- Health Conditions A-Z
- Health & Wellness
- Nutrition
- Fitness
- Health News
- Ayurveda
- Videos
- Medicine A-Z
- Parenting
What To Expect From Menopause?

Menopause could lead to weight gain (Credits: Canva)
There are many phases in a woman's life, menarche, menstruations, pregnancy, postpartum and menopause. Each phase comes with its own challenges, and changes the way of looking at life. However, narrowing to one, today we are focusing on weight gain after menopause. Gaining weight is a common concern for many women are approaching menopause. This period brings hormonal changes, shifts in activity levels and effects of aging. All of these contribute to weight gain. However, not everyone experiences weight gain during menopause, and individual experiences may vary greatly.
Menopause and Its Life Phases
Before diving into the specifics of weight gain, it’s helpful to understand the terminology associated with menopause:
- Premenopause refers to the period between puberty and the commencement of perimenopause.
- Perimenopause is the transitory period before menopause, characterized by fluctuating reproductive hormones.
- Menopause is defined as the absence of menstrual cycles for 12 consecutive months.
- Postmenopause is the period following menopause; typically used interchangeably with "menopause."
Hormonal Changes and Weight Gain
Hormones influence weight fluctuations after menopause, specifically how fat is distributed and how the body controls hunger.
Fat Content and Distribution
The hormonal fluctuations of perimenopause and menopause influence where fat is stored in the body:
Perimenopause: During this phase, estrogen levels fluctuate while progesterone levels decline steadily. In early perimenopause, higher estrogen levels can promote fat storage in the hips and thighs as subcutaneous fat, which generally carries fewer health risks.
Menopause: As estrogen levels drop significantly, fat storage shifts to the abdominal area as visceral fat.
This type of fat surrounds internal organs and is associated with health risks like:
- Insulin resistance
- Type 2 diabetes
- Heart disease
- Other metabolic issues
Appetite Regulation
Lower estrogen levels during perimenopause can have an impact on appetite management. A 2019 analysis found that decreased estrogen may diminish satiety signals, making you feel less full after meals. This might lead to increased calorie consumption and weight gain.
The Effect of Age on Weight
Weight gain during menopause is attributed to more than just hormonal changes. Several elements come into play throughout the aging process:
Increased fat content and decreased muscle mass: These changes affect the body's resting energy expenditure (REE), which means fewer calories are expended when at rest.
Lower activity levels: Fatigue, sleep difficulties, and menopause-related symptoms can all lead to a decrease in physical activity, further reducing REE and increasing weight.
Managing Weight Gain During Menopause
If you are concerned about weight gain during menopause, a variety of strategies can help you manage it effectively. It is usually recommended that you speak with a healthcare practitioner before developing a specific approach.
Dietary modifications
Focus on a well-balanced diet that includes less carbohydrates, more fiber, and less added sugar and salt.
Include nutrient-dense meals to boost overall health.
Physical exercise
Regular exercise helps to maintain muscle mass and reduce body fat. Strength training, aerobic, and flexibility exercises are quite beneficial.
If you have osteoporosis, see your doctor about safe activity options.
Rest and Stress Management
Prioritize sleep and relaxation to combat fatigue and stress, both of which can contribute to weight gain.
Mindfulness practices or yoga may help reduce stress levels.
Breast Cancer Signs That Do Not Feel Like Cancer, Explain Doctors

Credits: iStock
On World Cancer Day 2026, we at Health and Me is focussing on the most common cancer among women in India. Breast Cancer, which accounts for over 216,000 new cases every year, as per the 2022 data. This means, 28.2 per cent of female cancers are attributed to breast cancer. What is more tragic is that one woman is diagnosed with breast cancer every four minutes, and one dies every eight minutes in the country.
While, we all know that finding a lump is the red flag, there are other signs that women often miss that delays their detection. Health experts are increasingly warning that this narrow understanding may be delaying early diagnosis for many patients. New medical insights suggest that several lesser-known changes in breast tissue, skin and nipple appearance may signal cancer but often go unnoticed or get dismissed as harmless hormonal changes.
Read: More Than A Diagnosis: Cancer Survivors Share The Small Wins That Helped Them Heal
Breast Cancer Is Not Just A Lump
Data from a consumer survey commissioned by The Ohio State University Comprehensive Cancer Center shows that 93 percent of adults identify a lump as a symptom of breast cancer. But fewer than half are aware of several other warning signs that could appear much earlier.

Experts warn that this knowledge gap can be risky because not all breast cancers form lumps that are easily felt. Breast medical oncologist Ashley Pariser explains that screening mammography remains the most effective tool for detecting breast cancer at its earliest and most treatable stages. She adds that being familiar with the normal look and feel of one’s breast tissue helps people detect subtle changes faster and seek timely medical care.
Pariser notes that many breast changes can occur due to aging or childbirth. Still, she stresses that breast cancer can present in multiple ways, making it important for individuals to report unusual symptoms without delay.
Signs That Should Not Be Ignored
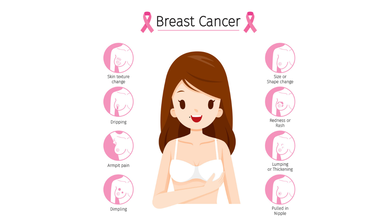
According to Dr Kanchan Kaur, Oncoplastic Breast Surgery Specialist, structural changes in the breast are among the most overlooked early warning signs. She highlights that while lumps are common indicators, deformations in breast shape such as flattening, indentation or dimpling should not be ignored.
Read: AI Detects More Breast Cancer Cases in Landmark Swedish Study
Dr Kaur also points out that an unusual increase or decrease in breast size, particularly when it affects only one breast, and sudden changes in breast symmetry may signal an underlying issue. She advises that these signs warrant clinical evaluation even if they appear painless or gradual.
Another concerning sign is skin texture change. She explains that a reddish, pitted texture resembling the surface of an orange or a marble-like area under the skin can indicate deeper tissue abnormalities. Any area of the breast that looks or feels noticeably different from surrounding tissue should be assessed by a doctor.
Nipple Changes Can Be Early Red Flags
Both research findings and clinical observations highlight nipple changes as key indicators that are often missed. Survey results from Ohio State University show that only about one-third of respondents recognized nipple inversion or retraction as a symptom of breast cancer.
Dr Kaur notes that nipples can provide early clues about breast disease. Symptoms such as newly inverted nipples, dimpling around the nipple, scaly red rashes, burning or itching, and ulceration should prompt medical attention.
Read: Oncologists Warns Of The Cancer Rising Among Women in India
Clear or bloody nipple discharge that is unrelated to pregnancy or breastfeeding is another warning sign. While discharge can occur due to benign causes, experts recommend prompt evaluation to rule out cancer.
Specialists at Moffitt Cancer Center caution that symptoms such as breast tenderness, swelling or changes in fullness are often mistaken for routine hormonal fluctuations. Because these symptoms frequently overlap with premenstrual changes, many women delay consulting a specialist.
Experts from the center advise that persistent breast pain, swelling or unusual fullness that does not resolve within a few days should be medically evaluated. They emphasize that sudden nipple inversion, discharge or skin texture changes require immediate attention.
World Cancer Day 2026: India’s 10 Most Common Cancers, Explains Doctor
Credits: Canva
Cancer trends in India are changing rapidly, driven by lifestyle patterns, environmental exposure, infections, and limited access to early healthcare in some regions. According to Dr Puneet Gupta, Chairman of Oncology Services at Asian Hospital, understanding early warning signs and adopting preventive habits can significantly improve survival outcomes.
“Cancer patterns in India are the results of multiple factors ranging from lifestyle, environmental exposure, infections and access to timely care,” Dr Gupta explained, adding that early symptoms can appear months or even years before the disease reaches advanced stages.
Breast Cancer: The Most Common Cancer In Women
Dr Gupta noted that breast cancer is frequently seen in women, especially after the age of 40. He highlighted that the disease often develops silently and without pain.
He explained that warning signs may include lumps in the breast or under the arm, changes in breast shape, skin dimpling, inward turning of the nipple, or unusual discharge. “Do not ignore these changes,” he cautioned. Regular self-examination, along with timely imaging tests such as mammography, ultrasound, or MRI, can help detect breast cancer early.
Cervical Cancer: Strongly Linked To HPV Infection
Cervical cancer mainly affects women between 30 and 60 years. Dr Gupta emphasised that HPV infection remains the leading risk factor. Early symptoms can include abnormal vaginal bleeding, bleeding after intercourse, or persistent pelvic pain, although early stages often remain symptom-free.
He stressed that routine Pap smear screening and HPV vaccination play a crucial role in prevention and early diagnosis.
Lung Cancer: Rising Risk Beyond Smoking
While lung cancer remains more common in men, Dr Gupta pointed out that cases among women are rising as well. Smoking is the primary cause, but exposure to fine particulate air pollution (PM2.5) also contributes to the risk.
He warned that persistent cough, chest pain, breathing difficulty, unexplained weight loss, or coughing blood require immediate medical evaluation, particularly in people with a history of tobacco use.
Oral Cancer: A Major Concern In India
Oral cancer remains widespread due to tobacco, gutka, areca nut consumption, and HPV infection. Dr Gupta explained that long-lasting mouth ulcers, red or white patches inside the mouth, jaw stiffness, or swallowing difficulty are early red flags. Regular dental and oral examinations can help detect early cancerous changes.
Colorectal Cancer: Lifestyle-Linked Risks
According to Dr Gupta, colorectal cancer is increasingly being diagnosed in adults around 40 years of age. Sedentary lifestyles, low-fiber diets, and excessive red meat intake are major contributing factors.
He said symptoms such as blood in stool, persistent bowel habit changes, abdominal pain, or unexplained anaemia should not be overlooked. Early screening and genetic testing in high-risk individuals can significantly improve outcomes.
Stomach Cancer: Often Shows Subtle Symptoms
Dr Gupta explained that stomach cancer may initially present as indigestion, early fullness, nausea, or unexplained weight loss. It is often associated with long-term Helicobacter pylori infection, smoking, and salt-heavy diets. Persistent digestive discomfort warrants medical attention.
Prostate Cancer: Common But Often Slow Growing
Prostate cancer typically affects men above 50 and usually progresses gradually. Dr Gupta noted that difficulty urinating and frequent nighttime urination are common early symptoms. Regular check-ups help detect the disease before complications arise.
Esophageal Cancer: Linked To Lifestyle And Nutrition
Tobacco use, alcohol consumption, poor nutrition, and iron deficiency increase the risk of esophageal cancer. Dr Gupta advised that swallowing difficulty, chest discomfort, or unexplained weight loss should prompt evaluation through tests like endoscopy or barium swallow.
Ovarian Cancer: Often Missed Due To Vague Symptoms
Dr Gupta explained that ovarian cancer frequently goes undetected due to non-specific symptoms such as bloating, abdominal discomfort, or early satiety. Women with persistent symptoms, particularly those with a family history of breast or ovarian cancer, should seek medical evaluation.
Liver Cancer: Screening Is Crucial For High-Risk Groups
Liver cancer often develops in individuals with chronic liver disease. Symptoms such as jaundice, abdominal swelling, or persistent pain usually appear late. Dr Gupta stressed that hepatitis vaccination and screening among high-risk groups are vital for prevention.
Lifestyle Changes And Screening Can Reduce Risk
Dr Gupta emphasized that although cancer cannot be completely prevented, a significant proportion of cases are linked to modifiable risk factors. Avoiding tobacco, maintaining a healthy weight, consuming balanced nutrition, managing stress, and staying physically active can lower risk.
He added that vaccinations against HPV and hepatitis further reduce cancer risk, while regular screening helps detect cancers at pre-cancer or early stages. “Education, prevention and early detection make the difference between late-stage disease and long-term survival,” Dr Gupta concluded.
Prenatal Vitamins vs Multivitamins: Experts Reveal What Women Need

Credit: Canva
While you may have seen multiple women, who are not pregnant, taking prenatal vitamins to improve their skin, hair and nail quality, experts say you should steer clear and only stick to multivitamins to ensure your body stays healthy all-year round.
Prenatal vitamins are daily supplements for women who are pregnant or trying to get pregnant. These supplements contain the vitamins and minerals you need to support healthy fetal development, according to the Cleveland Clinic.
Dr Rohan Palshetkar, Consultant IVF Specialist, Bloom IVF tells Healthandme: ""Prenatal vitamin should be taken three months at least prior to the pregnancy or basically whenever you begin to start planning the pregnancy, ensure that all your micro nutrients as well as your folic acid levels are up to the normal mark so as to ensure that your baby has a healthy growth"
But when your body doesn't need it, taking supplements could put you at risk over time.
Which Vitamins And Minerals Are Prenatal Vitamins Rich In?
As per the American College of Obstetricians and Gynecologists (ACOG), here are the most important nutrients prenatal vitamins are packed with:
Folic Acid: One of the most important prenatal nutrients, this B vitamin is important as it creates your baby's neural tube. This is the structure that eventually forms brain. As per the US Preventive Services Task Force, folic acid supplements significantly increase the growth of healthy neural tube. The American Academy of Pediatrics also notes that it helps the neural tube to protect from defects by 50 percent.
Iron: It supplies blood and oxygen to the fetus and also helps build the placenta. It also gives the mother extra blood volume that you need throughout pregnancy. Pregnant people are prone to anemia, this is why iron supplementation is a must.
Calcium: The most time spend in uterus for a baby is invested in building their bones and teeth, this is a Herculean task, and requires the mother to have plenty of calcium. If you don't have enough calcium, then your baby will utilise the calcium from your body, which could lead to temporary bone loss.
Certain prenatal supplements also contain other additives such as omega-3 fatty acids.
Why Is It Dangerous To Take Prenatal Vitamins
The main difference between a prenatal vitamin and a multivitamin is the concentration of folic acid and iron.
Ingesting enough folate from food or folic acid from supplements at the start of a pregnancy lowers the risk of certain birth defects. Along with this, iron supplements help the body make the extra blood cells needed during pregnancy.
The amount of folic acid suggested for people who are planning a pregnancy is 400 to 800 micrograms (mcg) a day. The amount of iron needed in pregnancy is 27 milligrams (mg) a day.
The typical amount of folic acid for an non-pregnant adult is 400 mcg a day. For iron, the typical daily amount is 8 mg for males and 18 mg for females.
Taking iron and folic acid at levels higher than the suggested amounts may bump people closer to the upper limit for these nutrients which can raise the risk of health problems.
Taking too much folic acid, especially over 1,000 mcg daily without a doctor's advice, can mask a vitamin B12 deficiency, potentially causing irreversible nerve damage and may lead to side effects such as bitter taste, nausea or sleep problems, with potential links to increased risks in pregnancy like autism or insulin resistance.
Eating too much iron, especially from supplements, can cause acute iron poisoning, leading to severe nausea, vomiting, abdominal pain, diarrhea and bloody stools. Long-term excessive intake causes iron to deposit in tissues, causing iron overload (hemochromatosis) that damages the liver (cirrhosis), heart (failure), and pancreas (diabetes) and may cause a bronze skin color.
© 2024 Bennett, Coleman & Company Limited

