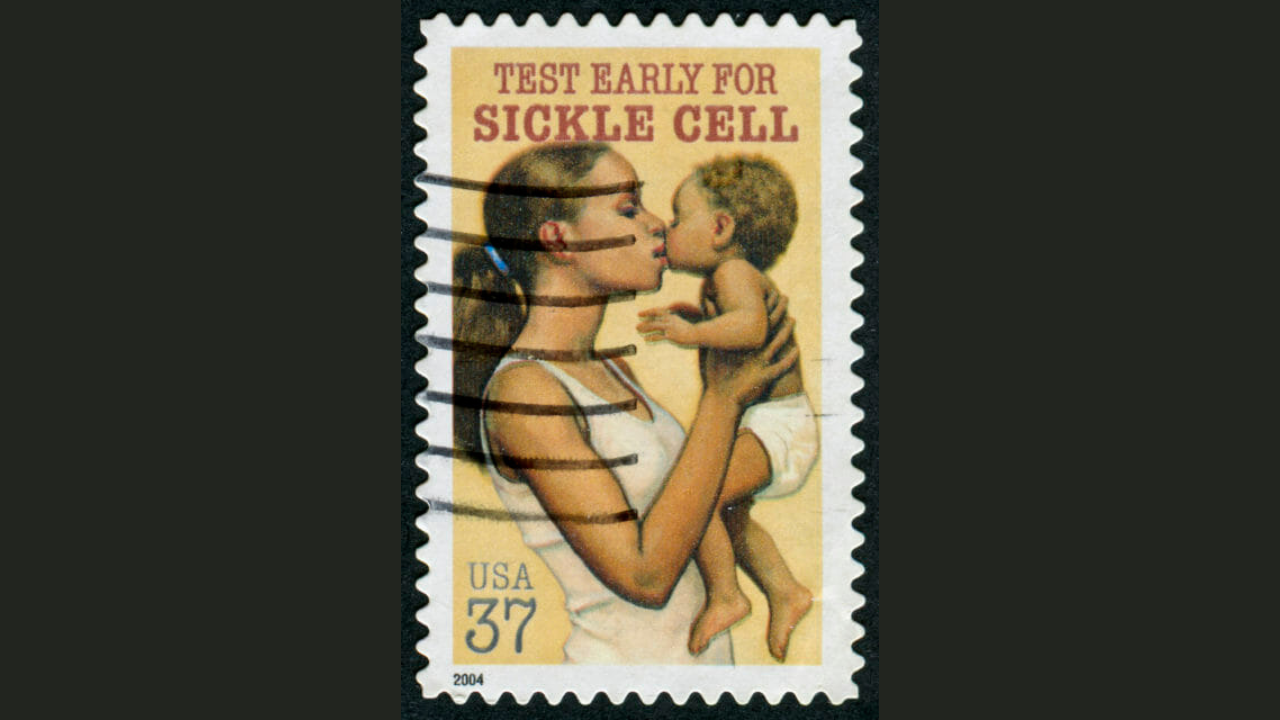
Sickle Cell Disease: Tracing The History Of The First Ever Genetic Disease To Be Diagnosed

Credits: PIB
A parasite that causes malaria is halted by sickle cells and makes people who carry the sickle cell trait more resistant to the disease. This is why sickle cell trait also occurs more in people who live in tropical and sub-tropical regions where cases of malaria were or still is common.
It comes from the copy of an abnormal sickle or the HBB gene and one copy of the normal HBB gene. The gene is an evolutionary response to malaria, where humans begin to develop an abnormal HBB gene and pass it onto to the next generation.
The "Black Disease"
The earliest documentation of sickle cell symptoms in medical texts could be found from the 1870s. However, it had not been formally identified until in 1910. when the first case was detected in the United States. The first case of sickle cell disease or SCD in the US was in 1904, when Walter Clement Noel, a 20-year-old dental student from Grenada, sought care for anemia at Chicago Presbyterian Hospital, where he met Dr James B Herrick. Dr Herrick was a cardiologist and professor of medicine and he was assigned noel who had experienced recurrent episodes of "muscular rheumatism" and "bilious attacks" over a period of 3 years.
This case was assigned to an intern Dr Ernest E Irons by Dr Herrick. Dr Ernest performed initial blood work on Noel and observed the unusual sickle-shaped red blood cells in the sample under the microscope. This is when Dr Herrick was told about it, leading to him publishing the first documented case study of SCD, titled, "Peculiar Elongated and Sickle-Shaped Red Blood Corpuscles in a Case of Severe Anemia."
However, the name, sickle cell anemia, was not coined until in 1922, by Vernon Mason. It was also the first diagnosed genetic disease and the first to be linked to the hemoglobin protein.
But, how did it gain the name "Black Disease"? This is because the disease often disproportionately affected Black Americans in the US, which caused racial bias and prevented people with sickle cell from receiving quality care.
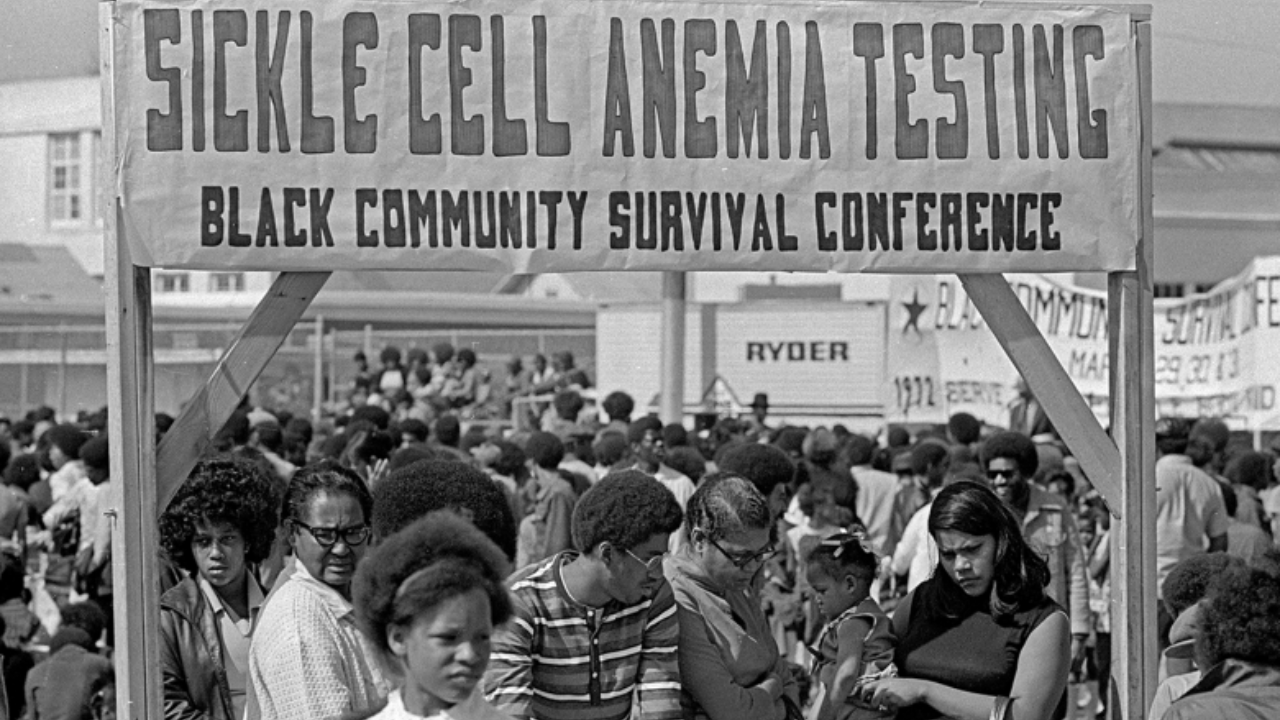
In response to this, in the 1960s, the Black Panther Party worked to expand community-based care for education and treatment of this disease. This was part of their initiative to tackle the sickle cell, which received little to no attention because it mostly affected a large part of Black community.
While Herrick may have described the first known case in the US, SCD did exist for generations in African and Mediterranean descent, due to the regions being prone to diseases like malaria. In African medical literature, it was known as "ogbanjes", which loosely translated into "children who come and go" as the infants born with this disease had a high mortality rates. One of the first records, as is also noted by the Sickle Cell Association from Africa is from a Ghanian family in 1670.
A Groundbreaking Discovery
In 1927, scientists Hahn and Gillespie made a discovery that reshaped our understanding of blood disorders. While studying red blood cells in a low-oxygen environment saturated with carbon dioxide, they observed a curious phenomenon: the cells twisted into sickle shapes—not just in patients with sickle cell disease (SCD), but sometimes in people without any symptoms at all.
This puzzling observation hinted at an invisible carrier state and eventually led to the identification of what we now call the sickle cell trait.

Fast-forward to the late 1940s and early 1950s, and the pieces of the puzzle began falling into place. In 1949, two scientists working continents apart independently uncovered the genetic blueprint of SCD.
Col. E. A. Beet, a military physician stationed in what is now Mozambique, published his findings in an African medical journal. Around the same time, Dr. James V. Neel at the University of Michigan released a parallel study in the journal Science. Both revealed that SCD follows an autosomal recessive inheritance pattern—meaning the disease only occurs when a person inherits two copies of the mutated gene. Those with just one copy? They carried the trait, but not the illness.
Together, their work laid the foundation for our modern understanding of genetic inheritance and reshaped how we screen for and manage sickle cell disorders today.
© 2024 Bennett, Coleman & Company Limited

