- Health Conditions A-Z
- Health & Wellness
- Nutrition
- Fitness
- Health News
- Ayurveda
- Videos
- Medicine A-Z
- Parenting
- Web Stories
Probiotics Can Keep You ‘Happy, Healthy And Wise’ Reveals Breakthrough Study
We have all heard the phrase ‘I have a gut feeling’ or ‘gut-wrenching’ experience and other variations of gut and our feelings. However, are they just phrases or do they hold some truth to them. There have been many studies that show how your mental health affects your gut and vice versa.
People have expressed how when they are scared or angry or anxious they often experience an upset stomach with other people also experiencing some sort of sudden reaction with heightened feelings whether it is a lurch or a sudden ‘drop’.
So, if these things affect your gut, then can helping your gut make you feel better? A new study shows that a happy gut could mean a happy you.
A recent study published in the npj Mental Health Research found that people who took probiotic supplements, which contain live microorganisms, reported feeling better emotionally over a month. Interestingly, these probiotics didn't seem to change people's overall mood as measured by standard psychological questionnaires.
The study explained that "negative feelings" can mean different things to different people. She believes this finding is significant because it suggests probiotics might help with whatever an individual interprets as a negative emotion, whether it's anxiety, sadness, or tiredness.
What Are Probiotics?
The types of microbes that thrive in our gut are largely determined by the food we eat and what those microbes do because of this, companies and researchers have developed probiotic supplements containing specific strains of live microorganisms. The goal is to see if these supplements can improve health. Probiotics, usually sold in capsules or pills, are defined as live microorganisms that provide a health benefit when consumed in adequate amounts. These beneficial microbes are also naturally present in some fermented foods like yogurt.
How Do Probiotics Directly Affect Your Mood?
The study involved 88 healthy individuals. For one month, half of the participants took a daily probiotic supplement, while the other half took a placebo (a dummy pill with no active ingredients). The probiotic used was a mix of nine different bacteria strains found in the Ecologic Barrier mixture from a Dutch company. Participants mixed a sachet of these bacteria with lukewarm water each day.
At the beginning and end of the study, everyone completed ten different questionnaires about their emotions and how they processed them, as well as one about any bowel issues. Participants also rated how positive or negative they felt each day on a scale and provided stool samples.
The results showed that both the placebo group and the probiotic group:
- Scored similarly on the mood questionnaires.
- Reported similar levels of good mood each day.
However, the group that took probiotics said their negative mood went down after just two weeks. This difference between daily feelings and the questionnaires suggests we might need better ways to measure mood changes.
How the Gut And Brain is Connected?
Harvard Health Publishing explains that our gut and our brain are closely linked, so much so that how we feel emotionally can directly affect our stomach and intestines, and problems in our gut can also send signals to our brain, influencing our mood. Think about how stress can give you "butterflies" or how worry can make you feel sick to your stomach – these common feelings show this strong connection because of this, when our gut is upset for no clear physical reason, it's important to consider how our stress and emotions might be playing a role, as our mental state can actually change how our digestive system works and how sensitive we are to pain in our gut.
Medical Memoir: History of Hysteria, Why Doctors Once Blamed the Moon and the Uterus for Women’s Mental Health
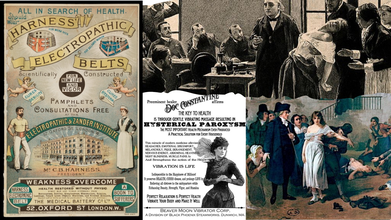
(McGill University, Wellcome Collection, Journal of Victorian Culture)
To reach the medical knowledge we have today, we have gone through many theories and phases, trials and errors to now be accurate with our information and remedies. However, it has only been quite recently that mental health is being taken seriously. So how was it dealt with in the past?
One big example of it is something that was debunked quite recently. A belief that the moon influenced people’s moods, to the point that it led people into hysteria.
The idea is ancient, tied to folklore about werewolves and other creatures, and it continues to influence modern belief. For instance, a surprising number of doctors and nurses—up to 80% in one study—still believe the moon affects moods, even though there's no solid science to support it. This enduring myth is a powerful example of how historical misdiagnoses, especially those related to women, have shaped our understanding of health.
History has been a witness to many medical anomalies, surprising ailments and even more astounding treatments. Many of these treatments were for women, which is not the surprising part as history has shown how medical research for women was pushed aside and overlooked to the point that basic illnesses and conditions in women had no cure or proper treatment until recently.
If you are someone who enjoys history, or simply someone who likes reading, then you may know about the word ‘Hysteria’ or ‘Hysterical’. In modern English, it is used to define being frantic or out of control, but did you know, this used to be a formal diagnosis, even thought of as something physical by historical medical practitioners. It was a major source of debate and a prime example of how women's health was misunderstood and often mistreated.

How Has History Treated Women’s Health?
According to the McGill University, The idea of hysteria dates back to ancient Egypt and Greece. Physicians in these societies believed that a woman’s uterus was the source of a wide range of health issues. In ancient Greece, it was believed that the uterus could actually "wander" around the body, pressing on other organs and causing all sorts of symptoms, from anxiety and fainting to insomnia and fevers. This idea was so widespread that the term "hysteria" comes from the Greek word hysteria, which means uterus. Doctors would try to coax the uterus back into place using "good smells" near the vagina and "bad smells" near the mouth.
During the Middle Ages, the understanding of hysteria took a dark turn. The "scientific" view of the wandering uterus was often replaced by a demonological one. Mental illness in women was seen as a sign of sin or a pact with the Devil. Women with symptoms of hysteria were often accused of witchcraft and subjected to exorcisms, torture, and even death. This period marked a major step backward in the treatment of mental health.
Did History Have A Cure For Hysteria?
Later, a Roman physician named Galen offered a different theory. He believed that hysteria was caused by a woman's body holding on to "female seed" or "menstrual blood" instead of releasing it. The solution, he thought, was to get rid of these fluids. Because of this belief, doctors often recommended marriage and regular sex as a cure. For women who were unmarried, widows, or simply couldn't have an orgasm from sex, midwives were sometimes brought in to manually stimulate them. The doctors believed that without this "release," women would suffer from anxiety and other problems.
Was Hysteria Considered A Mental Health Issue?
The Renaissance and the Enlightenment brought a renewed focus on science. Physicians like Thomas Willis and Thomas Sydenham began to suggest that hysteria was linked to the brain and nervous system, not the uterus. This was a revolutionary idea because it meant the condition could affect both men and women, challenging the old belief that it was an exclusively female disease.
In the 19th century, French neurologist Jean-Martin Charcot further proved this point by systematically studying hysteria in both sexes. His work paved the way for Sigmund Freud, the "father of psychoanalysis." Freud believed that hysteria was a psychological disorder caused by repressed emotional trauma, not a physical problem. His new approach shifted treatment from physical remedies to talking therapy.
Did Men Also Experience Hysteria?
According to the Clinical Practice & Epidemiology in Mental Health journal, until the 20th century, hysteria was rarely diagnosed in men. But during World War I, military doctors saw a rise in "shell shock," a condition with symptoms like paralysis and tremors. Many doctors realized these were actually hysterical symptoms, which led to the first widespread recognition of male hysteria. This provided a way for soldiers to escape the battlefield without being seen as cowards.
Studies during World War II also showed a clear difference in how soldiers from different cultures expressed mental distress. For example, British soldiers were more likely to show symptoms of anxiety, while Indian soldiers more often showed physical symptoms of hysteria. This highlighted a key idea: how people express their emotional pain is often shaped by their culture.

Decline of Hysteria in the West
In the second half of the 20th century, psychiatric data showed a dramatic drop in hysteria diagnoses in Western countries. At the same time, there was a sharp increase in diagnoses of anxiety and depression. Doctors believe this shift is linked to "Westernization" and a new emphasis on individualism. In Western societies, people are more likely to see themselves as masters of their own destiny. This can lead to feelings of self-blame and unworthiness when things go wrong, which are classic symptoms of depression. In contrast, in societies with strong group ties, people may be more likely to blame external factors like evil spirits or social pressures for their problems, which could express as physical, hysterical symptoms.
Is ‘Hysteria’ Still Considered A Mental Disorder?
Although hysteria is no longer a diagnosis, its history continues to be seen in modern-day medicine. Researchers who studied patient records from two old hospitals in Sardinia, Italy, found that doctors in the late 1800s and early 1900s were still using ancient treatments for hysteria. For example, they used herbal remedies, purgatives, and even leeches. In some cases, patients were confined to asylums for life with a diagnosis of hysteria, showing that even with advances in medicine, old and harmful beliefs about women's health were slow to change.
Youtuber Shares How She Went Into A Coma 2 Weeks After Giving Birth: Can Complication During Childbirth Become Deadly?

(Credit-Mrkate/Instagram)
Childbirth and pregnancy are one of the most hardest things a human body can go through. Although things have gotten easier, in terms of care and ensuring the mother’s safety while giving birth, the small percentage of mortality looming overhead does not disappear. ‘But it’s just the pregnancy and childbirth that’s the tough part, right? Once you get past that you no longer have to worry about other complications.' But that is not entirely true either and facing this reality, the YouTube duo, Mr. Kate, shared their birth story.
You may know Mr. Kate from their YouTube channel, that has amassed over 3 million subscribers, sharing their life, stories and other fun challenges. In a recent video, they shared their birth story and the unexpected challenges they faced.
In the video, Kate Albrecht and Joey Zehr, welcomed their second baby together in a home birth. Their first child was born in 2019 in the hospital and Kate hoped for her second and last pregnancy she could experience a natural homebirth. In an interview with the People, she shared how she wanted to do a home birth because it sounded “really magical”, and since they chose to have their first birth at hospital, she thought for her second and last pregnancy, she was ready to challenge herself with a home birth.
How Do Home Births Work?
According to the National Health Services (NHS) when cosidering a home birth, one should be very careful and make sure they are making a well-informed choice. They explain that during a home birth, a community midwife, will come to look after you during the birth and a short while after the baby is born, they will assist you in different things along with making a birth plan suitable for the mother’s care.
Kate explained that she and Joey engaged in "dual care," seeing both a midwife and an OB-GYN to ensure a safe delivery. The birth of their daughter, Mars, was a success, and the baby was born en caul (still inside the amniotic sac), a rare and significant event.
Following the birth, Kate was prepared for a smoother recovery than her first. However, it was just 2 weeks after she gave birth after which a medical emergency arose.

Can Pregnancy Complications Occur Weeks After Giving Birth?
After giving birth, Kate felt exhausted and had severe headaches and a bad backache. When she went for her check-up, doctors told her these symptoms were normal for someone recovering from childbirth. However, two weeks after Mars was born, Kate suddenly collapsed at home. When her husband Joey found her, she was unconscious and having a seizure.
Joey called 911, and paramedics quickly figured out that Kate was suffering from eclampsia, a dangerous condition that can cause seizures. It's connected to preeclampsia, a blood pressure issue that can happen during pregnancy. In Kate's case, it happened after she gave birth, which is rare. Even though she had been perfectly healthy during her pregnancy and her tests for preeclampsia were negative, her body had developed the condition in the weeks after her baby was born.
Can Childbirth Complications Lead To Coma?
At the hospital, doctors put Kate in a medically induced coma to protect her brain. Scans showed she did not have any brain bleeding, which was a huge relief. However, they did find a blood clot in a vein near her kidney. This explained the terrible back pain she had been feeling.
After a few days, Kate was finally able to wake up from the coma. She had to stay in the hospital for a little while, but she was eventually sent home with medication to help prevent future blood clots.
Kate and Joey decided to share their story to help other parents. They learned that postpartum eclampsia can happen up to six weeks after a baby is born. They want everyone to know that even if you have a healthy pregnancy, you still need to be aware of the signs of this condition and get medical help for any unusual symptoms after giving birth.
Although the complications were scary, Kate and Joey are happy and thriving with the new addition to their family. Their fans and well-wishers commented supporting the couple and advocating how important postpartum care is.
78-Year-Old Retired Professor Shared His Secret To Keeping 'Razor Sharp' Memory Even As He Ages

(Credit-Canva)
It is no secret that as we age our memories decline and fade. We have all seen our grandparents age and slowly lose the agility they had when we were kids, how they remembered to bring our favorite sweets and foods, and tell us stories of their youth. However, this is no longer easy for them as their minds take an obvious turn for the worse.
We all wish to see our aging elders live their days peacefully and healthily and one of those aspects is their memory. However, it doesn’t always have to be this bleak, there are many people who have aged and also kept their minds strong, and this 78-year-old professor is giving everyone a run for their money.
Anthony D. Fredericks, a former education professor at York College of Pennsylvania, shared with CNBC, his simple habits that he credits with keeping his brain in top shape.
5 Habits That Keep Your Brain Strong Over 70
Never Stop Learning
Your brain loves a challenge. Whether you're learning a new language, taking a class, or doing a crossword puzzle, challenging your mind helps it form new connections. Research has even shown that staying mentally active over the years can lower your risk of dementia. As Fredericks says, reading widely and staying curious keeps your mind engaged.
Stay Social
Being lonely doesn't just make you sad; it can also slow your brain down. Having strong connections with friends and family has been linked to a lower risk of memory problems, lower blood pressure, and a longer life. An old professor, Fredericks, stays sharp by regularly spending time with friends, volunteering, and seeing family, which he believes helps his mind and overall well-being.
Keep Things Organized
Setting goals and staying organized can make your brain work better. When you organize your tasks, you activate the part of your brain responsible for planning and making decisions. Fredericks uses a simple, color-coded sticky note system to keep track of his daily tasks, a habit he says has made a huge difference.
Stay Active
Physical exercise is very important for a healthy brain. It increases blood flow to the brain, which helps create new brain cells and strengthens connections between them. Experts recommend at least 150 minutes of moderate activity each week, like brisk walking, swimming, or gardening. Fredericks himself swims and walks regularly to stay active.
Eat and Drink Smart
What you eat has a big impact on your brain health. A healthy diet, along with drinking plenty of water and getting good sleep, can help keep your mind sharp. Fredericks makes sure to eat heart-healthy foods like berries, leafy greens, and salmon. He also drinks at least eight glasses of water and gets at least seven hours of sleep every night.
Other Tips To Keep Your Mind Sharp As You Age
According to the National Institute of Aging, there are many ways to keep your mind as healthy as your body when you age. Including the points mentioned above by the professor, here are some additional tips to keep your memory strong.
Manage Blood Pressure
Keeping your blood pressure in a healthy range is not just good for your heart; it's also good for your brain. High blood pressure in middle age can increase the risk of memory and thinking problems later on. Get your blood pressure checked every year, and talk to your doctor about exercise, diet changes, or medicine if needed.
Address Health Problems
Conditions like a stroke or depression can seriously affect your brain. Getting the right treatment for these issues can help prevent or delay mental decline.
Be Smart About Medications
Some medicines can cause confusion or memory loss, especially in older people. Always talk to your doctor if you have concerns about your medications and never stop taking a prescribed medicine without their advice.
© 2024 Bennett, Coleman & Company Limited

