- Health Conditions A-Z
- Health & Wellness
- Nutrition
- Fitness
- Health News
- Ayurveda
- Videos
- Medicine A-Z
- Parenting
- Web Stories
Why Does Alcohol Make Your Sleep Faster?

Credit: Canva
Alcohol causes cancer, but it can also make you fall asleep faster and more deeply. If you have ever had alcohol, you might have experienced it yourself. Intrestingly, the sedative effects of alcohol are only felt in an environment that is quite, if you are in an active while drinking, you might not even notice it.
What Is Alcohol And How Does It Impact Your Sleep?
Alcohol is a chemical compound that typically refers to ethanol, the type found in alcoholic beverages like beer, wine, and spirits. It is produced through the fermentation of sugars by yeast, and when consumed, it acts as a depressant on the central nervous system.
Once alcohol reaches your brain, it impacts a neurotransmitter called gamma-aminobutyric acid (GABA) that slows down your brain's processing capability. This is why alcohol relaxes your mind. Alcohol also puts the brakes on an excitatory neurotransmitter called glutamate while tapping the reward centres of your brain. Due to this effect, having a drink or two before bed might actually calm down your central nervous system, making it easier for you to fall asleep. You might also notice a difference in your sleep quality. You sleep deeper and harder when you have alchohol in your system.
While wine, rum or other forms of alcohol can make you fall asleep almost immediately, it still might help disrupt your average sleep cycle. As per experts, the initial crash might make you believe you'll sleep better, but you will be missing on some of the REM sleep while alcohol is in your system. This is because once your body metabolises alcohol, your sleep will lighten and you are more likely to wake up frequently. You see, alcohol inhibits melatonin, a hormone that signals your body to sleep. Not only that, but alcohol interferes with the melatonin receptors in your brain.
However, that doesn't mean you should pop a melatonin gummy while sipping a can of bear. Combining alcohol and melatonin can make you even more drowsy or cause irritability. Alcohol already taxes your liver, and adding a melatonin supplement makes your liver work overtime. This weakens your liver's ability to produce certain enzymes, causing several side effects.
Alcohol's Impact On Your Brain
Primarily, alcohol interferes with the brain's communication pathways. According to the National Institutes of Health (NIH), alcohol can also alter how the brain looks and functions. It disrupts the areas of the brain responsible for balance, memory, speech, and judgment, increasing the likelihood of injuries and other negative outcomes. Long-term alcohol consumption can permanently change neural pathways, leading to lasting cognitive and emotional effects.
Moreover, it is a proven fact that alcohol can worsen mood swings. Recent research shows that alcohol may exacerbate symptoms of bipolar disorder by destabilizing mood, which impacts efficiency at work. Alcohol also affects conditions like depression, and panic disorder, and can trigger impulsive behaviour. Additionally, alcohol has been shown to disrupt sleep patterns, making it harder to get restorative rest.
Clint Eastwood’s Secret To Staying Young And Healthy At 95
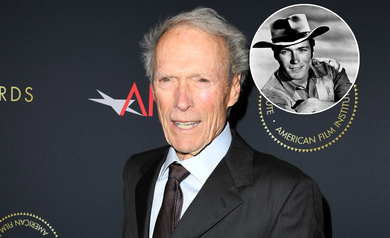
Credits: AFI
At 95, Clint Eastwood is still a testament to virility and understated strength still hard at work, incisive, and very much living on his own terms. Where most Hollywood actors depend on a battery of age-reversing tricks, Eastwood's technique lies in discipline, minimalism, and a decades-long dedication to healthy living. No gaudy supplements, no biohacking fads just plain sense tempered by routine.
Eastwood’s wellness journey began not in the gym or at a film set, but with the premature death of his father due to cardiovascular disease. That loss deeply impacted him, planting the seeds for a lifetime of preventive health practices. For Eastwood, longevity wasn’t a vanity project—it was a vow.
From then on, the actor-director doubled down on choices that would strengthen both his body and his mind. And while many in the entertainment industry were chasing the next health fad, Eastwood quietly adopted principles that science would later validate.
Meditation
One of Eastwood's most enduring health routines is Transcendental Meditation (TM), which he started in the 1970s. In contrast to many who practice mindfulness hit-or-miss, Eastwood has been a stickler—meditating regularly, sometimes twice a day, even when shooting a lot.
TM is the quiet repetition of a personally selected mantra for approximately 20 minutes, encouraging deep relaxation and "relaxed awareness." Research in peer-reviewed journals such as American Journal of Cardiology and Psychosomatic Medicine connects TM with decreased blood pressure, lowered cortisol levels, and enhanced cognitive performance.
Eastwood has attributed this discipline with keeping his head clear and his stress level in check. In a profession famous for mayhem and exhaustion, that clarity has probably helped not only his health, but also his remarkable productivity.
A Low-Fat, High-Impact Diet
Forget fancy detoxes or elimination diets. Eastwood’s dietary strategy is refreshingly practical. He opts for low-fat, nutrient-dense meals built around whole foods. That means lean proteins like salmon and chicken, paired with fibrous vegetables such as broccoli, asparagus, and dark leafy greens.
He keeps carbohydrates moderate and sugar intake minimal. No processed snacks or midnight nacho runs—when asked by Jimmy Kimmel if he indulged in wings or nachos, Eastwood’s response was clear, “None of that crap.”
This kind of diet supports metabolic health, reduces inflammation, and provides the steady energy needed for both physical activity and mental focus. And while he doesn’t follow any specific diet label—be it keto or paleo—the overall framework aligns with Mediterranean and Blue Zone dietary principles.
Hydration Over Hype
Another cornerstone of his health approach? Water. Eastwood is known to skip sugary beverages in favor of plain water. While that might seem minor, staying properly hydrated plays a critical role in cognitive clarity, digestion, and joint health—all especially important as we age.
Describing himself as a “lifelong gym rat,” Eastwood’s commitment to exercise hasn’t waned with age—it has simply evolved. In his younger years, he lifted heavy and trained hard. Now, the focus is on function and form.
He prefers low-impact activity: walking, golf, and light weight training. Instead of striving for personal bests, he values muscle protection, joint health, and equilibrium. As biographer Shawn Levy says, Eastwood's philosophy of fitness is deliberate and long-term: "He builds strength the way you build a house—brick by brick, rep by rep."
This mirrors advice from leading geriatric specialists, who emphasize the importance of strength training for older adults—not for aesthetics, but for mobility, fall prevention, and metabolic resilience.
Lessons to Learn From Clint Eastwood's Lifestyle of Longevity
What Eastwood demonstrates, without preaching, is that longevity isn’t the result of one miracle intervention—it’s the outcome of many small, deliberate choices repeated over time. And crucially, it’s not about perfection.
He doesn’t obsess over calorie counting or overtrain in the gym. Instead, he treats his body like a long-term investment. That includes managing stress through meditation, feeding it well through clean eating, and staying active through smart exercise.
It’s worth noting how much of his lifestyle overlaps with the habits of Blue Zone populations—those rare communities where people routinely live into their 90s and beyond. Things like daily walking, eating mostly plants, maintaining strong social ties, and managing stress effectively. Eastwood may not live in Sardinia or Okinawa, but he’s certainly aligned with the same timeless principles.
What is Transcendental Meditation?
The benefits of TM aren’t anecdotal. Clinical research has shown its impact on both physical and mental health. Studies from institutions like Harvard Medical School have documented reductions in stress, anxiety, and even symptoms of PTSD with regular practice.
TM also fosters better sleep quality, lower heart rate, and improved immune response. For an aging population, these are not just comfort perks—they are pillars of healthspan.
While not a substitute for medical treatment, TM can be a powerful complement to conventional care. And in Eastwood’s case, it’s a practice that has stood the test of time—five decades and counting.
What makes Clint Eastwood’s approach particularly noteworthy is its accessibility. There’s no need for expensive products, restrictive regimens, or tech-driven gimmicks. His longevity playbook is grounded in science, but also in discipline.
Healthy aging isn’t reserved for celebrities with personal trainers and private chefs. It’s achievable for anyone willing to prioritize their wellbeing and commit to the basics: nourish your body, move often, rest deeply, and manage your mind.
Hepatitis A To E: How Each Virus Affects Your Liver?

Credits: Canva
The liver doesn’t ask for much, but it does everything for you. It metabolizes nutrients, screens out poisons, synthesizes proteins, and aids in the digestion of your food. But when hepatitis strikes—a disease characterized by swelling of the liver—that whole system can become unbalanced. And the most likely culprits? The five viruses simply called hepatitis A, B, C, D, and E.
Each viral hepatitis type acts differently, transmits itself differently, and does its own kind of damage. Some resolve rapidly. Others lie dormant for years, silently harming the liver until it is too late. This makes learning about hepatitis—not as a disease but as a category of very different conditions—key to safeguarding long-term liver health.
When your liver becomes inflamed, it has difficulty doing its vital jobs—purifying your blood, making bile for digestion, storing nutrients, and helping to regulate clotting and metabolism. This inflammation may be acute (temporary) or chronic (longer than six months), depending on the cause and how your immune system reacts.
Hepatitis may be initiated by infections, toxins, autoimmune, or metabolic disorders, but the predominant offenders worldwide are viral infections. The viruses are segregated into hepatitis A through E, each with a different effect on liver cells and course of disease.
Hepatitis A
Hepatitis A is caused by the hepatitis A virus (HAV), usually spreading by food or water contamination. After entering the body, the virus takes the route of the bloodstream and reaches the liver. There, it infects liver cells and triggers the immune system to respond with inflammation.
This immune response results in the death of infected liver cells, and this can cause symptoms such as fatigue, jaundice, and gastrointestinal disturbance. Happily, HAV does not lead to chronic liver disease. The liver will normally regenerate completely after clearing the virus, and the majority of individuals recover in several weeks with no long-term effects.
All that being said, on occasion—most often in older individuals or individuals with existing liver disease—hepatitis A can result in acute liver failure. The liver gets so bogged down from inflammation that it temporarily ceases to function. Vaccination and proper sanitation are still the best defense.
Hepatitis B
Hepatitis B virus (HBV) is spread through blood, body fluids, or from mother to child at the time of birth. After entering the body, HBV infects liver cells and embeds its genetic material into them. The immune system destroys these infected cells, leading to extensive inflammation.
In most adults, the immune system eliminates the virus and the liver recovers. But not in all—particularly infants infected at birth—the virus persists. Chronic hepatitis B forms when the body's immune system fails to destroy the virus, resulting in prolonged inflammation and eventual loss of liver cells.
With time, this persistent immune attack can result in fibrosis (liver scarring), cirrhosis (severe, permanent scarring), and even liver cancer. What's particularly alarming is that chronic hepatitis B usually has no symptoms for decades. But below the radar, the virus quietly destroys liver tissue, cell by cell.
Vaccination prevents hepatitis B remarkably well, and antiviral medications can suppress the virus, stopping or slowing liver damage.
Hepatitis C
In contrast to HAV and HBV, hepatitis C virus (HCV) is transmitted nearly exclusively via the blood—usually through shared needles, untested transfusions (prior to 1992), or unsterilized medical procedures. Once infected by HCV, the liver starts to replicate the virus within liver cells, hiding from the immune system for years.
This sneaky virus hardly ever produces symptoms at the acute stage. Actually, most individuals don't even realize they are infected. But the liver doesn't remain unaffected. As HCV quietly multiplies, it causes low-grade inflammation that lasts for decades. The immune system acts against the infected cells, causing fibrosis.
Over time, chronic hepatitis C can lead to cirrhosis, in which scar tissue forms in place of healthy liver tissue. In later stages, the function of the liver declines, and the risk of liver failure and liver cancer accelerates. A liver transplant becomes the only recourse for many.
The better news? Direct-acting antiviral (DAA) treatments now cure greater than 95% of infections. Early diagnosis, however, is still important—once cirrhosis takes hold, the damage can be permanent, even once the virus is gone.
Hepatitis D
Hepatitis D, or HDV, is different from the others—it can't infect the liver by itself. It only exists in those already infected with hepatitis B, employing the outer shell of the HBV virus to replicate.
When HBV and HDV infect the liver concurrently (a co-infection) or if HDV is contracted later on superimposition of pre-existing HBV (a superinfection), the immune system is twice assaulted. The liver has to cope with more intense inflammation, resulting in more rapid fibrosis progression and much increased risk of cirrhosis and hepatocellular carcinoma.
In individuals with co-infection, liver injury is more severe, and complications arise years sooner than in HBV mono-infection. There are no specific therapies for HDV currently, and its management relies mostly on the control of hepatitis B.
It is also possible to prevent HBV infection and thereby hepatitis D by vaccination. Antiviral therapy and close follow-up can likewise decrease the chances of serious HDV complications in those already infected with HBV.
Hepatitis E
Hepatitis E virus (HEV) is transmitted primarily through water, which makes it prevalent in underdeveloped countries with inadequate sanitation. Upon entry into the body, it acts like HAV—producing an acute infection, liver inflammation, and a short duration of illness.
The vast majority of healthy individuals with hepatitis E recover uneventfully. The virus is naturally cleared, and the liver generally restores to normal completely. But in pregnant women, particularly in the third trimester, hepatitis E leads to acute liver failure and has a significantly increased risk of death. This is secondary to an overactive immune response and hormonal changes that exacerbate the liver's inflammatory process.
Hepatitis E can, in rare cases, become chronic, leading to long-term damage of the liver in some individuals, such as organ transplant recipients, especially those with weakened immune systems.
Prevention through clean water, sanitation, and hygiene and food safety is practiced in most countries where there are no widely available vaccines for hepatitis E.
What Are the Consequences of Chronic Hepatitis?
What links hepatitis B, C, and occasionally D is that they all have the potential to become chronic—i.e., the virus continues to cause liver inflammation over years or even decades. This ongoing low-grade inflammation leads to persistent scarring of liver tissue, called fibrosis.
As fibrosis progresses, it results in cirrhosis, with scar tissue dominating the liver, strangling its blood supply and function. The liver starts to fail. It is no longer able to process toxins, manufacture clotting factors, or metabolize drugs. Here, individuals are susceptible to internal bleeding, confusion, infections, and organ failure.
Even more concerning is the risk of hepatocellular carcinoma, a liver cancer primary to chronic hepatitis B and C. The chronic viral presence causes changes in DNA of liver cells, paving the way for malignant change.
What If Hepatitis Is Left Untreated?
Not treating hepatitis—especially the chronic stages—places you on a trajectory for irreversible liver damage. Even when you may not be feeling sick at present, inflammation can be quietly devouring your liver. Left untreated, this can culminate in lifelong disability, necessitate liver transplantation, or cut short lifespan from complications such as liver cancer.
In addition, untreated individuals can go on to infect others with hepatitis B or C by contact with blood or through sex. In pregnant women, hepatitis B and C can be transmitted to the unborn child at the time of delivery, which makes prevention and early treatment critical to the next generation.
Every year on July 28, World Hepatitis Day calls to mind that hepatitis remains a global health issue. More than 354 million individuals have chronic hepatitis B or C infection, unaware they are infected. It's not only an issue in low-income nations—people from all geographies and income groups are affected by hepatitis.
The date commemorates Nobel laureate scientist Dr. Baruch Blumberg, who discovered the hepatitis B virus and created the first vaccine. His legacy goes on saving millions of lives.
The World Health Organization's goal is ambitious, to eradicate viral hepatitis as a public health threat by 2030. But it begins with awareness, testing, vaccination, and access to life-saving treatment.
The liver is tough, but not forever. Once scarring sets in, there is no turning back. The sooner hepatitis is found, the better your chances of recovery and preventing long-term complications. With vaccines to prevent hepatitis A and B, and curative therapy for hepatitis C, the means are at hand.
If you’ve never been tested for hepatitis, especially if you’ve had a blood transfusion before the 90s, were born to an infected mother, or engaged in high-risk behaviors now is the time. Your liver’s future depends on it.
What Is The 'Asian Glow'? Is It Just Body's Reaction To Alcohol Or Something More Dangerous?

Credits: Canva
Commonly nicknamed the “Asian glow” or “Asian flush,” alcohol flush reaction is a physical response to drinking alcohol seen predominantly in people of East Asian descent.
This condition is marked by a reddening of the face, increased heart rate, and sometimes nausea or headaches shortly after consuming alcohol.
About 560 million people worldwide, which makes it roughly 8% of the global population, carry a genetic mutation called ALDH2*2 that causes this reaction. An estimated 45% of East Asians experience flushing when they drink, and many use antihistamines to mask the symptoms.
But researchers warn that these visible reactions are more than just a cosmetic issue, they’re a red flag indicating a heightened vulnerability to serious diseases.
What Causes It?
The root cause of alcohol flush reaction lies in how alcohol is metabolized in the body.
Normally, alcohol is broken down in two steps.
- First, it is converted into acetaldehyde, a compound far more toxic than alcohol itself.
- Then, acetaldehyde is quickly broken down into acetate by an enzyme called aldehyde dehydrogenase 2 (ALDH2), which the body can safely eliminate.
However, in people with the ALDH2*2 mutation, this second step is impaired. Their version of the ALDH2 enzyme has little to no activity, causing acetaldehyde to accumulate in the bloodstream. This toxic buildup is what leads to the flushing and other symptoms.
The World Health Organization classifies acetaldehyde as a Group 1 carcinogen, meaning there is strong evidence that it causes cancer in humans. Even with moderate alcohol intake—such as two beers, the acetaldehyde levels in people with this mutation can reach carcinogenic levels.
Why It’s Dangerous
While many consider alcohol flush reaction an inconvenience, the health risks it signals are far more serious. Experts have linked the ALDH2*2 mutation with significantly elevated risks for several life-threatening conditions if alcohol consumption continues.
People with the mutation who drink moderately (defined as two drinks per day for men and one for women) have a 40 to 80 times higher risk of developing esophageal cancer compared to those without the mutation. The risk increases with the amount of alcohol consumed, making it a dose-dependent danger.
The mutation is also associated with higher risks of:
- Head and neck cancers
- Gastric (stomach) cancer
- Coronary artery disease
- Stroke
- Osteoporosis
Importantly, these elevated health risks are not seen in non-drinkers with the same mutation, highlighting that alcohol intake is the trigger.
Why Antihistamines Don’t Help
Many young people, particularly college students, take over-the-counter antihistamines like Pepcid AC or Zantac to reduce the visible symptoms of alcohol flush reaction. While these drugs may lessen skin flushing by reducing blood vessel dilation, they do nothing to prevent the dangerous accumulation of acetaldehyde in the bloodstream.
Experts caution that using antihistamines this way is risky. By masking the body’s warning signals, individuals may end up drinking more than they should, unknowingly increasing their health risks.
A Problem of Awareness
Despite the potentially deadly consequences, awareness of the ALDH2*2 mutation remains low.
The variant is believed to have originated from a single individual in Southeast China 2,000 to 3,000 years ago. Today, its prevalence is highest in Taiwan (49 percent), Japan (40 percent), China (35 percent), and South Korea (30 percent). Yet, alcohol consumption in East Asia continues to rise.
Between 1990 and 2017, alcohol use in East Asia increased from 48.4 percent to 66.9 percent. The region now bears the highest burden of alcohol-attributable cancers globally, with 5.7 percent of all cancer cases linked to alcohol, nearly double the rate in North America.
Many people still believe that facial flushing from alcohol is harmless or even a sign of a strong liver. In fact, it’s a clear signal of toxicity and should not be ignored.
Raising Public Education and Health Literacy
Efforts to raise awareness are growing. In Taiwan, researchers and health advocates founded the Taiwan Alcohol Intolerance Education Society, which collaborates with government agencies to educate the public. The group launched National Taiwan No Alcohol Day on May 9, with “5-9” sounding like “no alcohol” in Mandarin, a clever linguistic nudge toward abstinence, as reported by the Washington Post.
Research also suggests that personalized health information can help. A study conducted among Asian American young adults found that those who were informed about their genetic risks related to the ALDH2*2 variant reduced both their drinking frequency and volume over the following month.
Experts emphasize that the message is clear: if you experience alcohol flush reaction, your body is sounding an alarm. Ignoring it may come at a serious cost.
© 2024 Bennett, Coleman & Company Limited




