- Health Conditions A-Z
- Health & Wellness
- Nutrition
- Fitness
- Health News
- Ayurveda
- Videos
- Medicine A-Z
- Parenting
- Web Stories
Ulcers vs Gastritis: How To Spot The Difference Before It Worsens?
Credits: iStock
Most of us have dealt with an occasional upset stomach. It’s uncomfortable, but usually passes after a few hours or a quick antacid. But when that stomach pain doesn’t go away or when it keeps returning—it might be something more serious. Two common culprits are gastritis and peptic ulcers. While their symptoms often overlap, these conditions are not identical, and mistaking one for the other can delay treatment and allow complications to develop.
Knowing how ulcers and gastritis are different, what they are caused by, and when to see a doctor is important. If left untreated, both can result in long-term health effects, from ongoing digestive discomfort to bleeding internally and even gastric cancer.
The stomach is designed to deal with acid. The lining of the stomach contains cells that secrete protective mucus and bicarbonate, forming a buffer against the very chemicals that digest food- hydrochloric acid and digestive enzymes.
This defensive system is robust, but not unbreakable. When the mucus layer weakens, or acid production turns too vigorous, stomach lining gets irritated or injured. This interference paves the way for gastritis (stomach lining inflammation) or peptic ulcers (sores in the stomach or small intestine).
Gastritis vs Ulcers: What's The Core Difference?
According to Dr. Amit G. Yelsangikar, gastroenterologist from Apollo Spectra Hospital, Bangalore, "Gastritis is inflammation of the mucous lining of the stomach. It can be caused by infection, chemicals, or irritants that stimulate the digestive system. Ulcers are more profound damage—open wounds that form when acid from the stomach wears away the protective coating. Not like gastritis, ulcers can go through layers of tissue and lead to sharp, focused pain. Gastritis is irritation, whereas ulcers are wounds."
Gastritis vs Ulcers: Overlapping and Deceptive Symptoms
One reason that ulcers and gastritis get confused is that their symptoms appear almost identical. The common symptoms are:
- Burning pain in the upper abdomen
- Bloating and over-burping
- Loss of appetite
- Nausea or vomiting
- Burning sensation in the chest area similar to heartburn
But not everyone with gastritis has symptoms, whereas pain from an ulcer is usually more sharp, burning or gnawing. Ulcer symptoms might get better temporarily after eating, only to recur a few hours later.
An ominous red flag for ulcers is vomiting blood, black stools, or sudden dizziness, which indicate bleeding inside and must be addressed immediately.
What Are The Underlying Causes?
Gastritis
Gastritis typically occurs as a result of stomach lining irritation and not structural damage. Some of the common causes include bacterial infections like stomach flu, heavy drinking, and long-term use of drugs such as NSAIDs (ibuprofen and aspirin). It may also occur due to decreased blood circulation to the stomach lining, as well as chronic stress and poor diet, which also stimulate inflammation.
Ulcers
Ulcers occur when the protective lining of the stomach or duodenum collapses, exposing the tissue to damage. The most prevalent cause is Helicobacter pylori (H. pylori) infection, a bacterium that causes long-term inflammation in the digestive system. An additional main cause is overproduction of stomach acid, which can exacerbate irritation and, in extreme cases, be associated with disorders like Zollinger-Ellison syndrome. Lifestyle and drug use also come into play—prolonged NSAID use and smoking both disrupt the healing process and predispose to recurrent ulcers.
Dr. Yelsangikar comments, "The germ H. pylori is a big contributor. It irritates the stomach and small intestine, thinning the mucous layer and leading to ulcers."
What Are The Risks of Ignoring Symptoms?
What starts as minor stomach upset can become worse. Chronic gastritis can lead to ulcers, and ulcers that aren't treated can result in:
- Internal bleeding, causing anemia or shock
- Perforation, in which the ulcer perforates the stomach wall
- Obstructions, disrupting digestion
- Greater risk of stomach cancer, especially in chronic H. pylori infections
- These complications highlight why proper diagnosis is so important.
Gastritis vs Ulcers: How Physicians Distinguish Them?
Physicians use a combination of patient history, physical exam, and tests to differentiate between ulcers and gastritis. Endoscopy permits direct visualization of the lining of the stomach and identification of ulcers. H. pylori tests (biopsy, stool, or breath) identify bacterial infection. Imaging scans are employed when complications are suspected.
The initial red flag distinguishing ulcers from gastritis is the presence of bleeding—vomit or stool containing blood. Once diagnosed, treatment varies with the cause.
How Does Treatment Addressing The Source In Stomach?
For Ulcers
Initial aim is healing the sore and avoiding recurrence. Routine treatment includes:
- Antibiotics for H. pylori infection
- Proton pump inhibitors (PPIs) to lower stomach acid
- Stopping NSAIDs where feasible
- Surgery, in exceptional cases, for persistent ulcers that do not respond to medication or lead to scarring and nerve damage
For Gastritis
Treatment usually centers around lifestyle modification and symptom control:
- Taking small, frequent meals
- Avoiding spicy, acidic, and carbonated foods
- Reducing smoking and alcohol consumption
- Including bland, stomach-soothing foods such as rice, bananas, and boiled potatoes
- Taking acid-reducing medications with medical guidance
Both conditions improve with stress management, good sleep, and regular medical follow-up, since acid imbalance and inflammation are likely to recur without proper care.
Why Lifestyle Is As Essential As Much As Medicated Treatment?
In most instances, long-term gastric well-being rests as much on lifestyle as on medication. Smoking, alcohol, unhealthy eating, and high-stress lifestyles all compromise the stomach's defenses. Minimizing these risk factors can prevent flare-ups as well as hasten recovery.
Self-medication with over-the-counter antacids to the point of ignoring chronic pain, however, is not an acceptable plan of action. Persistent symptoms require medical examination.
The stomach can appear to be able to stand any amount of abuse, yet gastritis and ulcers disprove this. Both diseases develop quietly, with symptoms that are dismissed or attributed to common indigestion.
The issue is that once they have developed further, the effects become much more serious and even irreversible. If you experience persistent stomach discomfort, unexplained bloating, or appetite changes, it's worth getting an appointment with a gastroenterologist. Tests nowadays are brief, noninvasive, and can avoid years of ongoing digestive issues.
Gastritis and ulcers can have similar symptoms, but they are different diseases that need to be addressed differently. Gastritis is like the warning signal—inflammation indicating that the defenses of the stomach are breached. Ulcers are the full-blown invasion, a wound that needs to be urgently healed.
Both can be treated easily with early diagnosis, specific treatment, and dietary modification. But neglecting the symptoms means allowing an easy-to-handle condition to escalate into a serious one.
That is to say, don't wait for your bellyache to intensify. Recognizing the difference between ulcers and gastritis at an early stage may be the move that saves your well-being.
Dr. Amit G Yelsangikar, MBBS, MD (General Medicine), DNB (Gastroenterology) at Apollo Spectra Hospital, Bangalore in India
Ohio Man Walks Again After Stroke, Thanks To New Implant Technology
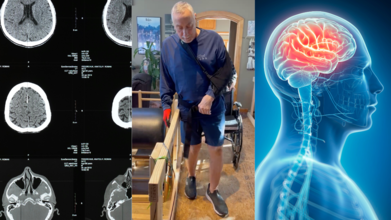
Credits: Canva and Thomas Fello
When Ohio restaurateur Tommy Fello left his restaurant on Christmas Eve, 2023, he thought his truck had a flat tire as it drifted off the road. Exhausted from preparing a holiday buffet since early morning, the then 71-year-old slowly drove home, leaning on his vehicle’s autocorrect system.
But the real problem wasn’t the truck, it was him.
As soon as Fello stepped out of his vehicle, he couldn’t steady himself. Minutes later, he collapsed, unable to move his left arm and leg. Doctors confirmed he had suffered a stroke.
Life After Stroke: Small Victories, Big Struggles
A clot-busting drug saved Fello’s life, but the damage lingered. He lost sensation on the left side of his body, struggled to swallow, and endured intense pain from his curled, immobile arm.
Physical and occupational therapy brought minor improvements, but progress was painfully slow. “Even lifting a cup felt like a gigantic accomplishment,” Fello recalled. “But I kept asking myself—is this as good as it’s going to get?”
The Promise of New Technology
In early 2024, Fello learned of a pioneering device called the Vivistim System, an FDA-approved implant developed by MicroTransponder Inc. The device pairs vagus nerve stimulation (VNS) with rehabilitation exercises to boost recovery in stroke patients with long-standing deficits.
Here’s how it works: during therapy sessions, wireless signals activate the implant, sending gentle pulses to the vagus nerve. These pulses enhance the brain’s ability to “rewire” itself, a process known as neuroplasticity. Patients also continue daily exercises at home.
According to neurosurgeon Dr. Erez Nossek of NYU Langone, who spoke to CBS News, the stimulation allows stroke survivors to achieve “greater and faster improvements in motor function.” A major trial published in The Lancet in 2021 showed patients using Vivistim had two to three times more improvement in arm and hand function compared with standard rehab.
First Patient at Cleveland Clinic
By April 2025, after consulting with Dr. Mark Bain, a cerebrovascular neurosurgeon at Cleveland Clinic, Fello became the hospital’s first patient to receive the implant.
The one-hour surgery placed the key-fob sized device under his clavicle, with tiny leads connected to the vagus nerve in his neck. Bain noted the procedure carries less than a 1% risk of complications. Two weeks later, the device was activated, and Fello resumed therapy with occupational therapist Dr. Sharon Covey.
Remarkable Progress
Within four months, Fello reported dramatic improvement. The constant pain and stiffness in his arm vanished, and he began practicing daily tasks, like carrying objects with his left hand, that were once impossible.
Covey described his progress as “huge,” noting that even the ability to use his left arm for basic tasks is “something he could not have done before.”
Fello, now 72, couldn’t be more optimistic. “I’m very happy I did it. I’m proud, and I can see the progress every day.”
A New Era in Stroke Recovery
Each year, about 800,000 Americans suffer an ischemic stroke, according to experts. While traditional rehabilitation remains essential, many patients plateau, leaving them with lifelong disabilities.
Vivistim represents a new frontier. “This is the first real breakthrough in stroke rehab in decades,” said Covey. “It’s going to turn the stroke recovery world upside down.”
Dr. Bain agrees: “In the next five to ten years, we’ll see an explosion of new technologies that help stroke patients reclaim their lives. With innovations like this—the sky’s the limit.”
For Fello, that future has already begun.
Your Eyes May Reveal Memory Trouble Before Doctors Notice It

Credits: iStock
Our eyes not just windows to the soul perhaps they are mirrors of our cognitive health as well. Recent research suggests that subtle changes in how we scan our visual environment might be a sign of memory loss, providing a painless window into mental health far beyond the classic testing methods.
As we get older, the patterns through which our eyes move—how they scan, lock, and dart between visual fields—evolve slowly. These changes are not only driven by age but also by neurological disease. Researchers from Canada and the West Indies have now found evidence that these patterns of eye movement are closely associated with memory performance, suggesting that our sight could indicate the beginnings of cognitive decay.
The researchers conducted eye-tracking experiments on groups of young and older adults, including participants diagnosed with memory-affecting conditions. By analyzing how their eyes explored images, both on first viewing and upon repetition, the team was able to identify distinct differences in visual behavior.
The results were dramatic. The subjects with compromised memory performance tracked highly consistent gaze patterns from one image to the next, scanning the same areas over and over instead of examining the full field of view. This decreased variability and diminished exploration—lower dispersion of eye movements was contrasted with the more flexible and individualized scanning observed in subjects with better memory.
"Reduced eye movement diversity seems to mirror the cognitive limitations beneath," the scientists write in their research published in PNAS. "Without even having to perform tasks consciously, patterns of gaze differed systematically by group, making them a potential early indicator of memory decline."
How Do Your Eyes Reflect Your Brain Activity?
While the research did not explore in depth the mechanisms underlying these results, previous studies have indicated a close relationship between eye movement and the hippocampus, the area of the brain that is involved in creating and retrieving memory. Alterations in this important region may not only have a deleterious effect on recall but also modify visual attention directed by the brain.
Previous research has shown that eye properties—such as saccadic movement and pupil dilation—have been correlated with cognitive health and even used to predict the development of diseases like Alzheimer's disease. What this study does differently is that it looks at naturalistic gaze behavior, which records people looking at real-world complex stimuli in their natural settings, compared to simple laboratory tasks.
Can Your Eye Movement Be Used As A New Tool for Early Detection?
These findings have important implications. If confirmed in larger, longitudinal studies, eye-tracking measures could offer a quick, cheap, and non-invasive tool to identify early cognitive decline. In contrast to MRI scans or time-consuming neuropsychological testing, this method may be feasible during routine clinical visits or even with digital tools at home.
Scientists propose that eye-tracking might be added to other preclinical diagnostic measures, allowing clinicians to spot vulnerable individuals before difficulties with memory become evident in everyday life. Early diagnosis is important because treatments—pharmacological, lifestyle-oriented, or cognitive—work best when initiated prior to extensive neural damage.
Continuum of Brain Health
One of the main findings of the research is that eye movement change runs on a continuum and indicates gradual decline in brain function and not sudden onset of disease. Even among non-demented, non-cognitively impaired individuals, subtle diminution in exploratory patterns of gaze can presage early or preclinical brain changes.
"This work shows the promise of naturalistic gaze patterns as a sensitive marker for cognitive decline," the researchers write. "Monitoring these patterns longitudinally would make it possible to assess memory health throughout life."
While exciting, the actual clinical utility of this research is still in the distance. Additional studies are necessary to standardize eye-tracking protocols, to estimate the predictive accuracy of gaze metrics, and to define thresholds distinguishing normal aging from incipient cognitive impairment.
Advances in wearable eye-tracking devices, smartphone cameras, and artificial intelligence-powered analysis may speed the translation of these results into daily health monitoring. Think about how cool it would be to have a future where small changes in how you look at a screen or at your environment could warn you or your physician of the first signs of memory loss—months or even years before forgetfulness invades daily life.
Our eyes do more than lead us through the physical world they reflect the state of our mind. As this study shows, the patterns of our gaze hold secret signs of cognitive health and memory function. By tapping these insights, researchers are opening a new frontier for early detection and monitoring of memory loss, holding out hope for proactive treatments and improved brain health outcomes around the world.
Rock Legend Justin Currie Says Parkinson's Makes Playing Guitar Difficult - How Motor Skills Are Affected

(Credit-Spotify)
Del Amitri’s singer, rock legend Justin Currie, recently opened up about his struggle with playing the guitar due to one of the devastating effects of Parkinson's.
The 60-year-old Scottish songwriter spoke about his condition on BBC Breakfast, he explained how the degenerative condition is causing him to lose control of his hand which is affecting his ability to play the bass.
“You get good weeks and bad weeks, I think. And I’ve felt quite asymptomatic recently, slight tremor this morning.” explained Currie. He added how when he has no symptoms it is like being “high” but the weeks when there are recurring symptoms, he feels incredibly ill. When it comes to his career, he added that it's been getting hard navigate, “It’s hard knowing what kind of nick you’re going to be in from gig to gig.”
This is not new news to him, he had known about his diagnosis long before. However, he did not want to go public with this knowledge as he didn’t want to tell his mother, who later passed away.
How Does Parkinson’s Affects Movement?
According to Parkinson’s Community Los Angeles, Parkinson's disease (PD) is a brain disorder that affects a person's ability to move normally. While it might seem strange, one of the best ways to manage the symptoms is to stay active. Participating in games and activities that help with hand-eye coordination, thinking skills, flexibility, and balance is very important for reducing symptoms and improving a person's quality of life.
Parkinson's UK explains that this disease affects a person's ability to move and keep their balance. It's important to remember that everyone experiences symptoms differently, and most people will only have some of them. The disease damages the brain cells that produce dopamine, a chemical needed for smooth, coordinated movement. This damage leads to several common symptoms, including:
Shaking, especially at rest.
Stiff muscles.
Slowness of movement.
Problems with balance.
A sudden, brief inability to move, as if your feet are stuck to the floor.
Painful muscle contractions or cramps.
Movement skills are divided into two main categories: fine motor skills and gross motor skills. Both are affected by Parkinson's, and understanding the difference is key to managing the disease.
Fine Motor Skills vs. Gross Motor Skills
Fine Motor Skills
These are the small, precise movements we use every day, like writing, buttoning a shirt, or picking up small objects. These skills are often one of the first things affected by PD. People may find their handwriting becomes very small and cramped (a condition called micrographia), and simple tasks like using a fork or tying shoelaces become slow and frustrating.
Gross Motor Skills
These involve the use of large muscle groups for bigger movements, such as walking, standing up, or keeping your balance. As PD gets worse, people often struggle with these larger movements. This can lead to a shuffling way of walking, poor balance, and a higher risk of falling. The stiffness and slowness caused by the disease make these movements difficult and slow.
Activities That Can Help With The Loss of Movement
Engaging in specific games and activities can help people with Parkinson's disease improve the small, precise movements of their hands.
Puzzles and Board Games
Puzzles and board games that use small pieces can improve hand movements and dexterity. Puzzles also stimulate your brain, which helps to improve memory and thinking skills.
Coloring and Painting
Holding a pen, pencil, or brush can help you practice control and reduce tremors. It is also a great way to express yourself and feel a sense of calm.
Beading or Knitting
These hobbies require careful, precise movements. You can use larger beads or needles to make the task easier, while still practicing control over movement and timing.
© 2024 Bennett, Coleman & Company Limited

