- Health Conditions A-Z
- Health & Wellness
- Nutrition
- Fitness
- Health News
- Ayurveda
- Videos
- Medicine A-Z
- Parenting
- Web Stories
Youtuber Shares How She Went Into A Coma 2 Weeks After Giving Birth: Can Complication During Childbirth Become Deadly?

(Credit-Mrkate/Instagram)
Childbirth and pregnancy are one of the most hardest things a human body can go through. Although things have gotten easier, in terms of care and ensuring the mother’s safety while giving birth, the small percentage of mortality looming overhead does not disappear. ‘But it’s just the pregnancy and childbirth that’s the tough part, right? Once you get past that you no longer have to worry about other complications.' But that is not entirely true either and facing this reality, the YouTube duo, Mr. Kate, shared their birth story.
You may know Mr. Kate from their YouTube channel, that has amassed over 3 million subscribers, sharing their life, stories and other fun challenges. In a recent video, they shared their birth story and the unexpected challenges they faced.
In the video, Kate Albrecht and Joey Zehr, welcomed their second baby together in a home birth. Their first child was born in 2019 in the hospital and Kate hoped for her second and last pregnancy she could experience a natural homebirth. In an interview with the People, she shared how she wanted to do a home birth because it sounded “really magical”, and since they chose to have their first birth at hospital, she thought for her second and last pregnancy, she was ready to challenge herself with a home birth.
How Do Home Births Work?
According to the National Health Services (NHS) when cosidering a home birth, one should be very careful and make sure they are making a well-informed choice. They explain that during a home birth, a community midwife, will come to look after you during the birth and a short while after the baby is born, they will assist you in different things along with making a birth plan suitable for the mother’s care.
Kate explained that she and Joey engaged in "dual care," seeing both a midwife and an OB-GYN to ensure a safe delivery. The birth of their daughter, Mars, was a success, and the baby was born en caul (still inside the amniotic sac), a rare and significant event.
Following the birth, Kate was prepared for a smoother recovery than her first. However, it was just 2 weeks after she gave birth after which a medical emergency arose.

Can Pregnancy Complications Occur Weeks After Giving Birth?
After giving birth, Kate felt exhausted and had severe headaches and a bad backache. When she went for her check-up, doctors told her these symptoms were normal for someone recovering from childbirth. However, two weeks after Mars was born, Kate suddenly collapsed at home. When her husband Joey found her, she was unconscious and having a seizure.
Joey called 911, and paramedics quickly figured out that Kate was suffering from eclampsia, a dangerous condition that can cause seizures. It's connected to preeclampsia, a blood pressure issue that can happen during pregnancy. In Kate's case, it happened after she gave birth, which is rare. Even though she had been perfectly healthy during her pregnancy and her tests for preeclampsia were negative, her body had developed the condition in the weeks after her baby was born.
Can Childbirth Complications Lead To Coma?
At the hospital, doctors put Kate in a medically induced coma to protect her brain. Scans showed she did not have any brain bleeding, which was a huge relief. However, they did find a blood clot in a vein near her kidney. This explained the terrible back pain she had been feeling.
After a few days, Kate was finally able to wake up from the coma. She had to stay in the hospital for a little while, but she was eventually sent home with medication to help prevent future blood clots.
Kate and Joey decided to share their story to help other parents. They learned that postpartum eclampsia can happen up to six weeks after a baby is born. They want everyone to know that even if you have a healthy pregnancy, you still need to be aware of the signs of this condition and get medical help for any unusual symptoms after giving birth.
Although the complications were scary, Kate and Joey are happy and thriving with the new addition to their family. Their fans and well-wishers commented supporting the couple and advocating how important postpartum care is.
Best Sleeping Position for Back Pain Relief: How To Wake Up Without Aches or Stiffness

(Credit-Canva)
Lower back pain is a very common problem, with a large majority of adults experiencing it at some point in their lives. While some morning stiffness is normal after being in one position for a while, if you feel pain that doesn't go away after you start moving, there might be a specific reason for it. It could be something as simple as your mattress, or it might be a sign of an underlying medical issue.
Have you ever woken up with a sore neck or a tingling arm? Your sleep position might be the reason. When you sleep, the goal is to keep your spine in a straight, natural line. Doing this reduces the strain on your neck and back, which can lead to a more pain-free and restful night.
Common Causes For Sleep Related Back Pain
According to the Sleep Foundation, if you wake up with back pain every morning, your sleep position may be to blame.
Your Mattress
An old or unsupportive mattress can contribute to back pain. If your mattress is more than five years old, it might be time for a new one. Studies have shown that people who replace their old mattresses often see a big improvement in their sleep and a reduction in back pain. In general, a medium-firm mattress is often recommended to help with lower back pain.
Lack of Movement
Staying in one position for a long time during sleep can lead to stiffness and tightness in your lower back. This is why morning stretches are often recommended to help get things moving again and relieve discomfort.
Muscle Strains or Soreness
If you wake up with pain after a tough workout or from lifting something heavy, you might have muscle soreness or a strain. The discomfort from a strain can feel more noticeable in the morning after your body has been still for several hours.
What Is The Best Sleeping Positions for a Pain-Free Night
According to Keck Medicine of USC,
On Your Back
Lying flat on your back is considered the best position for your spine. It keeps everything in a neutral position with the least amount of pressure. To make this position even better, place a pillow under your head or neck and another one under your knees to support the natural curve of your spine. However, if you are pregnant, it's best to avoid this position as it can reduce blood flow.
On Your Side
This is the second-best position for avoiding back and neck pain. It's especially helpful if you snore or have sleep apnea because it keeps your airways open. For proper alignment, try to sleep with your legs stretched out straight and a pillow tucked between your knees.
Positions to Be Careful With While Sleeping
The Fetal Position
Even though this is one of the most popular ways to sleep, curling up with your legs bent toward your chest can be tough on your back. It creates uneven pressure on your spine and can make your joints sore. If you prefer to sleep on your side, try to untuck your chin and straighten your body into a more relaxed position.
On Your Stomach
According to spine experts, sleeping on your stomach is the absolute worst position for your back. It flattens the natural curve of your spine and forces you to turn your neck to the side. This puts a lot of stress on your spine's muscles and joints, which can easily lead to pain in your neck and upper back.
What Doctors Thought Was A Sports Injury Turned Out To Be A Rare Form Of Cancer For This Teenager
(Credit - Megan Lallo/ Cleveland Clinic)
Like any other young boy, Evan Lallo from Kirtland, Ohio, was finding his footing in life. What were his hobbies, what kind of sports he likes etc. And it is a given that starting any sports meant hurting muscles, tiredness and random pangs of pain. However, it was not simple for Evan. Although he may not have wished for a sports injury, what he found was much worse.
Evan’s difficult journey began with something that seemed simple: a painful shoulder. As a 14-year-old athlete who loved basketball, football, and lacrosse, the pain he started feeling was initially diagnosed as a common sports injury. He went through treatment, but the pain kept getting worse, eventually becoming so severe he couldn't even hold a pencil.
This alarming change led his family to the emergency room in search of answers. An MRI revealed a shocking truth: a mass was growing on his neck. Evan was quickly sent to Cleveland Clinic Children's, where a team of specialists worked together to identify the rare tumor. They discovered it was a type of cancer called Ewing sarcoma, which was growing along his nerves and causing all the pain and loss of function in his arm.
What Is Ewing Sarcoma?
According to National Cancer Institute, Ewing sarcoma is a type of cancer that forms from certain cells in your body. It usually appears in your bones or the soft tissues around them, such as muscles, fat, and cartilage. This cancer is most common in teenagers and young adults, typically from their teens up to their mid-20s.
This cancer can develop in the bones of your arms, legs, feet, hands, chest, pelvis, spine, or skull. It can also form in the body’s soft tissues, which are the tissues that connect, support, and surround your other organs.
Following the life-changing diagnosis, Evan’s treatment began immediately and was incredibly challenging. Over the next seven months, he endured multiple rounds of grueling chemotherapy and radiation therapy. Evan’s mom, Megan, shared that they spent more than 70 nights in the hospital throughout the treatment.
What Are Symptoms of Rare Bone Cancer?
The symptoms of Ewing sarcoma can vary from person to person. They may look like a lump on the arms, legs, or chest. Some other signs to be aware of include:
- Bone pain that comes and goes, especially at night.
- Swelling around a bone that hurts when you touch it.
- A lump near the skin's surface that feels warm and soft.
- A fever that won't go away.
- A bone that breaks without an obvious injury.
- Feeling very tired and losing weight without trying, which can happen if the cancer spreads.
Does Bone Cancer Reduce Limb Functionality?
Even after the intensive chemotherapy and radiation shrank Evan’s tumor, he was still struggling with limited function in his arm because the cancer had caused nerve damage. This created a new challenge for his recovery. His team brought in a specialist, Dr. Megan Jack, a neurosurgeon who performs a rare procedure called a nerve transfer.
She explained that the surgery essentially takes a healthy nerve and reconnects it to the damaged one to restore movement. Evan’s successful surgery in May 2025 gave him a new sense of hope. Although his arm would take time to heal and require physical therapy, his doctors were already seeing signs of improvement.
A Brave New Beginning: Life After Cancer
By June 2025, Evan had reached the final milestone of his cancer journey. His scans showed no signs of cancer remaining. He celebrated this incredible victory by ringing the Bravery Bell, a moment filled with relief, pride, and gratitude.
With his cancer treatment behind him, Evan is now focused on the future. He is looking forward to going back to school full-time and, with continued healing, getting back to playing sports with his friends. Evan’s powerful message to others is simple: “Just keep going.” His journey is a true testament to his incredible resilience and the strength of his support system.
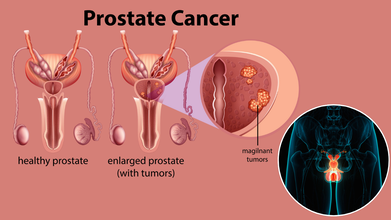
Prostate Cancer Rates Climb Again After A Decade Of Decline: 80% Of Americans Don’t Know Early Stage Disease Has No Symptoms
Credits: iStock
Prostate cancer deaths in the United States were on the decline, thanks to advances in screening and treatment but new data from the American Cancer Society (ACS) shows that the tide is shifting — prostate cancer rates have been climbing steadily for the past decade, particularly in advanced stages of the disease. At the same time, a new national survey highlights a troubling gap in public awareness, 80% of Americans don’t know that early-stage prostate cancer often has no symptoms, underscoring why early detection remains such a challenge.
According to the ACS’s latest prostate cancer statistics report, diagnoses of prostate cancer have increased by about 3% per year since 2014. This rise is particularly striking given that the decade before saw a 6.4% annual decline. What is most concerning is not only that more men are being diagnosed, but that more cases are being caught at advanced stages. The report notes that advanced-stage diagnoses are climbing at an even faster rate — up to 6.2% annually, depending on the age group.
Mortality trends add another layer of concern. In the 1990s and 2000s, prostate cancer death rates declined by 3% to 4% per year. Over the past decade, however, that rate of decline has slowed dramatically to just 0.6% annually.
Why is Prostate Cancer Screening Still Debatable?
One reason for the reversal may lie in the U.S. Preventive Services Task Force’s (USPSTF) guidance from the early 2010s, which advised against routine prostate-specific antigen (PSA) screening. The goal was to reduce overdiagnosis and overtreatment, as PSA testing can detect cancers that are slow-growing and unlikely to ever cause harm.
But the shift away from routine screening may have had unintended consequences. With fewer men undergoing PSA tests, cancers are now being discovered later and at more aggressive stages. “We actually see PSA testing this decade versus the previous decade going down, so the incidence [of prostate cancer] is going up despite less testing occurring,” experts from ACS noted. “That starts to speak to other factors that might be environmental or nutritional or other things that we don’t fully understand.”
The paradox is clear: cutting back on PSA tests may have reduced overdiagnosis, but it may also be fueling the resurgence of advanced-stage disease.
Why Are Americans in the Dark About Prostate Cancer Detection?
Compounding the problem is public misunderstanding of prostate cancer symptoms. A nationwide survey conducted by The Ohio State University Comprehensive Cancer Center revealed that four out of five Americans don’t know early-stage prostate cancer often has no symptoms at all. Most cases are detected only through routine screening, usually via a blood test for PSA levels.
The survey also found that 59% of respondents did not know sexual dysfunction can be a warning sign. Often, it’s partners who first notice these changes and encourage men to seek medical care. Other lesser-known symptoms — such as fatigue or unexplained weight loss — were better recognized by Black adults than by white adults, but Black respondents were less likely to know that early-stage disease can be asymptomatic.
This knowledge gap matters. When men assume they’ll feel ill if something is wrong, they’re less likely to prioritize regular screenings.
The ACS report also highlights stark racial disparities. Black men are twice as likely to die from prostate cancer as men from any other racial or ethnic group. Native American men, meanwhile, have a 12% higher death rate compared to white men despite a 13% lower incidence of the disease.
The reasons for these disparities are complex, involving a mix of biology, access to care, socioeconomic factors, and structural inequities in healthcare. What remains clear is that certain populations are paying a higher price for gaps in screening and treatment access.
Most common cancer in US men, Prostate cancer accounts for about 30% of male cancer diagnoses in 2025. Second leading cause of cancer death: After lung cancer, prostate cancer kills nearly 36,000 men annually in the U.S.
Annual cases: More than 300,000 American men are expected to be diagnosed in 2025.
Age factor: The majority of cases occur in men over 50.
Why Is Prostate Cancer Screening Crucial?
While the debate over PSA testing continues, experts agree on one point: men need to have informed conversations with their doctors about screening. The ACS and other organizations recommend that men aged 45 and older talk with their healthcare providers about the benefits and risks. For those at higher risk including Black men and those with a family history of prostate cancer — those discussions should begin as early as age 40.
Screening can be a double-edged sword. It may detect cancers that grow slowly and never cause harm, but it can also catch aggressive cancers before they spread. Without it, many men may not realize they’re sick until it’s too late for curative treatment.
Ohio State Cancer Center patient Daryl Wilber and his wife, Jodi, were shocked when a routine blood test revealed he had early-stage prostate cancer. He had no symptoms. For Jodi, the lesson is clear: partners play a vital role in men’s health. “Help them get over that hump from going from ‘Yeah, yeah, yeah, I know I should do it’ to, ‘OK, I’m going to go tomorrow and do it,’” she said.
Their story echoes what oncologists stress — early detection saves lives. Because prostate cancer often progresses slowly, finding it early greatly improves survival odds.
What are The Pros and Cons of Screening?
PSA testing and digital rectal exams remain the two primary tools for early detection. But both come with limitations. Elevated PSA doesn’t always mean cancer, and not all prostate cancers need immediate treatment. Some may never grow large enough to cause harm, leading to unnecessary treatments that carry risks such as urinary incontinence and erectile dysfunction.
That’s why many doctors recommend “shared decision-making”, weighing the risks and benefits together with the patient. Screening is not a one-size-fits-all solution. The right approach depends on age, race, family history, and personal health values.
The ACS projects nearly 314,000 new prostate cancer cases in 2025. That number, coupled with the slowed progress in reducing mortality, signals a pressing need to rethink screening strategies and public education.
Too many men and their families still believe symptoms will be obvious. Too many assume prostate cancer is always slow-growing. And too many at-risk populations lack access to timely testing and care.
© 2024 Bennett, Coleman & Company Limited

