- Health Conditions A-Z
- Health & Wellness
- Nutrition
- Fitness
- Health News
- Ayurveda
- Videos
- Medicine A-Z
- Parenting
Why Placenta Banking Is Being Called the Ultimate Health Insurance for Families
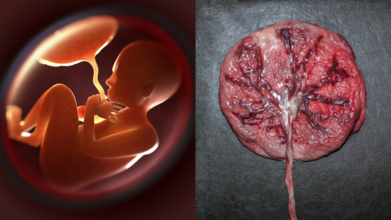
Credits: Canva
If you thought the only souvenirs from childbirth were baby pictures and tiny socks, times have changed. Turns out, the real treasure might be something most parents never even glance at before it is thrown away: the placenta and umbilical cord. Doctors are now calling placenta banking “biological insurance”, and the idea is picking up pace.
Your Baby’s Placenta Is More Than Just Leftovers
For centuries, the placenta has been treated as medical waste. But according to Dr. D.B. Usha Rajinikanthan, Senior Consultant in Gynaecology and IVF at SIMS Hospital, Chennai, this organ is brimming with stem cells that could be life-saving later on.
“Placenta and cord blood contain stem cells that can repair or replace damaged tissue. Collecting them at birth is safe and painless, but once discarded, that opportunity is lost forever,” she says.
These tiny cells are essentially the body’s master builders, with the potential to transform into different blood and immune cells. Which means what is usually thrown in a bin could actually hold a family’s medical safety net.
Why Stem Cells Are a Big Deal
Stem cells from the placenta are not just versatile; they are generous. Dr. Rajinikanthan explains that they have already been used to treat more than 80 diseases worldwide, including leukaemia, certain immune deficiencies and metabolic disorders. “Research is expanding into conditions like heart repair, brain injury and even diabetes,” she adds.
Placental stem cells are “younger” and more flexible, making them easier to match with siblings and relatives. In simple terms, the baby, siblings, parents and even grandparents may stand to benefit. It is not just your child’s resource; it is potentially a family heirloom.
Placenta Preservation: A Health Insurance
If we insure our cars and houses against accidents, why not our health? Placenta banking works on that philosophy. “It is a one-time investment in future health security. Families may never need it, but having stored stem cells gives enormous peace of mind,” says Dr. Rajinikanthan. She emphasises, though, that choosing an accredited stem cell bank that follows quality standards is essential.
How Does Amniotic Membrane Help?
Beyond the cord blood, there is another underrated star, the amniotic membrane. Dr. A. Jaishree Gajaraj, Head of Obstetrics and Gynaecology at MGM Healthcare, Chennai, explains that the amnion has been saving lives for over a century. “The first use dates back to 1910 when it was applied as a skin graft to promote healing. Today, it is used in ophthalmology for dry eyes, as well as for burns and diabetic ulcers,” she says.
In other words, this part of the placenta is not just a wrapper for your baby; it is a medical toolkit waiting to be tapped.
The Science Behind the Promise
Stem cell science has moved leaps and bounds in recent decades. According to Dr. Gajaraj, the umbilical cord blood and tissue have already been used successfully in bone marrow transplants for children with leukaemia and other bone marrow disorders. But the real buzz is around their future potential.
“These pluripotent cells are being researched for regenerating organs like the pancreas, liver, lungs and even the spinal cord. While still experimental, the promise is extraordinary,” she explains.
She adds that mesenchymal stem cells (MSCs), particularly those derived from cord tissue, are showing the greatest promise in regenerative therapies. “Foetal MSCs from cord tissue expand better, are less likely to trigger immune rejection, and have higher therapeutic potential than their maternal counterparts,” says Dr. Gajaraj. Simply put, storing placenta and cord tissue maximises the number and types of cells available for future therapies.
But What About Delayed Cord Clamping?
Some parents worry that opting for placenta banking might compromise delayed cord clamping, the practice of waiting a few minutes before cutting the cord to allow extra blood flow to the baby. Dr. Gajaraj reassures that this is not the case. “Delayed clamping does not reduce the yield of mesenchymal stem cells. Parents can safely choose both practices,” she says.
A Gift From Your Newborn to the Whole Family
Placenta banking is not a crystal ball or a cure-all. It does not guarantee immunity against every illness. But as both doctors point out, it offers a shot at future treatments that could transform outcomes in life-threatening conditions
Why Pap Smear Is Non-Negotiable After 30 And Why So Many Women Still Avoid It | Women's Day Special

Credit: iStock
Vaccinated for human papillomavirus (HPV)? Now, take that Pap smear test. This is the most common advice women hear to prevent the risk of cervical cancer that annually causes around 6,60,000 new cases and around 350,000 deaths worldwide.
However, it's easier said than done for most of the fairer sex.
A Pap smear is typically a gynecological examination where a speculum is inserted to collect cells from the cervix.
Although the procedure is brief and generally safe, the discomfort discourages many from getting screened. Fear of pain, anxiety of the results, form the common psychological barriers worldwide, and is followed by shame, cultural attitudes, and concerns with male clinicians.
A study in Iran, published in the BMJ Open journal in January 2024, showed that psychological stress, cultural issues, and fear, along with limited information and health services, were the biggest hindrances to getting Pap tests.
Another research published in the BMC Women's Health in December 2022, focusing on Africa, Asia, and South America, reported that many women avoided or delayed Pap smears because they are afraid the procedure will hurt. Many also reported being embarrassed about the pelvic exam or fear of having a stranger see their private areas. Some also worried that the test could damage the uterus.
A Pap Smear test, however, is proven to be safe and is recommended for every woman above the age of 21 years.
“A Pap smear is a rapid, safe, and painless screening procedure that detects irregular cellular changes well before they become malignant. The ability to treat at this pre-cancerous stage of disease provides an excellent outcome,” Dr. Tirathram Kaushik, Senior Consultant GI, HPB, Gastrointestinal & Thoracic Oncology and Robotic Surgery, HCG Cancer Centre, Borivali, told HealthandMe.
A 2025 study, published in the Journal of Contemporary Clinical Practice, showed that pap smears are excellent at ruling out precancerous risks. It also remains a valuable screening tool where molecular testing is limited.
There are many myths about Pap smears that make people anxious or avoid screening. Let’s clear up the most common ones:
Pap Smears Are Painful
The most common myth regarding pap smear screening is that it is painful, unnecessary, or only required when symptoms are present.The Pap smear procedure, which takes only a few minutes, is often described as uncomfortable. While some feel like a quick pinch, others experience slight discomfort or spotting. Severe pain is not considered normal.
“From an oncology perspective, this myth results in a delay in diagnosis. Cervical cancer often occurs silently in its early stages, without any noticeable symptoms,” Kaushik said.
I Am Healthy, So I don’t need A Pap Smear
Some people believe that if they feel healthy, they don’t need a Pap smear. However, HPV can cause early cervical cell changes, which usually produce no symptoms.While individuals may feel completely well, they still have abnormal cells developing silently. As a result, regular Pap smear screening is important because it detects these changes early -- before they turn into cervical cancer.
“The HPV infection and subsequent changes that lead to cervical cancer happen slowly over many years. HPV infection is also very common, and one in two women is likely to get infected. Regular screening by a Pap smear will help to catch infection early before it can convert into cancer,” Dr. Deepak Jha, Chief - Breast Surgery & Sr. Consultant Surgical Oncology, Artemis Hospitals, told HealthandMe.
I Have Only One Partner, So I don’t need Screening
HPV can be transmitted even in monogamous relationships. Your partner may have been exposed to HPV before, and the virus can stay in the body for years without symptoms.“HPV doesn’t need penetrative sex for infection. It can be transferred if there is any contact of bodily fluid. It’s always safe to test and be assured rather than repent later,” Dr. Jha said.
Testing Means Cervical Cancer
Many women worry that testing automatically means cancer, which is not true. Screening is preventive, and most results are normal.“Even if HPV is detected, it usually indicates a pre-cancerous stage that is highly treatable,” Dr. Parminder Kaur, Consultant Gynecologic Oncologist at CK Birla Hospital, Delhi, told HealthandMe.
Moreover, a Pap smear only screens for cervical cancer; it can’t detect other gynecological cancers such as cervical, ovarian, uterine (endometrial), vaginal, and vulvar cancers. So, screening and appropriate tests for those will be required, irrespective of the Pap smear.
I Am old, So I don’t need A Pap Smear
HPV infection happens at an early age, so merely old age is not enough to stop Pap smear. At least three consecutive negative screens (minimum three-yearly Pap smears or five-yearly HPV screens) would be needed in this situation.I Got Vaccinated, So I Do Not Need A Pap Smear
The vaccine covers the major variants of the HPV virus, but there is still a small probability of cervical cancer due to the uncommon HPV variants.Irrespective of vaccinated status, a woman should go for regular screening between the ages of 25 and 79. Also, if a woman already had HPV exposure before being vaccinated, she would not benefit, the experts said.
“Screening is not just a routine procedure - it is a preventive measure. In the treatment of cancer, early detection alters the disease course, whereas waiting for symptoms to develop means the disease is likely to be already advanced,” Dr. Kaushik said.
Dr Kaur called for more awareness and stated that open discussion are key to help more women take the important screening test.
When To Get Screened
The United States Preventive Services Task Force (USPSTF) and the American Cancer Society (ACS) recommend getting your first Pap test at age 21, followed by Pap testing every 3 years. Even if you are sexually active, you do not need a Pap test before age 21.
- Individuals must start getting Pap tests at age 21. If the result is normal, repeat the test after three years.
- For individuals aged between 30 and 65 years old, doctors are likely to recommend an HPV test along with a Pap test. If both are normal, repeat after five years.
In women older than 65, you don't need to be screened anymore if:
- You have had at least three Pap tests or two HPV tests in the past 10 years, and the test results were normal or negative, and
- You have not had a cervical precancer in the past, or
- You have had your cervix removed as part of a total hysterectomy for non-cancerous conditions, like fibroids.
Long Covid Causes Lasting Brain Inflammation And Lung Injury, Reveals Study

Credit: Canva
Are you still experiencing brain fog, fatigue, and mood changes even after years of a mild COVID-19 infection? A new study showed that the SARS-CoV-2 virus, behind the COVID infection, can cause persistent brain inflammation and lung injury, according to a study.
Researchers from Tulane University, in Louisiana, US found that the brain inflammation lasts long even after the virus was no longer detectable.
Their study, published in Frontiers in Immunology, can answer why long COVID often includes neurological symptoms such as brain fog, fatigue, and mood changes.
"Long-term effects on the brain were unique to SARS-CoV-2. That distinction is critical to understanding long COVID," said lead author Dr. Xuebin Qin, professor of microbiology and immunology at the Tulane National Biomedical Research Center. Qin also mentioned "lasting lung injury" among COVID patients.
In a mouse model, the team found that immune cells in the lungs failed to fully stand down and also spiked the buildup of collagen -- a protein associated with scarring.
The changes stiffened lung tissue, making breathing feel more labored -- a possible answer to breathlessness faced by COVID survivors.
Further, the researchers also noted no repair to the injury, suggesting the virus may interfere with the lung's natural healing process.
On the other hand, in the brain, the mice with COVID showed signs of persistent brain inflammation weeks later. The team also reported tiny areas of bleeding.
Conducting a gene expression analysis, the team found ongoing inflammatory signaling and disruption of pathways involved in serotonin and dopamine regulation -- brain functions linked to mood, cognition, and energy levels.
What Is Long COVID?
Long COVID is a collection of symptoms that last three months or longer after your first COVID symptoms. They include fatigue, brain fog, headaches, breathlessness, altered sense of smell or taste, headaches, and more.
While many of the Long conditions remain to be fully recognized, some people have more than one symptom.
mRNA Vaccine Against COVID
As per recent data from the World Health Organization, more than 43,000 new cases have been reported from 61 countries, between January and February.
Vaccination that prevents SARS-CoV-2 infection is the most effective way to prevent long COVID.
Recently, the European Medicines Agency (EMA) recommended a marketing authorisation in the European Union (EU) for mCombriax -- a messenger RNA vaccine for protecting people aged 50 years and older against COVID-19 and seasonal influenza (flu).
Co-infection with the influenza virus and SARS-CoV-2 can result in more severe disease than would occur with either SARS-CoV-2 or influenza virus infection alone.
mCombriax works like other vaccines by preparing the body to defend itself against infection. It contains messenger RNA with instructions for making proteins found on SARS-CoV-2 and the following seasonal influenza viruses: influenza type A-H1N1, influenza type A-H3N2, and influenza type B of the Victoria lineage.
Feeling Tired And Foggy? It Could Be Vitamin B12 Deficiency

Credit: Canva
Vitamin B12 might sound like just another nutrient on a health label but it plays a major role in how your body works. The vitamin is crucial in helping the body produce red blood cells, supports your nervous system and essential for making DNA, which is the genetic material inside all your cells.
Symptoms of a Vitamin B12 deficiency often appear slowly. You may not notice them at first, or may blame them on stress, lack of sleep or a busy schedule. However, if this deficiency continues for too long, it could lead to serious health problems.
Here are three key signs to look out for:
1. Ongoing Fatigue and Weakness
Vitamin B12 is extremely crucial for making red blood cells who are responsible for carrying oxygen from your lungs to the rest of your body. Oxygen is what your cells need to produce energy.
Without adequate levels of B12, the body cannot produce enough healthy red blood cells, leading to a condition called anemia.
This can make you feel constantly exhausted, even after getting enough sleep. You may also feel weak, short of breath or find that everyday tasks feel harder to do than they generally are.
If the fatigue feels persistent and does not improve with rest, it is important to seek a consultation with a doctor.
2. Tingling or Numbness in the Hands and Feet
Vitamin B12 is also essential for maintaining the myelin sheath, a protective covering around your nerves. You can think of it like the protective plastic that we see around electrical wires. It helps nerve signals travel quickly and correctly between your brain and the rest of your body.
When B12 levels are too low, this protective layer can become damaged and subsequently lead to nerve signals slowing down or misfiring. This may lead you to feel pins and needles, tingling or numbness in your hands and feet. Some people also experience burning sensations or difficulty with balance.
At first, it may seem minor, such as your foot ‘falling asleep’. But if these sensations happen often or without a clear reason, they should not be ignored. Long-term B12 deficiency can cause permanent nerve damage, which is why early medical consultations are important.
3. Brain Fog, Memory Problems or Mood Changes
Your brain also depends on vitamin B12. It helps your body produce neurotransmitters, which are chemicals that allow brain cells to communicate with each other. These chemicals influence memory, focus and mood.
When B12 levels are low, communication between brain cells may not work as efficiently. You may notice difficulty concentrating, forgetfulness or a feeling of mental fog. Some people feel more irritable, anxious or unusually low in mood.
As these symptoms are common during stressful times, they are often dismissed. However, if you feel mentally different from your usual self for a long period, it is important to investigate the cause.
Why Does B12 Deficiency Happen?
Vitamin B12 is mainly found in animal-based foods such as meat, fish, eggs and dairy products. People who follow vegetarian or vegan diets may need fortified foods or supplements to get enough.
Absorption is also a key factor. Vitamin B12 needs a special protein in the stomach called intrinsic factor to be absorbed properly. Certain medical conditions, medications, or aging can reduce absorption. This means that even if someone eats enough B12, their body may not absorb it efficiently.
When to See a Doctor
If you experience ongoing fatigue, tingling sensations or noticeable changes in memory or mood, consult a healthcare professional. A simple blood test can measure your B12 levels.
The good news is that Vitamin B12 deficiency is usually treatable. Treatment may include dietary changes, oral supplements or, in more severe cases, injections. When identified early, most people recover well.
The Bottom Line
Vitamin B12 supports your blood, nerves and brain. A deficiency can quietly affect your energy, sensation and thinking over time.
Pay attention to persistent changes in your body. If something feels consistently wrong, it is important to seek medical advice. Early detection can prevent long-term complications and help restore your health.
© 2024 Bennett, Coleman & Company Limited

