- Health Conditions A-Z
- Health & Wellness
- Nutrition
- Fitness
- Health News
- Ayurveda
- Videos
- Medicine A-Z
- Parenting
- Web Stories
When Your Phone Ping Feels Like a Threat: The Science Behind Cortisol Spikes, Sleep Disruption and Notification Anxiety

If you’ve ever felt your heart rate spike just because your phone buzzed during dinner, you’re not alone. In our hyper-connected lives, notifications can set off a full-blown biological alarm. But what’s happening inside you isn’t just “in your head”; it’s ancient biology meeting modern tech, and the result is often anxiety, chronic stress and, eventually, burnout.
Here’s why you panic every time that screen lights up and how to stop spiralling into stress over a simple message.
Your brain may be rational, but your hormones have other ideas. According to reports, the moment a message lands, especially one that feels urgent or work-related, your body launches into ‘fight or flight’ mode.
Cortisol, the stress hormone, floods your system and primes you to react. And if the ping is from your boss or an emotionally charged source, the cortisol surge can be even more intense.
Also Read: Mouth Ulcers Are Common, But Run To Your Doctor Or Dentist If You Notice These Signs
To make things worse, adrenaline often tags along. This amps up alertness, raises your heart rate and makes it nearly impossible to relax. Your brain is preparing you to flee from danger even if the only threat is an email with the subject line “quick update”.
The Dopamine Trap
Just to complicate things, dopamine, the pleasure chemical, also plays a part. Every time you check your phone and respond, your brain rewards you with a little shot of satisfaction. That’s why it’s so easy to get hooked and why you keep checking even though it stresses you out.When Oxytocin Gets Triggered
Normally, messages from loved ones trigger oxytocin, the hormone that helps us bond and feel safe. But when the messages are draining, demanding or tied to work, that warm fuzzy feeling gets pushed out by stress chemicals. Over time, this can disrupt your ability to be present and genuinely connect with others, leading to burnout.Melatonin Meltdown
And if you’re checking those pings before bed, you should stop. Reports warn that notifications late at night reduce the production of melatonin, the hormone responsible for quality sleep. Without it, you may struggle to nod off, stay asleep or feel rested, fuelling a cycle of fatigue, brain fog and even more stress.The Long-Term Fallout
If this sounds like an exhausting loop, it is. Consistent cortisol spikes and dopamine hits can wreak havoc on your health. Think weight gain, insomnia, poor focus and a fried nervous system. In fact, studies show that 76 per cent of millennials and 40 per cent of baby boomers admit to feeling anxious the moment their phone lights up.Here are a few tricks to help you break the cycle.
1. Set Notification Boundaries
Draw a digital line in the sand. Turn off alerts after a set time or batch-check messages every few hours instead of reacting instantly. Use your phone’s ‘Do Not Disturb’ mode to protect time for real life.
2. Mute the Noise
Not every ping is essential. Reports suggest turning off non-urgent app and group chat notifications. Fewer pings mean fewer cortisol spikes and less temptation to fall down the notification rabbit hole.
3. Prioritise In-Person Conversations
Texts are easy to misread, and fast replies aren’t always the best ones. If possible, have real conversations with friends, colleagues or family. Face-to-face talks promote oxytocin, reduce stress and avoid unnecessary misunderstandings.
4. Train Yourself to Pause
Next time your phone buzzes, don’t jump. Take five deep breaths. Count to five. Ask yourself if the message needs an immediate reply. This tiny pause rewires your stress response and reins in that hormone cascade.
5. Keep Work Messages in Their Lane
When work bleeds into personal time, stress seeps in. It is recommended to have a chat with your manager or team about boundaries. Set a window for work-related conversations and stick to it. Your wellbeing shouldn’t be a casualty of always being “available”.
Ronald Acuña Jr. Sidelined with Achilles Tendon Tightness: What It Means and Why It Matters

It’s déjà vu Braves fans didn’t ask for. Ronald Acuña Jr., Atlanta’s powerhouse baseball outfielder and reigning National League MVP, has hit the injured list again, this time with tightness in his right Achilles tendon. Just months after returning from a torn ACL in his left knee, Acuña pulled up sore after sprinting the bases and later chasing a fly ball, exiting Tuesday’s game against the Royals mid-inning.
But what does Achilles tendon tightness actually mean, and why does it freak out athletes and sports doctors alike?
The Achilles tendon, also known as the calcaneal tendon, is the thick band of tissue that connects your calf muscles to your heel bone. It is the biggest and strongest tendon in the human body. But it can bring even the fittest athletes to their knees.
It helps you run, jump, pivot and push off the ground, basically every move an outfielder like Acuña makes in a single play. When it is tight, inflamed or partially torn, that springy propulsion becomes painful and unstable. Cue the limping, grimacing and, in some cases, weeks on the injured list.
Why Achilles Pain Is a Red Flag
Achilles tightness might sound like a minor complaint, but it is often the body’s early warning system. It could stem from overuse, fatigue, poor footwear, or biomechanical imbalances.In Acuña’s case, the discomfort reportedly began the night before while sprinting around the bases and got worse chasing fly balls. That is a classic setup: high-intensity bursts, sudden stops, and quick direction changes, all high-risk moves for the Achilles.
If ignored, tightness can escalate to tendonitis (inflammation), partial tears, or the dreaded rupture, which is basically the tendon snapping in two. That is a season-ending injury, often requiring surgery and months of rehab.
When the Body Says No
Beyond the physical pain, repeated injuries hit hard on the mental game. Acuña admitted he did not want to sit out, even though the pain intensified, because he has already missed too much time.But ignoring Achilles issues can backfire in the worst way. What starts as tightness today could be crutches tomorrow. The tendon does not heal fast, and re-injury is a very real risk if recovery is rushed.
The Game Plan for Recovery
For now, Acuña’s been placed on the 10-day injured list, but tendon issues do not always follow a schedule. He will likely undergo scans to rule out structural damage, followed by rest, anti-inflammatories, and physical therapy to stretch and strengthen the area.Recovery is not just about waiting for the pain to stop; it is about rebuilding strength, restoring flexibility, and ensuring both legs are balanced and strong.
Why This Matters for Everyone Who Plays
This is not just a pro-athlete problem. Achilles injuries are surprisingly common in runners, dancers, and gym-goers. If you feel stiffness in your heel or lower calf, especially first thing in the morning or during exercise, do not brush it off.Stretch regularly, warm up before activity, avoid sudden ramp-ups in intensity, and listen to your body. And if the pain lingers or worsens, see a specialist. Ronald Acuña Jr.’s Achilles flare-up might just be tightness, but it is the kind of tightness that turns trainers serious and fans anxious. It’s also a timely reminder that this tendon is small but mighty, and when it acts up, rest is not optional. Whether you are chasing fly balls or your morning run goal, treat your heels with the caution they deserve.
Manhattan Shooter Cited CTE in Suicide Note: Here Is What the Condition Means
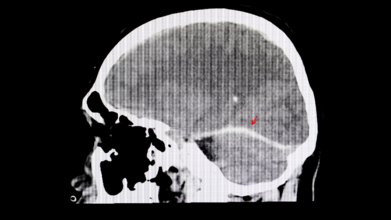
A recent tragic shooting in Midtown Manhattan has pulled an obscure but alarming brain disease back into the headlines. The shooter reportedly left behind a suicide note claiming he suffered from CTE, short for chronic traumatic encephalopathy, a condition linked to repeated head trauma. As shocking as the incident was, it has opened up a floodgate of questions: What exactly is CTE? Can it really make someone act out violently? And how can we even know if someone had it?
What Exactly Is CTE?
CTE is not your everyday concussion aftermath. It is a progressive, degenerative brain disease caused by repeated head injuries, the kind you get from rough contact sports, military service, or just too many unfortunate falls. Over time, these impacts seem to trigger the buildup of an abnormal protein in the brain called tau. This sticky substance does not just sit there quietly. It gradually spreads through the brain, messing with vital functions and causing serious, irreversible damage.The Symptoms
People with CTE do not wake up one morning knowing something is wrong. The symptoms can creep in slowly, subtle at first, then increasingly hard to ignore, leading to memory lapses, confusion, impulsive behaviour, unexplained aggression, mood swings, deepening depression and, in many tragic cases, suicidal thoughts.It is the sort of change that can feel like a personality transplant. Loved ones often report seeing someone “become a different person” over time.
Not Just a Pro Athlete Problem
For a long time, CTE seemed to be the unwanted souvenir of retired American football players. The sport's culture of full-body collisions made it the perfect storm for head trauma. But recent research is telling a more disturbing story. A 2023 study uncovered CTE in younger, amateur athletes, including teens as young as 17.Back to the Manhattan case. While the shooter’s note mentioned CTE, we still do not know whether he actually had it, let alone whether it influenced his behaviour. This brings up messy territory: should possible brain disease be considered in criminal responsibility? Can CTE be a mitigating factor in violent crime?
It is a grey zone. And until we develop reliable tools to diagnose CTE in the living, we are mostly left guessing.
What Can We Do?
CTE is a slow, silent thief, robbing people of their memory, emotions, and identity. And while scientists are racing to understand it better, prevention remains our best bet for now. That means:- Rethinking how we approach youth and professional sports
- Reducing repeated head trauma wherever possible
- Keeping an eye out for changes in behaviour following head injuries
What Is That One Thing That Makes Hepatitis So Dangerous?

Hepatitis is not nicknamed the “silent killer” for nothing. What makes it so dangerous is how symptomless it often is for years. It can quietly chip away at your liver without so much as a warning sign. By the time symptoms like fatigue, jaundice, or abdominal pain appear, significant harm may already have occurred. This eerie silence allows hepatitis to go undetected until it has done some serious damage.
Just Because You Cannot Hear It Does Not Mean It Is Not There
Dr Vikram Vora says that hepatitis is a major global health threat, killing over a million people each year. What is even more tragic? These deaths are, in his words, “largely preventable”. The villains in this tale, cirrhosis and liver cancer, often stem from untreated or undiagnosed hepatitis infections.
Prevention Helps
“The cornerstone of hepatitis control is prevention,” Dr Vora says. And the good news is that you have got some powerful tools at your disposal. “Vaccination, especially against Hepatitis B, is one of the most effective tools available,” he says, adding that infants, healthcare workers, and at-risk adults should be prioritised. Other prevention measures include safe injection practices, steering clear of needle-sharing, and ensuring blood transfusions are properly screened.
But danger often hides in plain sight. Dr Vora warns that something as seemingly harmless as getting a tattoo or piercing can carry lifelong consequences if done in an unregulated facility. His advice? “Choosing safe, licensed establishments is non-negotiable.”
Why You Should Not Wait for Symptoms
If there is one thing hepatitis is good at, it is staying undetected. That is why Dr Vora champions regular screening, especially if you have had medical procedures, blood transfusions, or close contact with someone infected. “Early diagnosis is a game-changer,” he says. Caught in time, hepatitis can be treated effectively, helping patients avoid severe liver disease or even make a full recovery.
A Diagnosis Is Not a Death Sentence
Dr Vora offers hope to those living with hepatitis. “With proper medical care and lifestyle adjustments, a healthy life is achievable,” he insists. That means ditching alcohol, sticking to a balanced diet, maintaining a healthy weight, and closely following medical advice. He also points out the mental and emotional toll a diagnosis can take. “Support from family, community, and healthcare providers can make a significant difference in outcomes.”
The Stigma That Silences
Perhaps just as damaging as the virus itself is the social stigma surrounding it. Dr Vora identifies this as a major hurdle in tackling hepatitis. “Fear of social exclusion keeps many from seeking help,” he explains. And that delay can cost lives. According to him, building a culture of empathy and understanding is critical. He encourages public health campaigns, education, and open dialogue as essential tools to dismantle this stigma.
Make Noise Against the Silence
In Dr Vora’s words, “Hepatitis may be silent, but it is not invincible.” Every little step, whether it is getting vaccinated, getting screened, or just talking about it, can chip away at the power hepatitis holds. Silence has cost too many lives already. Awareness can save them.
© 2024 Bennett, Coleman & Company Limited

