- Health Conditions A-Z
- Health & Wellness
- Nutrition
- Fitness
- Health News
- Ayurveda
- Videos
- Medicine A-Z
- Parenting
Why Everyone Is Suddenly Talking About Ivermectin As A Cancer Breakthrough?
A PubMed search for “ivermectin” and “cancer” yields hundreds of preclinical studies, many conducted on cell cultures or mice. In the sector of alternative cancer treatments, few drugs have generated as much buzz—and controversy—as ivermectin. Once lauded for its ability to treat parasitic infections and awarded a Nobel Prize for its contribution to global health, ivermectin has more recently been at the center of misleading narratives, first as an alleged cure for COVID-19 and now as a so-called “cancer breakthrough.”
Social media, podcasts, and even some patient communities are abuzz with stories of miraculous recoveries and scientific “breakthroughs.” But what’s driving this surge of interest, and does the science live up to the hype?
For decades, ivermectin was best known as a safe and effective treatment for parasitic diseases like river blindness and scabies. Its impact was so significant that it earned its discoverers the Nobel Prize in 2015. But after being widely discredited as a COVID-19 treatment, ivermectin found new life in online cancer forums and alternative health circles, where it’s now promoted as a cheap, accessible alternative to mainstream cancer therapies.
The renewed interest in ivermectin as a potential cancer therapy has largely been driven by non-scientific sources. On platforms like X (formerly Twitter), Substack, and YouTube, influential figures promote ivermectin as a natural, low-cost cure "suppressed by big pharma."
One viral moment came during a widely viewed episode of The Joe Rogan Experience, in which actor Mel Gibson recounted how three friends with stage IV cancer reportedly became cancer-free after taking ivermectin and fenbendazole. That snippet, viewed by nearly 20 million people, has fueled speculation—despite the anecdotal nature of the claims.
Further fanning the flames, public figures like Robert F. Kennedy Jr. have accused health authorities of deliberately suppressing ivermectin to favor profit-driven cancer treatments—a claim lacking credible evidence but resonating with those distrustful of traditional medicine.
What Is Ivermectin Approved For?
Ivermectin is a U.S. FDA-approved antiparasitic drug, used for treating river blindness (onchocerciasis), strongyloidiasis, lice, and scabies in humans. It’s also commonly used in veterinary medicine to treat parasitic infections in animals.
Its development and application in tropical medicine were so impactful that the researchers behind ivermectin received the Nobel Prize in 2015. However, its uses have always remained confined to parasitic infections—not viral illnesses like COVID-19, and certainly not cancer.
How Ivermectin Might Work Against Cancer?
Ivermectin’s anticancer effects appear to be unrelated to its anti-parasitic action. Instead, the drug disrupts cancer cell signaling, impairs mitochondrial function, induces autophagy (a process that can kill cancer cells), and inhibits cancer stem cells. It also weakens the mechanisms that allow tumors to resist chemotherapy and evade the immune system.
In the Brazilian rat study, nano-encapsulated ivermectin not only shrank tumors but also improved the health of surrounding brain tissue and reduced abnormal blood vessel growth—suggesting multiple avenues of attack against cancer.
What the Science Says About Ivermectin and Cancer?
A search of scientific literature reveals hundreds of studies linking ivermectin to cancer research. Some of these suggest that ivermectin may interfere with cancer cell metabolism, inhibit tumor growth, or boost immune response in lab-controlled environments. But—and this is critical—lab results do not equal human results.
Dr. Peter P. Lee, chair of the Department of Immuno-Oncology at the Beckman Research Institute of City of Hope, has studied ivermectin's immune-stimulating effects in mice. While findings hinted at some tumor-modulating potential, they fell far short of demonstrating therapeutic value in humans.
At the 2025 American Society of Clinical Oncology (ASCO) Annual Meeting, early results from a phase 1/2 trial combining ivermectin with immunotherapy in metastatic triple-negative breast cancer patients showed no significant benefit. Of the eight patients evaluated, six experienced disease progression, one had a partial response, and one achieved stable disease.
Risks of Using Ivermectin as a Cancer Therapy
Promoting ivermectin for cancer without evidence carries several dangers:
Neurological toxicity: High doses can lead to seizures, confusion, blurred vision, or even coma.
Drug interactions: Ivermectin can interfere with common cancer medications, such as blood thinners or immunotherapy agents.
Treatment delays: Perhaps most concerning is the risk that patients may delay or forgo evidence-based cancer treatments in favor of unproven, alternative drugs. Such delays can allow the cancer to progress unchecked.
False hope and financial exploitation: Some patients may spend time, money, and emotional energy pursuing unproven remedies, only to face worsening outcomes.
Why the Sudden Surge in Popularity?
Several factors have converged to make ivermectin a hot topic in cancer circles. Social media amplification has played a major role, with influencers and alternative health advocates promoting ivermectin as a cheap, “natural” alternative to mainstream cancer treatments. These promotions often rely on cherry-picked studies or anecdotal stories of success, rather than clinical evidence. Distrust in conventional oncology also fuels interest—many patients, disillusioned by the side effects, financial burden, or perceived limitations of standard therapies, are increasingly drawn to off-label or experimental alternatives like ivermectin.
Preclinical breakthroughs, such as the much-publicized Brazilian nano-ivermectin study in animals, add to the intrigue by generating hopeful headlines, despite lacking human trial data. Finally, political and cultural overtones stemming from ivermectin’s controversial use during the COVID-19 pandemic have transformed the drug into a rallying point for individuals skeptical of established medical authorities, further complicating the public narrative around its potential role in cancer treatment.
Where Does This Leave Patients and Doctors?
While the science around ivermectin and cancer is evolving, the consensus among oncologists and researchers is clear: There is no solid evidence that ivermectin can cure or significantly treat cancer in humans. The most promising findings are still limited to laboratory and animal studies, and ongoing clinical trials have yet to show meaningful benefit in people.
That said, the safety profile in small studies is reassuring, and the innovative use of nanotechnology to deliver ivermectin to brain tumors is a genuine scientific advance—one that warrants further research but not premature celebration.
Curiosity Is Good—But Let's Stick to the Science
The buzz around ivermectin as a cancer cure is based more on anecdotes and viral claims than on real science. While early lab data may inspire future studies, there is currently no evidence that ivermectin can treat or cure cancer in humans. Ivermectin’s journey from Nobel-winning anti-parasitic to cancer “miracle drug” is a testament to both the power of scientific curiosity and the dangers of viral misinformation.
Patients facing cancer deserve hope—but not false hope. Turning away from proven therapies in favor of unproven ones could have devastating consequences.
Why Do Sinus Problems Spike In Winter? Doctor Reveals

Credits: Canva
As winter approaches, many people notice an increase in sinus- and ear-related issues. Symptoms such as nasal congestion, facial pressure, headaches, ear pain, and dizziness become more frequent during this season. According to Dr. Swapnil Brajpuriya, Associate Director & Head Unit II – ENT at Asian Hospital, the combination of cold air, low humidity, and sudden temperature changes are the main reasons why sinus and ear problems worsen in winter.
Why Does Cold Air Cause Sinus Blockage?
The sinuses are air-filled cavities within the facial bones that connect to the nose and play a key role in the breathing process. During winter, the cold, dry air dries out the nasal lining, causing the mucus to thicken. Thickened mucus slows down normal sinus drainage, leading to congestion and blockage.
Dr. Brajpuriya explains, “In winter, the nasal mucous membrane tends to dry out, preventing proper drainage of mucus from the sinuses. This leads to congestion and sinus blockage.”
The Link Between Ear Heaviness, Headache, and Dizziness
The sinuses and ears are connected via the Eustachian tube, which regulates pressure between the middle ear and the environment. When sinus inflammation or blockage occurs, it can create pressure in the ears, causing a feeling of fullness, reduced hearing, headaches, and sometimes dizziness.
“Sinus infections can block the Eustachian tube, causing pressure buildup inside the ear. This pressure is often responsible for the headaches and dizziness experienced by patients,” says Dr. Brajpuriya.
Why Are Infections More Common in Winter?
Winter months often mean spending more time indoors in closed, crowded spaces, which increases the risk of viral and bacterial infections spreading. Additionally, colder temperatures and seasonal changes can weaken the immune system, making common colds and flu more likely to develop into sinusitis or middle ear infections.
Dr. Brajpuriya adds, “If a cold or flu is not treated promptly, it can progress to a sinus or middle ear infection, particularly in children and the elderly.”
Who Should Be Extra Careful?
Certain groups are more susceptible to sinus and ear problems during winter. People with allergies, asthma, frequent colds, weak immunity, or pre-existing sinus conditions need to be extra vigilant. Smokers are also at higher risk, as smoke can irritate the nasal and sinus lining, exacerbating congestion and inflammation.
Sinus Treatment and Prevention Tips
To manage and prevent winter-related sinus and ear issues, Dr. Brajpuriya recommends the following precautions:
- Keep your nose and ears protected from cold air using scarves or masks.
- Stay hydrated by drinking plenty of water to keep mucus thin.
- Minimise exposure to dust and allergens indoors.
- Seek medical advice if nasal congestion, ear pain, or dizziness persists for more than a few days.
He emphasizes, “Neglecting sinus and ear problems can lead to chronic infections. Timely treatment and proper care are essential to prevent complications.”
Cold air, dry weather, and viral or bacterial infections are the key factors behind the increase in sinus and ear problems during winter. With simple preventive measures, adequate hydration, protecting the nose and ears, and seeking early medical care, most people can manage these seasonal issues effectively and reduce the risk of complications.
Taking Diazepam Or Alprazolam? Four Warning Signs Doctors Say You Must Watch For

Credits: AI Generated
A pharmacist has raised concerns for an estimated 4.8 million people in the UK who may be taking medicines such as diazepam or alprazolam. Fresh findings from Oxford Online Pharmacy suggest that one in five adults has obtained prescription-only drugs through illegal means. Anti-anxiety medicines top the list. Based on current population estimates, this could involve up to 4.8 million adults.
Another 10 percent of respondents said they had been offered medicines from unlicensed and unlawful sources, including online sellers, salons, corner shops, or even friends and family, although they chose not to take them.
As part of the study, a nationally representative group of UK adults was asked whether they had bought, received, or been offered medication from an unlicensed source. Among those who said yes, more than a third, around 35 percent, reported obtaining anti-anxiety medicines. These included selective serotonin reuptake inhibitors (SSRIs), serotonin-norepinephrine reuptake inhibitors (SNRIs), and benzodiazepines such as Valium (diazepam) and Xanax (alprazolam), according to a report by the Mirror.
What Are Diazepam And Alprazolam Used For?
Diazepam, sold under the brand name Valium, and alprazolam, commonly known as Xanax, belong to a group of medicines called benzodiazepines. They work by calming activity in the brain and are mainly prescribed to manage anxiety. Diazepam is also used to treat seizures, muscle spasms, and symptoms of alcohol withdrawal.
Alprazolam, on the other hand, is more commonly prescribed for panic disorder. Diazepam stays in the body for longer, which makes it useful in withdrawal treatment, while alprazolam acts more quickly and is often chosen for sudden panic symptoms. Both medicines slow down the central nervous system to ease anxiety, but because of their effects and differences in how long they last, they should only be used under close medical guidance, as per Medicine Net.
Diazepam And Alprazolam: Why Are Doctors Warning Against It?
Kiran Jones, a clinical pharmacist at Oxford Online Pharmacy, has issued a strong warning for anyone thinking about using, or already using, anti-anxiety medicines sourced from the black market. “Anxiety is the most common mental health condition worldwide. At any given time, around 4 to 5 percent of people are living with an anxiety disorder. With such high numbers, it is not surprising that there is a growing illegal market for anti-anxiety drugs alongside those prescribed by qualified healthcare professionals. However, this trend is deeply worrying,” Jones said.
She explained that some benzodiazepines bought illegally are made to look like genuine prescription medicines but are actually counterfeit. These fake pills may contain extremely dangerous or even fatal substances, including synthetic opioids such as fentanyl. There is also a significant risk of addiction with these medicines, especially when they are taken over long periods. Over time, the body can develop tolerance, meaning higher doses are needed to achieve the same effect, which can quickly lead to dependence.
According to doctors and NHS guidance, there are several red flags people should be aware of:
Medication Appearance
If you have previously taken anti-anxiety medication, you may notice differences in the size or shape of tablets compared to what you were originally prescribed. If you are unfamiliar with the medicine, it is important to check online what the genuine product should look like and what the usual dosages are. You might also spot spelling mistakes in the drug name, manufacturer details, or listed ingredients, as well as differences in packaging design.
As per Mirror, these are often clear warning signs of a fake product. Proper packaging should always be sealed. If it appears opened, tampered with, or simply seems off, you should not take the medicine.
Medication Quality
Genuine medicines are produced to a consistent standard and should look uniform. Tablets should not be cracked, unevenly coated, or crumble easily when touched. Any signs of mould inside blister packs or containers should be treated as a serious warning sign.
You Have To Pay In Cash Or Via Bank Transfer
Reputable pharmacies and healthcare providers use secure and traceable payment systems. Requests for cash payments or bank transfers are commonly used by illegal sellers to avoid being identified and to keep transactions untraceable.
This lack of traceability makes it much harder to report scams, track down sellers, or get help if something goes wrong. If you come across an online provider and are unsure whether it is legitimate, you should check whether it is registered with the General Pharmaceutical Council before making any purchase. The UK government’s FakeMeds campaign also offers practical guidance on how to identify suspicious online sellers.
Disclaimer: This article is for general information only and should not be taken as medical advice. Always consult a qualified doctor, pharmacist, or healthcare professional before starting, stopping, or changing any medication, especially if you have an existing medical condition, are pregnant, breastfeeding, or taking other drugs.
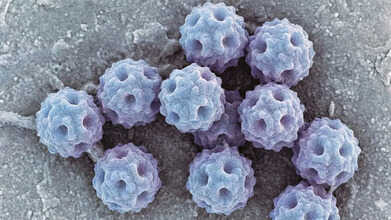
Norovirus Cases Rise In The UK: How To Avoid Catching The Winter Vomiting Bug
Credits: AI Generated
Winter creates the perfect setting for coughs, colds, and stomach bugs. With people spending longer hours indoors, infections pass from person to person more easily. Right now, one virus in particular is spreading fast across the UK.
Norovirus, often referred to as the winter vomiting bug, is circulating widely. Several NHS trusts have announced a “critical incident” after a sharp rise in hospital admissions linked to norovirus and flu. A critical incident is declared when Accident and emergency departments are no longer able to provide all services safely.
With cases climbing this winter, many are asking the same question: how can you protect yourself from catching the winter vomiting bug?
What Is Norovirus?
Norovirus is one of several viruses that infect the gut and cause symptoms such as diarrhoea, vomiting, and stomach cramps. These symptoms can continue for a few days and, in some cases, may lead to severe dehydration. Outbreaks are often reported in settings like cruise ships, nurseries, and care homes. You may have heard it called the “cruise ship virus.” These environments make it easier for the virus to spread because people are in close contact and often share food and drink sources.
Norovirus Symptoms To Take Note Of
Symptoms of norovirus typically appear between 12 and 48 hours after exposure, according to the California Department of Public Health (CDPH). People may experience repeated bouts of vomiting and diarrhoea throughout the day, with symptoms usually lasting one to three days.
As per the NHS, other symptoms include:
- Nausea and vomiting, often sudden and intense.
- Diarrhoea with loose, watery stools.
- Abdominal pain, including cramps and discomfort.
- Body aches, such as muscle pain and general weakness.
- Headaches.
- A mild fever.
Norovirus: How Can You Avoid Getting The Winter Vomiting Bug?
Try not to eat food prepared by anyone who is unwell or has recently been sick, although this is not always easy to manage. One of the most effective precautions is regular handwashing. Clean your hands with soap and water for at least 20 seconds, especially at key moments.
A useful habit is to wash your hands before putting anything in your mouth. This becomes even more important in group settings or if you are near someone who is ill.
If norovirus is a concern, make sure to wash your hands before eating in these situations:
- At shared meals, after serving dishes have been passed around and you have filled your plate.
- While snacking, if you are using shared utensils or pouring drinks from a communal bottle.
- After shaking hands when greeting people at gatherings involving food or drinks.
- In restaurants, after touching shared items such as menus or buffet and salad bar utensils.
- At work, if you are eating while using a computer or shared equipment.
- If washing your hands is not possible before handling food, it may be safer to eat using utensils only.
With proper care, most people bounce back from norovirus without complications. Staying well hydrated, getting enough rest, and managing symptoms should be your focus, while strict hygiene and isolation help stop the virus from spreading to others.
© 2024 Bennett, Coleman & Company Limited

