- Health Conditions A-Z
- Health & Wellness
- Nutrition
- Fitness
- Health News
- Ayurveda
- Videos
- Medicine A-Z
- Parenting
- Web Stories
Watching Too Much Porn Can Have Negative Impact On Your Life
Are you watching too much porn? Psychologists have developed a test to measure whether someone is watching too much porn. The scale was developed after there was significant evidence that watching too much can harm health. This scale helps therapists diagnose problematic pornography use (PPU). This is a type of compulsive sexual behaviour disorder (CSBD), which can affect a person's mental and sexual relationships and may lead to sexual violence.
As reported in the DailyMail, PPU is on the rise, and experts fear that it may lead to conditions like erectile dysfunction, anxiety, and depression, alongside withdrawal symptoms. This is why the experts have come up with a scale to detect PPU.
We spoke to relationship counsellor Ruchi Ruuh, and asked her what could happen if someone watches too much porn and how it affects their sex life? "Frequent exposure to porn can heavily shape sexual scripts, creating distorted ideas about what sex should look like, who should initiate it and what is considered desirable or acceptable. What the whole experience does is that it creates unrealistic physical expectations," she explains.
Ruuh points out that the bodies and genitals depicted in porn form an idealised image which leads to dissatisfaction with their own bodies and their partner's natural appearances.
What Is Porn?
Ruuh explains that it is a performance practised by professionals under guidance. It showcases sex as a flawlessly coordinated and intense, act. It is devoid of pressure, emotions and pauses that are very much a part of a real sexual encounter. This is what creates stress when one tries to replicate such acts in real life.
Another problematic aspect is the glorification of kinks. Most Porn has some kind of kink, performed flawlessly with partners completely in sync and enjoying it. "Porn often highlights extreme or niche kinks as commonplace. While this may normalise exploration, it can also lead to people feeling pressured to engage in acts they’re not ready for or genuinely uncomfortable with," she notes.
Real-life communication, consent and vulnerability are often missing in porn, leading viewers to expect sex to be spontaneous and instinctive.
Porn Leads To Unrealistic Expectations In A Relationship
Due to the unrealistic depiction of genitals, like hairless, symmetrical or surgically enhanced body parts, it can lead to criticism of a partner's body. Many also believe that sex should mirror pornographic perfection. It also misunderstands certain that not all acts can bring pleasure to your partner and that there are certain acts where your partner can draw boundaries.
Affecting The Young Minds
DailyMail reports that the UK has the second highest incidence of internet porn searches in the world, with an average of 1,66,00,000 searches each month. A quarter of 16 to 21-year-olds first saw porn on the internet and were still in primary school. By the age of 13, 50% of them have already been exposed to it. As per a 2015 report published in the Open Journal of Psychiatry & Allied Sciences, in India, 63% of youths in urban areas reported watching porn, with 74% accessing it through their mobile phones. The online erotic comic is also accessed in India.
Ruuh points out that young viewers may think that kinks are common and desired by everyone when it is not actually the case. "They might force, coerce, even shame their partners for being vanilla. Believing that extreme acts, such as BDSM or group sex, are the default rather than exceptions or consensual choices between partners."
There is also an overemphasis on aesthetics, on how the partners look or behave, which may be dissatisfactory in real circumstances. It also creates a perception that sex must escalate or surprise, rather than valuing it as an emotional connection and trust.
"Porn has no real representation of how a relationship dynamic works and how the emotional safety and intimacy ultimately lead to sexual desire. This missing gap makes individuals value the desire for novelty over intimacy which can be detrimental to forming a healthy relationship," says Ruuh.
It also creates anxiety in the bedroom. For instance, your partner may experience performance anxiety for not being "adventurous enough", or body image issues, kink pressure and fear of judgment, which might come from the expectation to perform unrealistic acts.
"Porn often creates a gap between what's fantasy vs the reality. It involves exaggerated scenarios that might seem appealing during solo play for imagination but feel impractical, uncomfortable or even undesirable in real-life settings. This over-reliance on porn’s extreme visuals or specific kinks can create arousal triggers that might not translate into partnered sex, causing frustration or a sense of disconnection. For example, someone might fantasize about certain acts during solo sex, influenced by porn, but find their partner uncomfortable with them. Sex is doing things, two people understanding and pleasing each other accordingly. With Porn, only a one-sided understanding of sex is created, which might make it hard to prioritize shared enjoyment and mutual consent during intimacy," explains Ruuh.
Can It Also Impair People's Communication?
Ruuh says that it could make people feel embarrassed about expressing desires influenced by porn, worrying their partner will find them strange or abnormal. Sometimes, the person also expects their partner to know their kinks, just like what porn shows. Most porn does not show any backstory of how two people or more came to a conclusion on what acts must they perform, this could lead to an unrealistic expectation that your "partner already knows what you want".
"Since porn rarely depicts discussions about emotions, boundaries or consent, viewers may lack the tools and vocabulary to articulate their own needs or respect a partner’s," she says.
So What Does The Porn-Test Scale Do?
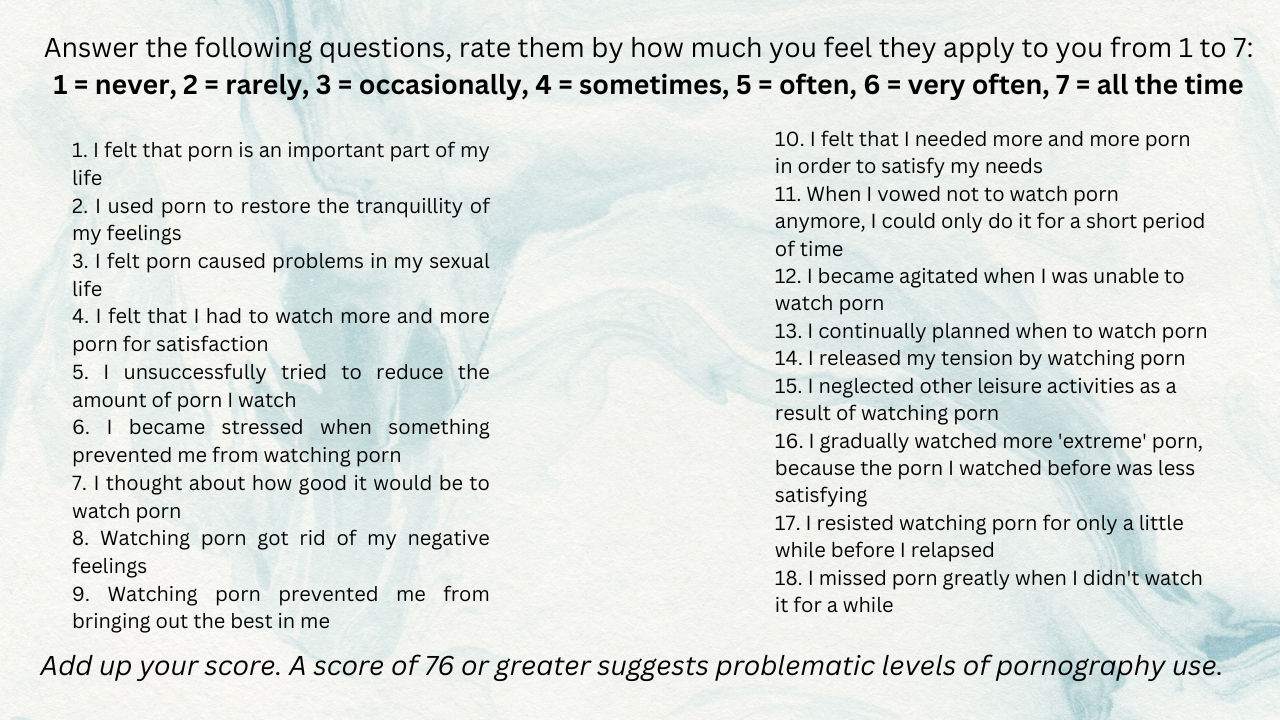
Developed by academics from Nottingham Trent University, the Problematic Pornography Consumption Scale has questioned hundreds of porn users, of both sexes and led to an 18-point questionnaire which can be carried out at home too.
The test found that men are more likely to score highly in this than women, regardless of their sexual orientation.
The test is developed around the 6 core elements of PPU. These include: salience, which refers to how important pornography is to a person's life; mood modification: how much they use masturbation to porn as a way of making them feel a certain way. Conflict: how much does masturbation to porn impact on the significant others, if it gets in the way of their work or other commitments. Tolerance: is masturbation to porn a necessary requirement to achieve a certain mood; relapse, which refers to attempts to abstain and then return to the problematic behaviour patterns; and lastly withdrawal: unpleasant feelings and emotional states that occur after quitting or attempting to quit porn.
What Really Happens In Your Brain During Deep Sleep

Credits: CANVA
Sleep takes up nearly one-third of a person’s life, yet many still wonder what really happens while we rest. Until the mid-20th century, scientists believed sleep was simply a time when the body and brain shut down.
Research now shows that sleep is far from passive, it’s an active, restorative process essential for mental and physical health. As Johns Hopkins neurologist and sleep expert Dr. Mark Wu explains, the brain remains deeply engaged during sleep, performing vital tasks that influence memory, mood, and overall well-being.
The Stages of Sleep
Experts say the human sleep cycle has four main stages that repeat throughout the night. The first three make up non-rapid eye movement (non-REM) sleep, while the fourth is REM sleep, the stage most closely linked with dreaming.
In the first stage of non-REM sleep, the brain and body begin to shift from wakefulness to rest. Brain activity slows, muscles relax, and it is common to experience small, sudden twitches.
During the second stage, the body’s temperature drops slightly, and breathing and heart rate slow. Brainwaves continue to decelerate, though quick bursts of activity may still appear as the brain processes and stores information.
The third stage marks deep sleep, which is the most restorative phase. Here, the body fully relaxes, and the heart rate, breathing, and brain activity reach their lowest levels. This stage is crucial for waking up feeling refreshed and for healing and repair processes throughout the body.
The final stage is REM sleep, which begins about 90 minutes after you fall asleep. It starts short, roughly 10 minutes, but lasts longer with each cycle. During REM, the eyes move rapidly beneath the eyelids, breathing quickens, and heart rate and blood pressure rise to near waking levels. This is when most dreaming occurs. Interestingly, as people age, the amount of REM sleep they experience gradually decreases.
How The Body Regulates Sleep
According to Dr. Wu, two main forces govern sleep: the circadian rhythm and the body’s sleep drive.
The circadian rhythm acts as the body’s internal clock, controlled by a cluster of brain cells that respond to light and darkness. This rhythm triggers the release of melatonin at night and halts it when morning light appears. People who are completely blind often struggle with sleep because their brains can’t register these light cues properly, as per the John Hopkins Study.
The sleep drive works much like hunger. The longer you stay awake, the stronger your urge to sleep becomes. Unlike hunger, though, your body can override your willpower, if exhaustion sets in, it can force sleep to happen, even during daily activities or while driving. In extreme fatigue, brief “microsleep” moments lasting just a few seconds can occur without a person realizing it. However, taking long naps later in the day can reduce this natural sleep pressure, making it harder to fall asleep at night.
Why Sleep Matters For Your Brain
Anyone who has felt mentally sluggish after a sleepless night knows how strongly rest affects the brain. Adequate sleep is key to brain plasticity—the ability to learn, adapt, and form memories. Without it, the brain struggles to retain new information and perform cognitive tasks. Scientists also believe that deep sleep allows the brain to clear out toxins that build up during waking hours, improving long-term brain health.
Sleep impacts far more than the mind. Poor sleep can worsen conditions like depression, high blood pressure, migraines, and even seizures. It weakens the immune system, leaving the body more vulnerable to infection. Metabolism also suffers, as just one night without enough rest can temporarily throw the body into a prediabetic state.
As Dr. Wu explains, “There are countless ways sleep supports health.” From mental clarity to physical repair, the hours we spend asleep are some of the most important for keeping the body and brain functioning at their best.
Can A Rash Be A Sign Of COVID-19? Here’s Everything You Should Know

Credits: canva
When COVID-19 first emerged, it was largely seen as a respiratory illness. Over time, doctors discovered that the virus can affect nearly every major organ, including the heart, kidneys, liver, and skin. While cough, fever, and fatigue remain common signs, some people also develop unusual skin reactions. So, can COVID-19 actually lead to rashes? Here’s what experts have found.
Can COVID-19 Really Cause Rashes?
When COVID-19 first emerged, it was largely seen as a respiratory illness. Over time, doctors discovered that the virus can affect nearly every major organ, including the heart, kidneys, liver, and skin. While cough, fever, and fatigue remain common signs, some people also develop unusual skin reactions. So, can COVID-19 actually lead to rashes? Here’s what experts have found.
What Do COVID-19 Rashes Look Like?
Skin changes linked to COVID-19 are not among the most common symptoms, but they do occur. These rashes may appear on the neck, mouth, or toes and are often caused by inflammation in the body, as per Health website. They can look like flat or raised patches, small round spots, or itchy bumps. In some people, these rashes appear while they’re infected; in others, they show up weeks later.
Why Do These Rashes Occur?
Researchers believe COVID-related rashes are connected to how the virus interacts with the body’s ACE2 receptors, which are found in the skin. When the virus attaches to these receptors, it can trigger the release of inflammatory proteins called cytokines. This inflammation may lead to skin irritation, itchiness, or lesions.
Common Types of COVID-19 Rashes
1. COVID Toes
One of the most recognized skin signs of the virus, “COVID toes,” resembles chilblains, which are cold-weather sores. They appear as pink, red, or purple patches, sometimes with swelling or blistering. This condition is seen more often in younger people and may occur even after other symptoms fade.
2. Hives (Urticaria)
Hives tend to appear suddenly and can spread across any part of the body. They’re itchy, raised, and may come and go within hours or days.
3. Neck Eczema
Some people develop eczema-like rashes on the neck, chest, or trunk during or after COVID-19. The patches can be itchy and vary in color depending on skin tone—pink on lighter skin and brown, gray, or purple on darker skin.
4. Oral Rash
COVID can also cause soreness or peeling inside the mouth or on the lips. The area may feel dry, irritated, or scaly as it heals.
5. Vesicular and Papular Rash
These small, itchy bumps can be filled with fluid (vesicular) or solid (papular). They may appear anywhere on the body and are often linked with ongoing inflammation.
6. Pityriasis Rosea
This condition begins with a single large patch on the chest, back, or abdomen, followed by smaller spots that form a tree-like pattern. Though harmless, it can take several weeks or months to fade.
7. Purpuric or Vasculitic Rash
These rashes appear as dark, bruise-like spots caused by small blood vessel damage under the skin. The color may range from red and purple to brown or black, depending on skin tone.
How Long Do COVID Rashes Last?
The duration depends on the type of rash and the person’s immune response. Most clear up within 2 to 12 days, but some, especially in long COVID cases, may persist for weeks.
How Are COVID Rashes Treated?
Many rashes resolve without any special treatment. To relieve itching or pain, applying mild hydrocortisone cream can help. For more severe or persistent cases, doctors may recommend:
- Antihistamines to reduce itching
- Corticosteroids to lower inflammation
- Blood thinners if the rash is linked to blood vessel irritation
Your doctor will determine the safest treatment depending on the type of rash and overall health.
Disclaimer: This article is for general informational purposes only and should not be considered medical advice. Always consult a qualified healthcare professional before starting, stopping, or changing any medication, or if you experience any unusual symptoms or side effects.
Don't Ignore Your 'Winter Blues', This Is The Biological Reason Behind Winter Depression

(Credit-Canva)
It is a common theme for people to feel down and sad in winter. However, why do shorter, colder days often bring on feelings of loneliness and gloom? There is a biological reason behind it. As the days get shorter, many people feel a dip in energy or mood, but for millions, this signals Seasonal Affective Disorder (SAD), which is a serious form of depression that shouldn't be ignored. Experts from West Virginia University (WVU) caution that SAD symptoms are very similar to major depressive disorder and must be taken seriously.
What Causes SAD?
SAD is much more than just feeling down when it gets dark. It's a genuine type of depression most often seen during the winter months, especially in places far north where daylight is scarce. The basic problem is simple: less natural light hits your eyes. This drop in sunlight confuses your brain's chemistry.
It messes with two vital brain chemicals: serotonin, which helps stabilize your mood, and melatonin, which controls when you sleep and wake up. This lack of light also throws off your body's internal clock, called the circadian rhythm. When all these elements get disrupted, it triggers feelings of low energy and depression.
What Are The Symptoms Of SAD?
SAD involves a cluster of symptoms that persist and significantly interfere with your daily life. The pattern is usually predictable: symptoms begin in the fall, peak in the winter, and disappear by spring. Symptoms often include:
- Feelings of hopelessness.
- Loss of interest in activities you once enjoyed.
- Significant changes in sleep (often sleeping more, or having disrupted sleep).
- Changes in appetite or increased food cravings.
- Difficulty concentrating and persistent fatigue.
The risk of SAD is higher among younger people, women, and those with a family history of mood disorders.
Can You Treat/Prevent Seasonal Affective Disorder?
Because Seasonal Affective Disorder is highly predictable, experts advise starting preventative treatments early in the fall. Seeing a healthcare provider is essential to determine the best plan and timing for treatment, rather than waiting for severe symptoms to appear later in winter.
Light Therapy
This involves sitting daily before a special light box emitting 10,000 lux of bright white light. Doing this for 30 to 60 minutes each morning is the most common and effective treatment for SAD, as it helps correct the imbalance caused by reduced sunlight exposure.
Cognitive-Behavioral Therapy (CBT)
This form of talk therapy teaches you practical skills to manage negative thinking patterns and behaviors linked to depression. CBT helps individuals reframe their outlook on winter and build effective coping mechanisms to reduce the impact of SAD symptoms.
Medication
In certain situations, a healthcare provider may prescribe antidepressant medication to help regulate mood-affecting brain chemicals like serotonin. This is often considered alongside light therapy or counseling, especially if symptoms of depression are severe or persistent.
Lifestyle Changes
Simple daily habits are powerful tools. Regular exercise boosts mood and energy, while maintaining a consistent sleep schedule keeps your body's internal clock stable. These practical steps offer significant support alongside clinical treatments.
© 2024 Bennett, Coleman & Company Limited

