- Health Conditions A-Z
- Health & Wellness
- Nutrition
- Fitness
- Health News
- Ayurveda
- Videos
- Medicine A-Z
- Parenting
- Web Stories
World IVF Day: What Makes The IVF Journey So Hard On The Mind?

In vitro fertilisation (IVF) is not just about science, syringes and success rates. What lies behind the walls of fertility clinics is a deeply personal journey filled with hope, heartbreak and resilience, making it more than just a medical procedure. Beyond the social taboos, infertility brings huge stress to the patients. And while IVF offers hope, it does not come easy. It is a rollercoaster ride that patients experience as they take on the road to this procedure; highs and lows can take a severe mental toll on them.
However, for those unversed, infertility has been classified by the World Health Organisation as a disease like diabetes or hypertension; the social taboo around it still persists. Over the years, advancements in reproductive science have made IVF treatments more patient-friendly and significantly improved outcomes. Yet, the focus often leans heavily on science, expertise and clinic proficiency, while the mental and emotional toll on the couple is overlooked.
For many, the psychological impact of IVF can match that of the death of a family member or going through a divorce. Although many people find IVF very stressful, every patient experiences it differently. Personalities and life experiences play a big role in determining how one handles the process and what part of IVF they find most difficult.
Why Is IVF So Emotionally Draining?
We ask an expert to break down several key factors that contribute to the immense stress IVF brings:
- Uncertainty of Outcomes
- Physical Strain
- Societal Pressure
- Guilt and Shame
- Depression After Failed Attempts
- Relationship Strain
Learning to Cope with Support Systems That Help
There is light at the end of the tunnel, and as Dr Saple says, there are several strategies that can help couples better cope with the IVF process.
- Psychological Counselling
- Support Groups
- Mind–Body Practices
Setting Realistic Expectations
“IVF may take more than one cycle to succeed,” she explains. Being mentally prepared for the outcome, while knowing you have done your best, helps couples accept results with resilience.
It is Okay to Ask for Help
As Dr Saple reminds us, mental and emotional health are as important as physical health during IVF. Prioritising emotional wellbeing not only makes the journey more bearable but can also improve the overall outcome. “Seeking help is a sign of strength, not weakness,” she says.
Why Does Your Face Start Tingling Mid-Bleach? We Find Out

The lazy ones know that facial bleach is one beauty product that comes in handy at any point in time. Whether it was for that last-minute party glow-up or to hide a sudden tan line, facial bleach has long been a last-minute resort in Indian homes. But what really happens when you apply that potent cream on your skin and wait for its effect? We dug in to find out exactly what is going on when your face starts tingling mid-bleach.
What is facial bleach?
Facial bleach usually contains hydrogen peroxide as the main ingredient. This acts as a lightening agent, breaking down melanin, the pigment responsible for skin colour. When you apply bleach, you are not removing hair or tanning; you are just lightening it to make it blend in with your skin.
What is happening under the surface?
When you apply bleach to your skin, it sets off a chain reaction. The hydrogen peroxide oxidises, which in simple terms means it reacts with the pigment and hair proteins, breaking down melanin and making everything lighter in colour. Your facial hair goes blonde, and your skin tone appears brighter, not because it has suddenly become radiant, but because there is less visual contrast.
It comes with side effects
If you have ever felt your face heat up or sting while bleaching, you have experienced a minor chemical reaction. Bleach is harsh. It strips the skin’s protective barrier ever so slightly, which is why your skin might feel sensitive, look a bit red, or feel tight afterwards.
Sensitive skin types should deal with it very carefully. Facial bleach can cause inflammation, itchiness, or even mild burns if left on too long or applied too often. And those with active acne, eczema, or any skin condition should steer clear altogether.
Can it damage your skin in the long run?
In moderation, bleaching every now and then might not wreak havoc, especially if you are using a reputable brand and following instructions to the dot. But using it too frequently is when trouble begins. Long-term, overuse can cause skin thinning, sensitivity to sunlight, and uneven pigmentation.
Also, your skin does not get used to bleach. It tolerates it up to a point and then acts up. You might suddenly develop a sensitivity you never had before.
Should you bleach at all?
Bleach has its moment. If you are prepping for a function, want that one-off glow, or just feel like softening the appearance of facial hair, go ahead; just be smart about it. Patch test always. Stick to the recommended time. Do not pile it on like it is moisturiser. And do not expose your skin to the sun immediately.
Use facial bleach sparingly, respect your skin, and be okay with skipping it altogether if your face is already protesting. Because no glow-up is worth a full-blown skin tantrum.
BRCA Screening Before IVF: A Smart Safeguard or Ethical Overreach?

(Credit-Canva)
Recently, BRCA testing has garnered considerable attention, especially in the realm of reproductive medicine. BRCA1 and BRCA2 mutations are known to significantly increase the risk of breast and ovarian cancers. But as we begin considering their routine inclusion in IVF workups, we must ask: Are we proactively protecting future generations, or are we crossing into ethically uncertain territory?
In India, regulatory guidelines limit the number of donations from a donor to only a single recipient, placing significant constraints on donor selection. Moreover, potential genetic risks are already evaluated during donor screening through a detailed family and medical history. Sperm banks are careful to exclude donors with a known history of hereditary diseases that could impact the offspring. In addition, donors undergo stringent infectious disease screening, including sexually transmitted diseases like HIV, hepatitis B and C, and syphilis, to safeguard recipient health. These processes significantly mitigate both genetic and health-related risks.
This is not to undermine the value of BRCA or other genetic testing when clinically indicated. BRCA testing should be offered in IVF when there is a relevant personal or family history of cancers or where BRCA genes have been detected in the family. Couples who have experienced repeated miscarriages or have had a previous pregnancy loss where a genetic abnormality was found may benefit from more comprehensive genetic testing.
For women above the age of 35, another layer of screening becomes important: preimplantation genetic testing for aneuploidy (PGT-A). This is not about hereditary mutations but chromosomal abnormalities, which are more common as maternal age advances and lead to conditions like Down’s Syndrome in the child or recurrent miscarriages and IVF failures. PGT-A screens the embryos ensure that only chromosomally normal embryos are transferred into the uterus thus improving IVF success rates in older women.
Genetic screening plays a valuable role in safeguarding the health of future generations, but its use must be balanced with clinical relevance and ethical responsibility. The patients need extensive counselling on the procedure as it is invasive testing where afew cells are removed from the embryo and tested. In a small percentage because of mosaicism in embryo, there are also false positive reports (where abnormality is detected when none exists) and false negative reports (where abnormality exists but the report states a normal embryo). Patients must also be made aware of alternative methods of testing the child during pregnancy like NIPT (non invasive prenatal testing) and level 2 ultrasound during pregnancy to help them to take an informed decision.
However, incorporating BRCA testing or any advanced genetic screening into the routine workup for all IVF patients can significantly increase the financial burden of an already expensive procedure. While such tests are undoubtedly important in certain high-risk cases, they should be recommended judiciously, based on personal or family history, recurrent pregnancy loss or IVF failures, or previously identified genetic abnormalities. A targeted, case-by-case approach remains the most ethical and effective path forward in reproductive care.
Diagnostic Anomaly: This Man’s Brain Began Bleeding After A Regular Dental Checkup
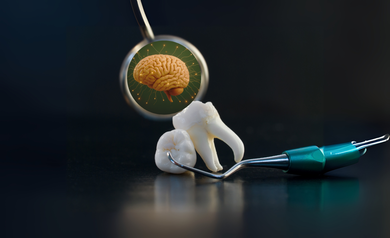
Credits: Canva
'Diagnostic Anomaly' is a Health And Me Series, where we dive deep into some of the rarest of rare diseases. Here, we trace such diseases and what causes them. We also try to bring case studies around the same.
A routine dentist appointment turned into a medical emergency for a man in his late 60s living in Australia. Just 30 minutes after having two teeth extracted, he began experiencing sudden and alarming symptoms — dizziness, vomiting, and a bizarre distortion in his vision, where the world appeared rotated 90 degrees counterclockwise.
These were not trivial side effects of anesthesia or stress. The symptoms were pointing to something much worse. When he came to the emergency room, physicians observed strange signs: abnormal eye movement to the left and a tendency to fall to the right when walking. A brain scan validated their suspicion he was having an intracerebral hemorrhage (ICH), a potentially fatal form of stroke due to bleeding in the brain.
Intracerebral hemorrhage constitutes 10–15% of all strokes and entails a ruptured vessel bleeding into the brain tissue. Ischemic strokes caused by obstructions do not need such immediate intervention, while ICH needs to be urgently treated to stop bleeding, reduce brain pressure, and avoid irreversible neurological injury.
In this patient, the bleeding was in the lower-left side of his brain — a region that affects balance, coordination, and vision. His health care team reacted quickly to treat the hemorrhage, decrease his blood pressure, and relieve intracranial pressure. Thankfully, after receiving immediate treatment, he was stabilized and released with medication to regulate his blood pressure.
Three months after that, he made a dramatic recovery. His eyesight was back to normal, and his balance also considerably improved. To prevent future strokes over the long term, he was put on aspirin, which prevents narrowing of the blood vessels in the brain by keeping the blood thin.
Although clinically managing the case was according to typical stroke procedure, what makes this case uncommon is the suspected etiology: a simple dental treatment.
The man’s symptoms began just half an hour after his tooth extraction. Medical literature contains a few rare reports of individuals experiencing ICH following dental procedures, possibly due to sharp spikes in blood pressure triggered by pain, anxiety, or physiological stress. In this case, the working theory is that the dental procedure, coupled with an undiagnosed underlying condition, created the perfect storm for a stroke.
What Is White Matter Disease?
As the medical staff delved deeper into his background, they discovered further hints. Only six weeks earlier, the man had received neurological tests for potential Parkinson's disease. Scans at the time had already indicated signs of white matter disease — abnormalities in the network of wiring in the brain, which can cause thought to be slower, lead to loss of balance, and predispose to stroke and dementia.
White matter disease targets the brain's "communication highways," the nerve fibers (axons) that carry signals between different areas of the brain and spinal cord. The fibers need a continuous supply of oxygen and nutrients. When blood flow is slowed — because of age, high blood pressure, or damaged vessels — the white matter breaks down, creating lesions that are seen on MRI scans.
Symptoms of white matter disease may range from memory loss, difficulty with coordination, sluggish movement, mood changes, and even urinary incontinence. The symptoms are worse if the damage is more extensive.
But the story didn't end there. Genetic studies of the man revealed he had an uncommon mutation associated with CADASIL-Cerebral Autosomal Dominant Arteriopathy with Subcortical Infarcts and Leukoencephalopathy. This inherited disorder is found in approximately 2 in 100,000 and causes blood vessel walls to thicken. This compromise results in reduced flow of blood into the brain and a drastically increased risk of stroke.
Other research implies ICH can be an complication of CADASIL, particularly when added on top of other influences such as high blood pressure or physical stress.
The course of events now makes sense. The patient's existing white matter disease already compromising brain connectivity and his unknown CADASIL mutation had left his brain's blood vessels particularly susceptible.
The dental removal, though apparently innocuous, perhaps triggered an increase in blood pressure due to stress or pain, a normal physiological reaction in a medical context. For a person with healthy blood vessels, this may not have resulted in anything. But with a brain containing constricted, weakened vessels, the pressure was sufficient to rupture a vessel resulting in an intracerebral hemorrhage.
How Small Triggers Meet Big Risks
This case is an admonition regarding the intricate intersection of genetics, chronic illness, and acute medical stressors. It also highlights the need for recognition and control of risk factors such as hypertension, white matter disease, and unrecognized genetic disorders that affect brain function.
For individuals with cardiovascular risk factors — for example, diabetes, hypertension, or high cholesterol — regular procedures, including dental treatment, might necessitate closer follow-up. Preventive interventions, such as brain imaging in individuals with neurological symptoms and a history of stroke or dementia in first-degree relatives, might detect conditions such as CADASIL before complications arise.
Can White Matter Disease Be Prevented?
Although some white matter changes are inevitable with aging, progression can be slowed down. Good management of heart and vascular health is key. Here's what doctors say:
- Keep blood pressure under control
- Manage high cholesterol and diabetes
- Stop smoking
- Be physically active
- Eat a heart-healthy diet (such as the Mediterranean diet)
Studies have established that lowering cardiovascular risk has been proven to reduce white matter lesions, thus reducing stroke, dementia, and physical disability risks later in life.
A routine dentist visit triggered a series of events that almost resulted in a catastrophe for this Australian man but with timely rescue and extensive diagnostic procedures, not only did he recover well, but the doctors also discovered a rare genetic disorder that might have been a future threat.
Occasionally, the body's reaction to less invasive procedures can expose deep-rooted problems. Paying attention to your body, reporting new symptoms, and being proactive about brain and heart health can be the difference-maker — particularly when the indicators are easy to miss.
© 2024 Bennett, Coleman & Company Limited

