- Health Conditions A-Z
- Health & Wellness
- Nutrition
- Fitness
- Health News
- Ayurveda
- Videos
- Medicine A-Z
- Parenting
- Web Stories
World Brain Day: Can Your Mind Break The Body? How Chronic Anxiety Might Be Fueling Neurodegeneration

Credits: Canva
We often think of anxiety as an emotional or mental struggle- a racing heart before a big meeting, a persistent knot in the stomach, the endless loop of worst-case scenarios playing out in our minds but what if anxiety was doing more than just weighing on your mood? What if, over time, it was actually damaging your brain?
Chronic anxiety, if left untreated, doesn't just affect how you feel. Emerging neuroscience suggests it can also cause structural and functional damage to the brain, potentially speeding up the onset of neurodegenerative diseases like Alzheimer’s and Parkinson’s.
According to Dr. Prajwal Rao, DM Neurology and Head of the Department of Neurology at Dr. D.Y. Patil Medical College, Hospital and Research Center in Pune, “We’re starting to view anxiety not just as a symptom of stress or a psychiatric diagnosis, but as a biological driver that may influence long-term brain health.” That insight is leading researchers and clinicians to reevaluate how they screen, diagnose, and treat anxiety—especially in older adults.
This is more than a mental health story. It’s a wake-up call about how your mind and body are more interconnected than we ever realized—and why ignoring chronic anxiety could have irreversible consequences.
How Does The Brain React on Chronic Stress?
At the core of this mind-body connection lies the body’s stress response system, known as the hypothalamic-pituitary-adrenal (HPA) axis. This system is built for short-term survival, it floods your body with cortisol to help you react in fight-or-flight situations. But when anxiety is chronic, the HPA axis stays overactivated, keeping cortisol levels high for too long.
Dr. Rao explains, “Sustained cortisol exposure has neurotoxic effects. It weakens the hippocampus, the area of the brain responsible for memory and learning. Over time, this can lead to measurable cognitive decline.”
This means that someone living with long-term anxiety isn’t just emotionally fatigued—they may also be more vulnerable to diseases involving memory loss, such as Alzheimer’s.
Recent imaging studies support what neurologists like Dr. Rao have long suspected. People with generalized anxiety disorder (GAD) frequently show reduced hippocampal volume, a condition also observed in patients with early-stage Alzheimer’s. These findings suggest a troubling overlap between anxiety-related brain changes and those seen in neurodegenerative diseases.
But the damage doesn’t stop there. Chronic anxiety can also trigger neuroinflammation, the process by which the brain’s immune system begins attacking its own cells. Neuroinflammation has been implicated in a wide range of neurological diseases—from Parkinson’s to ALS—raising the stakes for early anxiety treatment.
Can Poor Sleep Be The Silent Aggravator of Neurodegeneration?
Another hidden piece of the puzzle is sleep. The brain’s self-cleaning system, known as the glymphatic system, becomes active primarily during deep sleep. It flushes out toxic proteins like beta-amyloid, the same proteins that clump together to form plaques in Alzheimer’s patients.
Chronic anxiety often disrupts sleep, reducing both its quality and duration. “When deep sleep is compromised, the brain loses its opportunity to detoxify itself,” says Dr. Rao. “This may allow harmful proteins to build up, accelerating cognitive decline.”
What Role Genetics Play For Increased Vulnerability?
While not everyone with anxiety will develop a neurodegenerative disease, some individuals may be more biologically susceptible than others. Genetics appears to play a role—especially in people who have both anxiety-prone temperaments and gene variants that affect stress response and neural resilience.
These individuals may have a double disadvantage, they’re more likely to experience anxiety, and their brains may be less equipped to handle the long-term effects of that stress. Early screening and intervention in such high-risk populations could be crucial in delaying or preventing serious brain-related illnesses.
Is Anxiety in Older Adults An Overlooked Danger?
One of the most concerning aspects of this connection is how frequently anxiety is underdiagnosed in older adults. Symptoms like restlessness, irritability or sleep problems are often written off as “normal aging” especially when there’s no obvious cause.
This is a missed opportunity, says Dr. Rao. “Anxiety in the elderly shouldn’t be dismissed—it may be a modifiable risk factor for neurodegeneration. By treating it proactively, we’re not only improving emotional wellbeing but potentially preserving cognitive function.”
What This Means for People With Anxiety?
Treating anxiety isn’t just about feeling better in the moment—it could be a long-term investment in your brain health. Cognitive-behavioral therapy (CBT), mindfulness-based stress reduction, physical exercise, and even certain medications can all help manage anxiety. But more importantly, they may help protect the brain from premature decline.
“It’s time we stop thinking of anxiety as just an emotional burden,” Dr. Rao says. “The brain and body are intimately connected. Supporting mental health is supporting brain health—and ultimately, whole-body health.”
As neuroscience continues to evolve, one truth is becoming clear: our emotional health is not separate from our physical wellbeing. Chronic anxiety, if left unchecked, may do more than drain your energy or mood. It may slowly erode the very structure of your brain.
The next time you’re tempted to push anxiety to the side or power through it, remember this—the mind can break the body. But with the right care, attention, and treatment, it can also be the first line of defense in protecting your most vital organ: your brain.
Millions At Risk As Chikungunya Virus Threatens Global Health, Warns WHO; Can A Mosquito Bite In Monsoon Trigger Severe Symptoms?

Credits: Canva
The World Health Organization (WHO) has issued a grim warning about a large-scale outbreak of the chikungunya virus is gaining speed—and the initial symptoms are ominously reminiscent. In comparison to the catastrophic 2004–2005 epidemic that started in the Indian Ocean region and later reached hundreds of thousands of people all over the world, WHO experts are calling on governments to take action before the same repeats itself.
Dr. Diana Rojas Alvarez, WHO’s technical lead for chikungunya, told reporters in Geneva that the virus is now being detected in 119 countries, putting 5.6 billion people at risk. The warning is not hypothetical. Already in 2025, regions like Réunion, Mayotte, and Mauritius have seen major outbreaks. In Réunion alone, nearly one-third of the population is estimated to have been infected.
What’s different this time is the potential for global scale and speed, thanks to interconnected travel, shifting climates, and growing populations of virus-carrying mosquitoes. And while the name “chikungunya” may not be widely known outside scientific circles, its impact can be life-altering—if not deadly.
Why Is Chikungunya Dangerous?
Chikungunya is a mosquito-borne viral illness caused by the chikungunya virus (CHIKV), typically transmitted by Aedes aegypti and Aedes albopictus, the same mosquitoes that spread dengue and Zika viruses. These insects bite mostly during the daytime with peak activity in the morning and late afternoon.
The virus causes sudden onset of high fever, intense joint pain, headaches, rash, and muscle aches. The joint pain can become so severe that it bends sufferers into contorted postures—an origin of the disease’s name, which comes from a Makonde word meaning “that which bends up.”
While the majority of patients recover within a week, some symptoms—particularly joint pain—can persist for months or even years. In rare cases, chikungunya can cause neurological, cardiac or ophthalmic complications. Newborns, older adults and those with chronic medical conditions face a higher risk of severe disease or death.
Although the case fatality rate remains under 1%, WHO warns that large-scale outbreaks could mean thousands of deaths, especially in countries with under-resourced health systems.
According to WHO, the trajectory of the current outbreaks strangely mirrors that of the 2004–2005 epidemic. It began in small island nations before spreading across the Indian Ocean and into Asia, Africa and beyond. Today, similar trends are being observed with:
- Réunion has reported over 51,000 cases as of May 2025
- Mayotte, another French territory, has recorded 560 cases, pushing it into an epidemic phase
- Madagascar, Somalia, and Kenya are now reporting new clusters
- South Asia is experiencing epidemic-level transmission
- France has confirmed 30 local cases across 12 regions, with the largest cluster in Salon-de-Provence
- Italy reported its first locally acquired case since 2017 in Piacenza
Even countries like Portugal have reported dengue and chikungunya cases in 2025, highlighting how climate change and international travel are making vector-borne illnesses harder to contain.
Dr. Rojas Alvarez emphasized, “We are raising the alarm early so countries can prepare early—strengthening detection, prevention, and response systems is key.”
Why Europe and the US Should Pay Attention?
For decades, chikungunya was seen as a “tropical” disease, limited to warmer parts of Asia, Africa, and the Americas.
The Aedes albopictus, or tiger mosquito, is expanding its range northward due to warming temperatures and human-driven climate change. These mosquitoes have already become established in parts of southern Europe and even the southeastern United States. And with imported cases from travelers on the rise, localized outbreaks are becoming increasingly plausible.
The European Centre for Disease Prevention and Control (ECDC) recently launched updated guidance on mosquito-borne illnesses and emphasized the growing risk of local transmission. In addition to chikungunya, local dengue cases have been reported in Italy, France and Portugal in 2025.
How Can People Protect Themselves?
There’s no antiviral treatment for chikungunya, and supportive care—hydration, rest, and pain relief—is the mainstay of treatment. That makes prevention the most powerful tool. The WHO and ECDC recommend the following steps:
- Use mosquito repellents with DEET or picaridin on skin and clothing
- Wear long sleeves and pants, especially during mosquito-active hours
- Install screens on windows and doors, and use insecticide-treated mosquito nets when sleeping
- Empty standing water from containers like buckets, pots, and old tires, where mosquitoes lay eggs
- Avoid outdoor activity during early morning and late afternoon, especially in outbreak zones
Has Vaccine Become The New Line of Defense?
In a significant step, UK has approved a chikungunya vaccine which contains a weakened version of the virus that trains the immune system to produce antibodies. The vaccine is prescription-only and is currently recommended for people traveling to high-risk areas. However, it is not without limitations. The Commission on Human Medicines has advised caution in people aged 65 and older, pending further evaluation.
Until now, all we had were repellents and mosquito nets. With this vaccine, people who travel frequently or live in endemic areas now have another layer of protection. Still, experts advise travelers to assess their personal risk. If you're taking a one-off trip to France, your risk is low but if you're planning repeated travel to areas with outbreaks, vaccination may be worthwhile.
Does Climate Change Affect Incidence Rate?
Chikungunya and other mosquito-borne diseases are moving into new regions and our global health systems are scrambling to keep up. The convergence of climate change, urbanization, and international mobility is creating the perfect storm for diseases like chikungunya, dengue, and Zika to flourish.
As WHO warns, the time to act is now. That means not only educating the public and travelers but also investing in surveillance, vector control, and vaccine distribution especially in lower-income countries where health infrastructure is fragile. In 2005, the world was caught off guard and in 2025, we don’t have that excuse.
Gluten Intolerance Could All Be In Your Head - Study Finds Psychological Link

(Credit-Canva)
Food intolerances are much more common than we realize. Things like gluten, lactose, or caffeine intolerances are some of the common food intolerances. According to the Cleveland Clinic about 6% of the US population is gluten intolerant, but did you know your gluten intolerance could be psychological more than a physical problem?
Some people who believe they have gluten intolerance may actually be experiencing symptoms due to their beliefs, rather than the gluten itself. A recent small study published in The Lancet Gastroenterology and Hepatology, suggests that for some with irritable bowel syndrome (IBS), their mind might be playing a trick on them.
How Psychology Affects Gluten Allergy
In the recent experiment, individuals diagnosed with IBS who thought they were sensitive to gluten reported feeling worse after eating a cereal bar, even when the bar contained no gluten or wheat. Their symptoms were similar whether they ate a gluten-free bar, a gluten-containing bar, or a whole wheat bar. This suggests that what people expect or believe about food, rather than the ingredients themselves, could be causing their digestive problems.
Understanding the "Nocebo Effect"
This phenomenon is known as the "nocebo effect," which is the opposite of the placebo effect. While a placebo makes you feel better because you expect to, the nocebo effect means that negative expectations can trigger real physical symptoms.
A senior researcher in the study explained that not everyone who believes they react to gluten truly does. While some people genuinely have a sensitivity, for many others, their conviction that gluten is harmful is what drives their symptoms and leads them to avoid gluten-containing foods.
Gluten: What It Is and Why It Matters
Gluten is a type of protein found in grains such as wheat, barley, and rye. For some people, eating gluten can genuinely cause problems with their digestion. This happens if they are allergic to the protein or if their body's defense system (immune system) reacts to it in a way that harms their gut. However, the recent study suggests that for many people who experience IBS symptoms, gluten might not always be the real cause.
Role of Social Media and Control
Researchers think that websites and social media platforms might be making people believe that gluten is bad for them, even when it's not the actual reason for their IBS symptoms. All the negative comments about gluten online can really influence what others think.
Also, some people with IBS might feel that by avoiding gluten, they are taking charge of their health, especially if they usually feel helpless about their condition. Interestingly, even after the study participants learned which food bars actually caused their symptoms, many of them didn't change what they believed or how they ate.
Beyond Dietary Restrictions
This suggests that simply telling patients, "Gluten isn't the problem," might not be enough. Instead, getting help like therapy or coaching could be necessary to help these individuals change their negative ideas about gluten.
Experts believe that helping these patients better means more than just giving them facts. Many could benefit from mental health support and advice to help them see gluten and wheat as harmless again, and to safely add these foods back into their diet.
More studies involving larger groups of people are needed to confirm these findings. We also need to understand exactly why a person's beliefs about gluten can cause real IBS symptoms in some cases.
Medical Memoir: Measles- The Unfinished Fight Against One Of The World’s Most Contagious Diseases
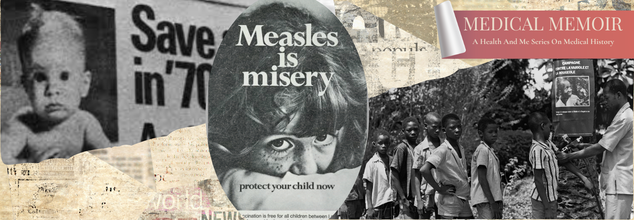
(Credit-WHO, Science Museum Group Collection)
'Medical Memoir' is a Health & Me series that delves into some of the most intriguing medical histories and unveils how medical innovations have evolved over time. Here, we trace the early stages of all things health, whether a vaccine, a treatment, a pill, or a cure.
Maggie was diagnosed with Leukemia at the age of 2.5-year-old, fighting cancer at a young age, she survived after another two and half years of treatment, but it left her in a very vulnerable state. Her immune system took a big hit, even a common cold could be dangerous for her.
What followed was Maggie’s parents' great efforts to ensure their child gets the best childhood, while making sure she stays safe. But no matter how safe you are or how much you try to keep your loved ones safe, things do not go as planned. Despite their efforts, during a routine visit to her oncologist, Maggie's parents were contacted about a measles case that was known to be in the clinic at the same time Maggie was. Every rash, cold or cough after that seemed like their nightmare come true, however, Maggie was lucky this time because she wasn’t infected.
This is not just a story, but the reality of Dr. Tim Jack, who spoke to the Vaccinate Your Family initiative, urging people not just to vaccinate to take care of their children, but also to ensure the safety of everyone around them. But what significance does this story have for our health? What do we need to be aware of measles?
A household name among diseases, measles, is considered to be one of the world’s most contagious diseases. Causing the deaths of millions, the disease impacts the respiratory tract and then slowly spreads throughout the body. Vaccination was the reason why we were able to control the disease in the 1960s, before which the estimated death each year was said to be 2.6 million death each year, according to the World Health Organization (WHO).
How Old Is Measles?
WHO states that the records of the disease can be traced back to the 9th century by a Persian doctor named Abū Bakr Muhammad Zakariyyā Rāzī. It became more common around the world starting in the 16th century as people traveled more. In 1757, a Scottish doctor named Francis Home discovered that measles was caused by a germ. He showed this by taking blood from sick people and giving the disease to healthy individuals.Places that had never seen the measles virus before were hit very hard. Outbreaks caused a lot of sickness and death in isolated communities, like the Faroe Islands in 1846, Hawai'i in 1848, Fiji in 1875, and Rotuma in 1911.
Root Cause Of Epidemics And Mass Death
Before vaccines, measles was always present around the world, causing epidemics. In richer countries, better healthcare and nutrition meant fewer people died from measles by the 20th century. While antibiotics couldn't fight the virus itself, they could help with complications like bacterial pneumonia. Still, common problems like ear infections, croup, diarrhea, and pneumonia led to thousands of hospital stays each year. A more serious complication, encephalitis (swelling of the brain), could cause brain damage, loss of hearing or sight, or even death.
Globally, the death rates remained very high, with about 30 million cases and over 2 million deaths every year.
The First Measles Vaccine
In 1954, a measles outbreak at a boarding school near Boston gave doctors a chance to try and find the measles virus. They took samples from sick students. A doctor named Thomas Peebles successfully grew the virus from a sample taken from an 11-year-old boy named David Edmonston. This success allowed doctors to create the very first vaccine against measles.
John Franklin Enders, who was Peebles's boss and is often called "the father of modern vaccines," developed the measles vaccine from a specific strain of the virus called 'Edmonston-B', named after David. This strain is still used today as the basis for most measles vaccines.
Enders and his team tested the vaccine on small groups of children from 1958 to 1960. After that, they started larger trials with thousands of children in New York City and Nigeria. In 1961, the vaccine was declared 100% effective, and the first measles vaccine was approved for public use in 1963.
Global Vaccination Efforts Begin
Starting in the 1960s, individual countries began large-scale vaccination programs against measles. The first international measles vaccination efforts began in Africa in 1966. The World Health Organization (WHO) worked with governments in over 20 newly independent African countries, along with other organizations, to give vaccinations. Their goal was to control measles and also get rid of smallpox.
Despite challenges, like keeping the heat-sensitive vaccine cold during transport and storage, these campaigns showed that vaccination worked against measles. By May 1967, The Gambia became the first country where the measles virus stopped spreading.
In 1968, Dr. Maurice Hilleman, a key figure in vaccine development, created an improved measles vaccine. He weakened the virus by passing it through chick embryo cells 40 times. This resulted in a vaccine that caused fewer severe side effects. This weaker version, known as the Edmonston-Enders strain, led to some of the strains still used in measles vaccines today.
In 1971, Hilleman combined the recently developed vaccines for measles, mumps, and rubella into a single shot called the MMR vaccine. In 2005, the chickenpox (varicella) vaccine was added to create the MMRV vaccine. Standalone measles vaccines are still available in many countries.
Worldwide Vaccination and Challenges
In 1974, measles was one of the first diseases targeted by the WHO when they started a program to expand vaccination efforts globally. Widespread childhood vaccination has dramatically reduced measles cases worldwide. WHO now suggests vaccinating babies at 9 months in areas where measles is common, and at 12–15 months in other areas. A second dose is recommended for all children, which is very important because about 15% of children don't get full protection from just one dose.
Why High Vaccination Rates are Crucial?
Because measles spreads so easily, a very high percentage of people need to be immune (at least 95%) to prevent large outbreaks. If vaccination rates drop too low, outbreaks can happen again when the disease is brought back into a community.
Besides the suffering measles causes, controlling outbreaks is expensive and takes resources away from other healthcare services. Measles deaths still occur in many countries, especially where vaccination programs have gaps. For example, in the Democratic Republic of the Congo, 7,800 people died from measles during an outbreak between 2018 and 2020, compared to 2,299 deaths from Ebola in the same period.
Eradication Efforts and Setbacks
The Americas region was declared free of endemic measles in 2016—the first WHO region to achieve this. However, this status was lost two years later due to a measles outbreak. This outbreak started because of a crisis in one country that led to gaps in vaccination and slow response. The virus then spread to neighboring countries, where it was eventually controlled.
To address these issues, the Pan American Health Organization (PAHO) has been training countries on how to quickly respond to prevent measles and rubella from spreading, improving disease tracking, and launching new, high-quality follow-up vaccination campaigns.
Between 2000 and 2023, measles vaccination prevented over 60 million deaths worldwide. However, despite having a safe and affordable vaccine, global measles deaths continued to rise before the COVID-19 pandemic. In 2019, there were over 207,000 measles deaths globally, which was the highest number of reported cases in 23 years.
Is Measles Still A Cause Of Concern?
According to Harvard Health as of July 2025, there have been 1,288 confirmed measles cases across 38 states in the US, primarily among children. This is the highest number of cases since 2000, the year measles was declared eliminated in the country.
This rise in cases is mainly because fewer people are getting vaccinated. Across the country, measles vaccination rates for school kids dropped from 95% in 2019 to 92% in 2023. In some areas where outbreaks are happening, like parts of west Texas, the vaccination rate is as low as 82%. This leaves many people unprotected. A big reason for the current cases is that 96% of recent infections were in people who weren't vaccinated or hadn't completed their shots.
As the history shows, measles outbreaks can be stopped. The MMR vaccine (Measles, Mumps, Rubella) is very effective, with two doses providing 97% protection, and it's very safe. Side effects are usually mild, like a sore arm or low fever. The false idea that vaccines cause autism has been proven wrong, but this misinformation has made some people hesitant to get vaccinated.
As a responsible citizen, one must ensure they keep in touch with healthcare professionals and keep the safety of their loved ones as well as everybody else around them.
© 2024 Bennett, Coleman & Company Limited

