- Health Conditions A-Z
- Health & Wellness
- Nutrition
- Fitness
- Health News
- Ayurveda
- Videos
- Medicine A-Z
- Parenting
What Are Cluster Headaches? Symptoms And How To Prevent

Cluster Headache (Credit-Canva)
Cluster headaches are a type of severe headache that typically occurs on one side of the head, often around the eye. The pain can be so intense that it may feel like a hot poker in the eye or a sharp nail behind the eye.
The primary symptom is excruciating pain on one side of the head. You may also experience a runny nose, watery eyes, stuffy nose, sweating, and restlessness. The exact cause of cluster headaches is unknown, but genetics may play a role.
Doctors may prescribe medications to help prevent or treat cluster headaches. Simple lifestyle modifications can also help reduce the frequency and severity of attacks. These include stress management techniques like meditation or yoga, identifying and avoiding triggers, getting regular sleep, and maintaining a healthy diet.
Symptoms Of Cluster Headaches
Cluster headaches are characterized by severe, stabbing pain that typically occurs on one side of the head, often around the eye. The pain can be so intense that it may cause people to pace or rock back and forth. In addition to the intense pain, other symptoms may include watering eye, nasal congestion, swollen eyelid, dilated pupil, restlessness, sweating, and sensitivity to light.
Causes of Cluster Headache
Cluster headaches are believed to be caused by changes in brain chemistry, specifically the overactivity of certain nerves that control pain and blood flow to the head. While the exact cause remains unknown, several factors may contribute to their development:
Genetic Predisposition: Individuals with a family history of cluster headaches are more likely to develop the condition themselves, suggesting a genetic component.
Environmental Triggers: Certain environmental factors can trigger or worsen cluster headaches, such as alcohol consumption, exposure to strong odors, bright light, mental stress, and altitude changes.
Hormonal Influences: Hormonal fluctuations, particularly in women, may contribute to the development or worsening of cluster headaches. Estrogen, a female sex hormone, has been linked to the condition, and some women may notice a reduction in headache frequency or severity during pregnancy or while on estrogen medication.
Home Remedies for Cluster Headaches
Cluster headaches can be extremely painful, but there are some home remedies that may provide temporary relief. Applying an ice pack or a warm compress to the affected side of your head can help soothe pain and inflammation. Gently massaging your temples or the back of your neck can relax muscles and alleviate pain. Acupressure, which involves applying pressure to specific points on your body, may also provide relief for some people. Additionally, relaxation techniques like meditation, deep breathing, or yoga can help reduce stress, which is a known trigger for cluster headaches.
Preventing Cluster Headaches
To help prevent cluster headaches, you can take several steps. First, identify and avoid any personal triggers, such as alcohol, strong odors, or bright light. Managing stress is also crucial, as stress can exacerbate cluster headaches. Incorporate relaxation techniques like meditation, deep breathing, or yoga into your daily routine. Regular exercise can help improve overall health and reduce stress, which may also contribute to preventing cluster headaches.
Aim for 7-8 hours of sleep each night to ensure adequate rest and hormonal regulation. Finally, maintaining a healthy diet can support your overall well-being and potentially reduce the risk of headaches. Avoid foods that trigger migraines, such as aged cheeses, cured meats, and chocolate. Additionally, limiting your intake of caffeine and alcohol can help prevent headaches.
How 26,000 Lives Could Be Saved Each Year With Just One Change to Lung Cancer Screening

Credits: Canva
If screening is made available and accessible to those between 40 to 85 years of age, it could detect 94% of lung cancers. Even if 30% of people get screened, it could prevent 26,000 deaths in the US. Despite that, the screening for the deadliest cancer in the US still misses most cases, reveals a JAMA Network study. As per the American Cancer Society, 226,650 new cases of lung and bronchus cancer in 2025, the Centers for Disease Control and Prevention (CDC) notes 18,893 new cases in 2022. As for deaths, the American Cancer Society estimates around 124,730 lung cancer deaths in 2025.
The Washington Post reports that when a 42-year-old mother of three, Jessie Creel first developed a stubborn cough in May last year, she did what most people would do. She went to her doctor, took the prescribed antibiotics and hoped to bounce back quickly. Instead, her cough worsened. She began losing weight, struggled to sleep and even coughed up blood during a camping trip. Nothing about it felt normal anymore.
Six months later, she was diagnosed with Stage 4 lung cancer. Creel ran, swam, avoided alcohol and had never smoked, yet her cancer had spread to her bones, brain and lymph nodes by the time it was detected. Her story is becoming more familiar among cancer specialists, who now say lung cancer is no longer a disease that fits the old stereotype of the heavy smoker. The JAMA Network study is pushing experts to ask whether current lung cancer screening guidelines are excluding thousands of people who might benefit from early detection.
The Current Screening Rules That Limits People From Getting Themselves Screened
Right now, lung cancer screening in the United States is recommended only for people between 50 and 80 who have a heavy smoking history and who either still smoke or quit within the last 15 years. However, the researchers of the new study examined around 1000 lung cancer patients treated at Northwestern Medicine. Only one third would have qualified for screening under today’s guidelines. Women, people of color and those who had never smoked made up a large portion of the patients who fell outside the criteria.
According to the study’s authors, this means most lung cancer cases in the country are detected only after symptoms appear, which often happens when the cancer has already advanced.
Experts suggest a broader, age based approach similar to breast or colon cancer screening. If everyone between 40 and 85 could get screened, researchers estimate that nearly 94 percent of lung cancer cases could be identified, potentially preventing more than 26,000 deaths each year even if only a fraction of eligible people participated.
How Is Lung Cancer Detected?
For those who qualify, lung cancer screening is done using a low dose CT scan once a year. These scans use far less radiation than a regular CT and have been shown to catch cancers early.
The U.S. Preventive Services Task Force guidelines decide who gets insurance covered screening. The American Cancer Society has its own recommendation, which is slightly more flexible but does not guarantee full coverage.
Doctors say that when lung cancer is caught early through screening, cure rates can exceed 90 percent. But many people who do not meet today’s criteria never get that chance and are often diagnosed only once symptoms set in. By that stage, treatment is more complex and outcomes are less optimistic.
Why Are Experts Asking For A Change In System?
Lung cancer remains the leading cause of cancer related deaths. It kills more people than breast, colon and prostate cancers combined. Yet smoking rates have dropped significantly over the years, which means screening based on smoking history alone no longer reflects who is actually getting sick.
The new study suggests that continuing with the current guidelines would mean detecting only one third of new cases. Experts call the findings alarming and believe shifting to an age based model could save more lives than the number of people who die each year from brain cancer.
Broader screening may also reduce long term healthcare costs. Detecting cancer at Stage 1 rather than Stage 4 could save nearly 25 billion dollars annually in treatment expenses, far outweighing the cost of offering more people access to scans.
These Popular Medicines May Trigger Serious Side Effects, Pharmacist Warns

Credits: Canva
We often reach for pills to soothe a headache, ease congestion, or help us drift off to sleep. Yet one experienced pharmacist believes that several everyday medicines tucked inside our bathroom cabinets may be causing more problems than they solve. Deborah Grayson, who has spent 13 years in pharmacy practice, has shared a firm warning about seven widely used treatments she personally avoids. Her concerns range from overpowering drowsiness that leaves people feeling disconnected to medications that can create a dependence over time.
Medicines That May Trigger Serious Side Effects
Below are the seven products she is cautious about, along with the alternatives she suggests.
1. Codeine
Codeine, sometimes sold in low doses mixed with paracetamol, is a strong opioid pain reliever. Deborah believes the danger of becoming reliant on it overshadows the intended relief.
She explained to the Daily Mail that opioid medicines convert to morphine inside the body and act on pain pathways to reduce discomfort, often bringing a warm, pleasant sensation that some describe as a mild “buzz.”
Her preferred approach for mild to moderate pain is sticking to paracetamol or ibuprofen. If those options fall short, she advises speaking with a doctor instead of moving to opioids.
2. Statins
Statins are prescribed to millions to help manage cholesterol levels, though debate continues about how effective they truly are for certain groups. Deborah said they should be used only when necessary, as people without clear risk may gain little benefit.
She noted that women may see even fewer protective effects, which raises concerns about whether many are being offered these drugs without enough consideration. Muscle aches, tiredness and possible liver irritation are recognised risks. She recommends having a detailed discussion with a healthcare professional to review whether another option may be more suitable.
3. Anti-depressants
Prescriptions for antidepressants in the UK have risen sharply. While these medicines are essential for many, Deborah believes that their long-term side effects and withdrawal symptoms can outweigh the positives for others.
She pointed out that access to cognitive behavioural therapy remains limited in an already strained health system, even though therapy may offer more lasting support for some patients. She added that antidepressants can cause nausea, headaches and sleep problems, and with long-term use may raise the risk of weight gain, diabetes and stomach bleeding.
Some people also develop sexual side effects, while withdrawal may bring dizziness, nausea, sharp shock-like sensations in the head, intense anxiety, irritability and disturbed sleep.
4. Gabapentin and Pregabalin
These medicines are often prescribed for nerve pain or fibromyalgia, yet Deborah feels that their side effects are not always fully explained.
She said they can lead to heavy drowsiness, poor balance, difficulty with concentration and memory issues over time, along with weight gain. Many people find the initial effects so overwhelming that they stop before any improvement is noticed, which may take several weeks.
Both medicines are controlled because of the possibility of addiction, and some users may develop both physical and psychological dependence.
5. Steroid Creams
Steroid creams are frequently used to manage eczema, psoriasis and other skin flare-ups. They are helpful in short bursts, although Deborah worries that many people continue using them far longer than advised because routine follow-up is often lacking.
Extended use may thin the skin and trigger painful reactions or infections. This creates a pattern where the discomfort returns, leading patients to reach again for the same cream, keeping them stuck in a cycle.
6. PPIs
Proton pump inhibitors, such as omeprazole or lansoprazole, are among the most common treatments for heartburn and acid reflux.
Deborah views these as a quick solution that can cause long-term harm if people rely on them for too long. She explained that stomach acid is necessary for breaking down food and absorbing nutrients, and PPIs interfere with this process. This can leave the stomach struggling to digest properly and may contribute to nutrient shortages.
She encourages people to consider dietary adjustments and stress management instead of long-term dependence on PPIs.
7. Laxatives
Many people turn to laxatives for constipation, and with so many available without a prescription, it is easy to depend on them more than intended. While they work well for short-term relief, consistent use may cause the bowel to slow down.
Deborah warned that many people eventually struggle to go to the toilet without help from these products. Short-term effects can include cramps, diarrhea, nausea, bloating, and trapped wind.
For ongoing constipation, she suggests increasing fibre intake or using options that draw more water into the bowel, such as Fybogel (ispaghula husk) or Macrogol sachets.
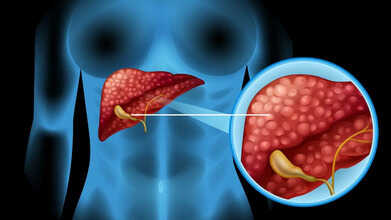
One Blood Type Linked To Higher Rates Of Fatal Liver Illness, Study Finds
Credits: Canva
A recent study suggests that a person’s blood group could play a role in whether they are more likely to develop severe liver conditions. Although most of us link blood type only with transfusions or donor matching, scientists now believe it may also offer clues about long-term liver health.
Higher Liver Disease Risk Linked to This Blood Group
A new study published in the journal Frontiers reports that individuals with blood group A have an increased chance of autoimmune liver disorders. In these conditions, the body’s own immune system mistakenly harms liver tissue, which can lead to ongoing damage and, in some cases, life-threatening liver failure.
The researchers also found that people with blood group B may have a slightly lower likelihood of certain liver-related concerns compared with those who have type A.
Why Your Blood Group Could Influence Liver Health?
Scientists have long examined how inherited blood groups relate to different illnesses. Some earlier findings noted that individuals with non-O blood types (A, B, or AB) tend to show higher activity of certain clotting factors and other changes in the body.
These differences may affect blood flow in the liver. For example, past studies found slightly increased levels of a clotting protein called von Willebrand factor in people with advanced liver disease who had non-O blood types, although it does not appear to be a major driver of risk.
Liver Conditions Connected to Certain Blood Groups
The latest research focused on autoimmune liver diseases such as:
- Autoimmune hepatitis, in which the immune system attacks liver cells.
- Primary biliary cholangitis (PBC), where the bile ducts inside the liver slowly break down.
Among these, autoimmune hepatitis showed a stronger link with blood group A. Blood group B appeared to carry a somewhat lower chance of PBC when compared with type A.
What Past Research Shows About Liver Cancer
Several earlier studies explored the relationship between blood group and liver cancer (hepatocellular carcinoma or HCC). Older data and a large meta-analysis found that people with type O blood were under-represented among those with liver cancer, suggesting that type O may be tied to a lower risk overall.
Why Knowing Your Blood Type Helps
Understanding your blood group can offer insight into potential health risks, though it does not mean you will certainly develop liver disease if you are type A or B. It remains only one part of a larger picture.
This may be especially important if you have blood type A or B and a family history of liver conditions. Routine health checks, liver screenings, and discussions with your doctor can help you watch for any early signs.
For now, it is clear that blood type is more than a simple classification, as it may hold useful information about future liver health.
Autoimmune liver disorders are uncommon, yet they can become serious when they are not spotted in time. A better grasp of the genetic and immune-related factors behind them can guide stronger prevention and treatment efforts. The authors of the study note that more research involving larger and more varied groups of people is needed to confirm these findings and to explain how different ABO blood types may influence the development of autoimmune liver problems.
© 2024 Bennett, Coleman & Company Limited

