- Health Conditions A-Z
- Health & Wellness
- Nutrition
- Fitness
- Health News
- Ayurveda
- Videos
- Medicine A-Z
- Parenting
What Is ‘Pleasanteeism’? The Workplace Trend That’s Quietly Harming Your Mental Health
Credits: Canva
Pleasanteeism, the pressure to appear cheerful and upbeat at work no matter what one is feeling inside, has become a growing concern in many workplaces. This constant expectation to keep a positive front often pushes employees to hide their real emotions, which can lead to mental fatigue, anxiety, and eventually burnout. Though not a new idea, the term ‘pleasanteeism’ has resurfaced as office workers once again discuss buzzwords like ‘quiet quitting,’ ‘coffee badging,’ and ‘office peacocking.’
What Is Pleasanteeism And How Is It Impacting Mental Health At Work?
According to Dr Chandni Tugnait, MD (A.M), Psychotherapist, Life Alchemist, Coach & Healer, and Founder & Director of Gateway of Healing, this problem has only worsened with the rise of hybrid work models. The need to look lively during video calls and the fading line between personal and professional life make it harder for employees to recover emotionally.
She explains to us that activities such as “forced fun” sessions or public praise for being positive can unintentionally discourage honesty and openness. “To address pleasanteeism, companies must create a space that values honesty and supports mental wellness,” says Dr Chandni.
A recent report by Lime also points to how pleasanteeism is hurting both mental health and workplace performance. This culture of putting on a “brave face” prevents people from having honest discussions about their struggles, keeping important mental health conversations out of reach.
Some of the key findings from the report include:
- 40% of employees say they feel less emotionally strong now than before the pandemic.
- 26% admit they find it difficult to manage work demands.
- 51% feel they must act cheerful around colleagues even when they are not.
- 44% believe their low emotional resilience affects how well they perform at work.
These figures highlight how important it is for organisations to build environments that encourage openness and emotional safety, which can benefit both well-being and productivity.
How Does Pleasanteeism Affect Mental Health In The Short And Long Term?
Short-term Effects
In the short term, pretending to be happy all the time can quickly drain one’s emotional energy, leading to emotional exhaustion. This leaves people feeling mentally tired and disconnected from their personal lives. Constantly trying to regulate expressions can also heighten anxiety, as employees become anxious about revealing how they truly feel. Over time, this stress often appears in physical forms, causing headaches, muscle tightness, and disturbed sleep, all of which further affect mental health.
Long-term Effects
Over a longer period, the effects deepen. Persistent emotional suppression can create an identity disconnect, where individuals lose sight of their real feelings and struggle to understand themselves. It can also cause chronic burnout, as constantly putting on a cheerful mask drains psychological energy, leading to detachment and low productivity. Relationships may begin to suffer too, since hiding emotions weakens genuine connections, leaving people feeling isolated and unsupported.
Professionally, pleasanteeism can contribute to career stagnation, as the effort spent maintaining appearances takes away from learning or growing in one’s field. Finally, it may lead to unhealthy coping habits, such as overeating or turning to alcohol to manage stress, which further worsens mental well-being.
Nipah Virus Symptoms Explained As Doctors Warn Up To 75% Fatality Risk
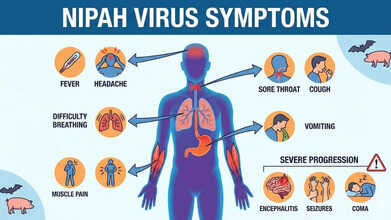
Credits: AI Generated
Health authorities have urged the public to stay alert to Nipah virus symptoms after doctors warned that up to 75 per cent of infected patients may not survive. The UK Health Security Agency (UKHSA) has classified Nipah as a “high priority pathogen” because of its severe fatality rate and the absence of any proven treatment.
In India, the federal health ministry has confirmed two cases in the eastern state of West Bengal. This has triggered large-scale containment measures, with local officials placing nearly 200 people who had contact with the infected individuals under quarantine.
Also Read: Vitamin D Supplements Under Scrutiny As It Fails Safety Test
In response, several Asian nations have stepped up airport checks and health surveillance for travellers arriving from India. Professor Paul Hunter, an infectious disease specialist at the University of East Anglia, said identifying Nipah cases at borders is challenging, as symptoms can take a long time to appear.
What Is Nipah Virus?
According to UKHSA, Nipah virus is a zoonotic infection, meaning it can pass from animals to humans. It can also spread through contaminated food or via direct human-to-human contact. The virus was first discovered in 1999 during an outbreak affecting pig farmers in Malaysia and Singapore.
Fruit bats, especially those belonging to the Pteropus species, are the virus’s natural carriers. Research shows that Nipah can also infect other animals, such as pigs, dogs, cats, goats, horses and sheep.
Nipah Virus Symptoms
UKHSA lists the following as common symptoms of Nipah virus infection:- Sudden onset of fever or general flu-like illness
- Development of pneumonia and other breathing-related problems
- Swelling or inflammation of the brain (encephalitis) or meningitis
Symptoms usually appear between four and 21 days after exposure, although longer incubation periods have occasionally been reported. More severe complications, including encephalitis or meningitis, can develop between three and 21 days after the initial illness begins.
Also Read: Nipah Virus Outbreak In India: All That You Need To Know About This Infection
Nipah Virus Symptoms Explained As Doctors Warn 75% Fatality Rate
UKHSA has cautioned that between 40 and 75 per cent of people infected with Nipah virus may die. Those who survive can experience long-term neurological effects, such as ongoing seizures or changes in behaviour and personality. In rare instances, the virus has been known to reactivate months or even years after the first infection.
Nipah Virus: Can You Prevent It From Spreading?
For people travelling to regions where Nipah is known to occur, prevention largely involves reducing exposure risks:
- avoid contact with bats, their habitats, and sick animals
- do not drink raw or partially fermented date palm sap; if consuming date palm juice, make sure it has been boiled
- wash all fruits well with clean water and peel them before eating; avoid fruits found on the ground or those that appear partly eaten by animals
- use protective clothing and gloves when handling sick animals or during slaughter and culling
- maintain good hand hygiene, especially after caring for or visiting ill individuals
- avoid close, unprotected contact with anyone infected with Nipah virus, including exposure to their blood or bodily fluids
Nipah Virus Symptoms Can Be Transmitted Easily?
Many Nipah infections have been linked to eating fruit or fruit-based products contaminated by the saliva, urine or droppings of infected fruit bats. Human-to-human transmission can also occur through close contact with an infected person or their bodily fluids, according to Mirror.
Such transmission has been documented in India and Bangladesh, with cases often involving family members or caregivers tending to infected patients. At present, there is no specific, proven treatment for Nipah virus infection, and no licensed vaccine is available to prevent it.
So far, no Nipah virus cases have been reported in the United States or the United Kingdom.
People Who Began Smoking Before 20 Face Higher Stroke Risk, Study Shows

Credits: Canva
Smoking has long been recognized as one of the most preventable causes of disease and early death worldwide. It plays a major role in heart attacks, strokes and several chronic illnesses. While public health messaging often focuses on how much a person smokes, new research suggests that when someone starts smoking may be just as important for long-term health.
A large nationwide study published in Scientific Reports analyzed health data from over nine million adults in South Korea. The findings were striking. People who began smoking before the age of 20 faced a significantly higher risk of stroke, heart attack and early death compared to those who started later, even if their total lifetime smoking exposure was similar.
Smoking Before 20: Why the age matters
Traditionally, doctors and researchers estimate smoking-related harm using pack-years, which combines the number of cigarettes smoked per day with the number of years a person has smoked. While this remains useful, the new study highlights an important gap. Two people with the same pack-years may not have the same health risks if one started smoking much earlier in life.
The researchers found that early starters had a much higher risk of stroke and heart attack than those who took up smoking after the age of 20. This suggests that the body may be especially vulnerable to tobacco damage during adolescence and early adulthood, making age of initiation an independent risk factor.
Smoking and stroke: what we already know
The link between smoking and stroke is well established. Long-term studies, including the famous Framingham Heart Study, have consistently shown that smokers are far more likely to experience a stroke than non-smokers. The risk increases with the number of cigarettes smoked and affects people across age groups.
Smoking damages blood vessels, speeds up plaque build-up in arteries, raises blood pressure and makes blood more likely to clot. All of these changes increase the chances of both ischaemic and haemorrhagic strokes. Younger adults who smoke are not protected simply because of their age, and in many cases, their relative risk is even higher.
Key findings from the Korean cohort
The study followed participants for nearly nine years using data from a mandatory national health screening programme. Researchers looked at stroke, heart attack, combined cardiovascular events and overall death rates.
Those who started smoking before 20 had about a 78 percent higher risk of stroke compared to non-smokers, especially when they also had high smoking exposure. Early starters also showed a much greater risk of heart attacks and combined cardiovascular events. Importantly, they had a higher risk of death from all causes, not just heart-related conditions. These patterns were consistent across men and women and across different metabolic health profiles.
Why early smoking causes greater harm
There are several reasons why smoking at a younger age may be more damaging. During adolescence, the heart, blood vessels and brain are still developing, which may make them more sensitive to toxins in tobacco smoke. Starting early is also linked to stronger nicotine dependence, making quitting harder and often leading to longer periods of smoking.
Early exposure may also trigger lasting inflammatory and metabolic changes in the body. These changes can increase stroke risk later in life, even when total cigarette exposure appears similar on paper.
What this means for public health
The findings send a clear message. Preventing smoking during adolescence could significantly reduce the future burden of stroke and heart disease. School-based education, strong warning messages and policies that limit youth access to tobacco remain critical.
Delaying smoking initiation, even by a few years, may have lifelong benefits. With cardiovascular diseases already among the leading causes of death globally, protecting young people from tobacco use is not just about avoiding addiction. It is about safeguarding their long-term health.
This Simple Tennis Ball Test Can Reveal Dementia Risk

(Credit-Canva)
A simple tennis ball might be able to tell you whether you have dementia or not. While it sounds strange, experts explain that the strength of your hands is a major clue for how well your mind is aging.
In a recent video, Neurologist Dr. Baibing Chen explains that your grip strength is a "window" into your cognitive health. To squeeze your hand, your brain must coordinate nerves, muscles, and blood flow all at once. When this system weakens, it often suggests that the brain’s "resilience" or ability to bounce back is also lower.
While weak hands don't cause dementia, they can be an early warning sign. In some conditions, like vascular dementia, physical changes like slowing down or dropping things often happen before memory loss even begins.
How To Do The Tennis Ball Test At Home?
You don't need expensive equipment to check your strength. You can use a standard tennis ball or a stress ball to track your progress:
Get Ready: Sit up straight with your feet flat on the floor and your arm stretched out in front of you.
Squeeze: Grip the ball as hard as you possibly can.
Hold: Try to keep that strong squeeze for 15 to 30 seconds.
Repeat: Do this three times with each hand and note if you feel tired or if your strength fades quickly.
What the Numbers Mean
Researchers have found that people in the bottom 20% of grip strength have a much higher risk of developing memory problems.
For example, a massive study of nearly 200,000 adults showed that as grip strength drops, the risk of dementia goes up by about 12% to 20%.
Specifically, if a man’s grip strength is below 22 kg or a woman’s is below 14 kg, doctors consider that a "red flag" for future cognitive decline. These numbers are helpful because they show changes in the body years before memory loss actually starts.
What If You Fail The Tennis Ball Dementia Test?
It is very important to remember that a weak grip is not a guarantee of dementia. Many factors, such as arthritis, old injuries, or general lack of exercise, can cause your hands to feel weak.
The goal of this test is not to scare you, but to encourage you to be proactive. If you feel like your hands are getting "tired" faster during daily chores or you are dropping items more often, mention it to your doctor. They can help determine if it is just a muscle issue or something that needs more investigation.
How Is Dementia Diagnosed?
Dementia is one of the most common cognitive conditions in the world. According to the World Health Organization, there were 57 million people living with dementia in 2021, many of whom never had any treatment for it.
Early detection of dementia is an important part of the treatment. While it may not completely cure the disease, it can slow down the progress to help people retain as much of their abilities as possible.
Finding out if someone has Alzheimer’s is not as simple as taking one single test. Doctors act like detectives, gathering many different clues to figure out what is happening in the brain. To make an accurate diagnosis, healthcare providers use a combination of different tools and tests:
Brain Scans
Doctors may use imaging tests like MRI, CT, or PET scans to look at the physical structure of the brain and check for any unusual changes.
Cognitive Tests
There may be cognitive tests that check your recall skills. These are mental puzzles or questions that check your memory, problem-solving skills, and how well you can perform daily tasks.
Lab Work
This can also include blood tests or checking "spinal fluid" to look for specific markers that show up in people with certain types of dementia.
Physical Exams
A neurologist may also check your balance, your senses, and your reflexes to see how well your nerves are working.
© 2024 Bennett, Coleman & Company Limited

