- Health Conditions A-Z
- Health & Wellness
- Nutrition
- Fitness
- Health News
- Ayurveda
- Videos
- Medicine A-Z
- Parenting
- Web Stories
Expecting? Here's What The New Gestational Diabetes Testing Rules Mean For You

Credits: Canva
In a significant update to maternal health care, Australia is introducing new national guidelines on how pregnant women are tested for gestational diabetes.
The changes, released by the Australasian Diabetes in Pregnancy Society and published in the Medical Journal of Australia, mark the first major update to gestational diabetes screening in over a decade. These revised guidelines are expected to impact more than 280,000 pregnant women annually, streamlining care, reducing overdiagnosis, and focusing medical resources where they are most needed.
What Is Gestational Diabetes and Why Is Testing Important?
Gestational diabetes mellitus (GDM) is a temporary form of diabetes that occurs during pregnancy. It’s defined by high blood glucose (sugar) levels that are first detected while a woman is pregnant. In Australia, GDM affects nearly one in five pregnancies and has short- and long-term health implications for both mother and baby.
Though GDM usually resolves after delivery, women who develop it are seven times more likely to later develop type 2 diabetes. Identifying and managing GDM is essential because untreated cases increase the risk of:
Macrosomia (a baby born significantly larger than average), which can lead to birth complications and higher rates of caesarean sections
Pre-eclampsia, a dangerous condition involving high blood pressure and potential organ damage
Premature birth and other serious outcomes
Moreover, the screening process offers a gateway for introducing long-term health interventions like dietary advice, physical activity plans, and future diabetes prevention programs.
Why Are the Guidelines Changing?
While GDM screening and treatment are beneficial for many women, a one-size-fits-all approach has downsides. The new guidelines aim to balance the benefits of early detection with the potential harms of overdiagnosis. Studies and patient feedback have highlighted several concerns with the current system:
Women report stress, shame, and stigma after diagnosis
Limited access to specialist care and nutrition support
Some women adopt overly restrictive diets without professional guidance
Others are forced to change their maternity care provider or place of delivery due to a high-risk classification
The aim is to reduce unnecessary interventions for women at low risk, while enhancing care for those who truly need it.
What Exactly Is Changing?
The revised recommendations result from a broad review of current research and expert input from medical professionals and consumers. Here are the key updates:
Universal Screening Remains – But With Adjustments
All pregnant women without a prior diabetes diagnosis will still undergo routine screening between 24 and 28 weeks using the Oral Glucose Tolerance Test (OGTT). This test involves:
- Fasting overnight
- A baseline blood test
- Drinking a sugary solution
- Two follow-up blood tests over two hours
However, fewer women will undergo multiple OGTTs during pregnancy. Early testing will be more targeted based on risk.
Early Testing for High-Risk Women
Women with risk factors will be screened earlier in pregnancy, ideally between 10 and 14 weeks. The approach includes:
An HbA1c test (a non-fasting blood test that gives an average of blood sugar levels over the past 2–3 months) in the first trimester for women with risk factors such as:
- High body mass index (BMI)
- Previous large baby
- History of gestational diabetes
If results show high HbA1c or there’s a history of GDM, women may undergo an OGTT early in pregnancy.
Stricter Diagnostic Thresholds
The cut-off values for diagnosing GDM using the OGTT have been adjusted upward. This means only women with more clearly elevated glucose levels will be diagnosed. The goal is to avoid labeling borderline cases as diabetic when the risks and outcomes are minimal.
What Do These Changes Mean for Women?
The updated guidelines aim to make gestational diabetes care more precise and patient-centered:
- Fewer unnecessary diagnoses for women with mild or borderline glucose levels
- Improved access to services for those at higher risk
- Reduced stress and confusion from unclear diagnosis or overtreatment
- Stronger support systems for managing diet and physical activity safely
Importantly, women are encouraged to maintain open communication with their health care providers, especially if they have risk factors or symptoms like fatigue, excessive thirst, or frequent urination during pregnancy.
Jana Duggar Announces Pregnancy At 35, Here's What New Mothers In Their 30s Should Pay Attention To

Credits: Instagram
Jana Duggar, 35, days after celebrating her first wedding anniversary with her husband Stephen Wissmann, announced that they are expecting their first baby. The 19 Kids and Counting star said that the baby is expected to arrive in January 2026 and that the couple is "counting down the days and eagerly looking forward to this thrilling new chapter".
As Duggar looks forward to this new chapter in her life, it does raise an important question: How safe is it to have your baby after 30?
As per the National Institute of Health (NIH), US (2022), 20% of women in the US are now having their first child after the age of 35. While it is the new trend, the NIH doctor Dr Alan Decherney, a fertility expert explains that "As women age, they are still fertile, but their odds of pregnancy are decreased because they are not making as many good eggs that will fertile and divide normally and turn out to be an embryo."
ALSO READ: Women Are Now Waiting More Before Becoming A Mother, Age Trend Shows Motherhood From 2016 to 2023
Is Getting Pregnant More Difficult After 30?
After age 30, a woman's fertility decreases ever year, notes the NIH July 2022 issue. It notes: "The number and quality of her eggs goes down until she reaches menopause."
However, experts do point out that getting pregnant in your 30s need not be a stressful affair at all times. As it is at this age when you experience more stability, and also someone you know who have a personal experience in handling one. Most important, you are more mature at this age, which you may not be in your 20s.
ALSO READ: Baby Born From 30-Year-Old Frozen Embryo Sets Record: Here's All That We Know About It
Are You Planning Your Pregnancy After 30s? Here's How To Do It Right
Quit Habits: If you are a smoker, or consume alcohol, this is a good time to leave it.
Reduce Stress: While pregnancy for some can bring stress, try to find activities that help you release it.
Healthy Weight: Ensure that your weight is right, reduce your waist to bring it to a healthy range for a healthy pregnancy.
Food Habits: Stop eating junk and start eating more whole grains.
Exercise: A sedentary lifestyle can impact negatively on the child. You do not have to do HIIT, however, regular easy workouts can make both the pregnancy and delivery easy.
What Women In Their 30s Should Be Ready For During Pregnancy?
Dr Michelle Y Owens, professor of obstetrics and gynecology and a practicing maternal-fetal medicine specialist at the University of Mississippi Medical Center in Jackson, writes for the American College of Obstetricians and Gynecologists (ACOG) that "the longer your eggs have been around, the more likely they are to produce a pregnancy with a chromosome problem that can lead to a condition like Down syndrome. The risk goes up significantly after 35."
However, she says, there is a good news. Now, we have tools to detect and respond to pregnancy complications early.
READ: Expecting? Here's What The New Gestational Diabetes Testing Rules Mean For You
Why First Trimester Is Important For You And Your Baby?
As per the Johns Hopkins Medicine, your first prenatal visit is the most thorough, this is when your complete medical history is taken, physical examination is done and certain tests and procedures are performed to assess the health of both you and your child.
This is also the time when the fetus is most susceptible to damage from substances like alcohol, drugs and certain medicines, and illnesses like rubella, thus this is the most crucial time for the parents. First trimester is also the time when the baby undergoes a lot of development, while it may not be seen from the baby bump, however, the amniotic sac, placenta and the umbilical cord are all developed during this stage.
Since a lot of development happens during this stage, Dr Owens notes that this is why having a prenatal screening test during the first trimester helps you understand your baby's development and if your baby is at risk for any genetic disorders. "More frequent ultrasounds can measure the growth of the fetus and also look for birth defects. We’ll check your blood pressure at every prenatal visit, and we'll test you for gestational diabetes too. Early diagnosis plus treatment creates the formula for the best possible outcomes," she writes.
Paracetamol During Pregnancy Could Cause Neurodevelopment Disorders In Newborns – Study

(Credit-Canva)
Pregnancy is a sensitive and difficult time for expectant mothers. They must be careful about what they eat and how long they are active. It is also advisable for them to avoid certain medications, unless they have been prescribed by a doctor. As you may know, what the mother consumes will eventually affect the child, so while something that the mother can handle can be fatal to the child as it is at a very vulnerable stage. As such, a few studies have suggested that consuming medications like paracetamol can affect the child’s brain.
A new study published in the BioMed Central suggests that taking paracetamol (also known as acetaminophen) during pregnancy might be linked to a higher risk of autism and ADHD in children. This is a significant finding because paracetamol is a very common over-the-counter medicine that many pregnant women take for headaches, pain, or fever.
Researchers from the Icahn School of Medicine at Mount Sinai looked at 46 past studies involving more than 100,000 people. They found that the better-quality studies were more likely to show a connection between using paracetamol during pregnancy and a child's risk of developing these disorders.
How Does Paracetamol Affects Pregnancy And The Baby?
The researchers believe there could be a biological reason for this connection. They explain that when a pregnant person takes paracetamol, the medicine can cross from their body to the baby. Once there, it might cause stress to the baby's cells, mess with their hormones, and even change how their genes behave. These changes could interfere with the normal development of the baby's brain.
Since the number of autism and ADHD cases seems to be increasing around the world, these findings are very important. They could change how doctors and health officials think about the use of this common drug during pregnancy.
Should Pregnant Women Take Paracetamol For Pregnancy?
It's important to remember that this study does not prove that paracetamol directly causes autism or ADHD. However, the evidence is strong enough to raise concerns about how much it's being used.
Because of these findings, the study's authors suggest that pregnant women should use paracetamol with caution, for a short period of time, and only under a doctor's guidance. They also say that more research is needed to fully confirm these results and understand the risks.
Is This Accurate For All Children?
While it is ok to be cautious, there are other studies that do not draw the same conclusion. A 2024 study published in the JAMA network found no such link. The study suggested that using paracetamol during pregnancy does not increase a child's risk of developing autism, ADHD, or intellectual disability. This finding goes against some previous studies and is important for managing pain and fever during pregnancy. The study, which looked at over 2.4 million children born in Sweden, found that a direct link could not be made when other factors were considered.
What the Sibling Study Showed
When the researchers compared the siblings, they found no evidence that paracetamol use during pregnancy was linked to a higher risk of autism, ADHD, or intellectual disability.
- The risk for autism, ADHD, and intellectual disability was virtually the same in the exposed and unexposed siblings.
- The study found no connection even when mothers took more paracetamol.
This suggests that the slight link found in the initial analysis was likely due to "confounding factors," meaning other family-related reasons—not the medication itself—were responsible for the difference in risk. For example, a mother with a certain condition that requires her to take paracetamol might also have a genetic trait that affects her children.
In short, this new research provides strong evidence that paracetamol use during pregnancy is not a direct cause of these neurodevelopmental disorders.
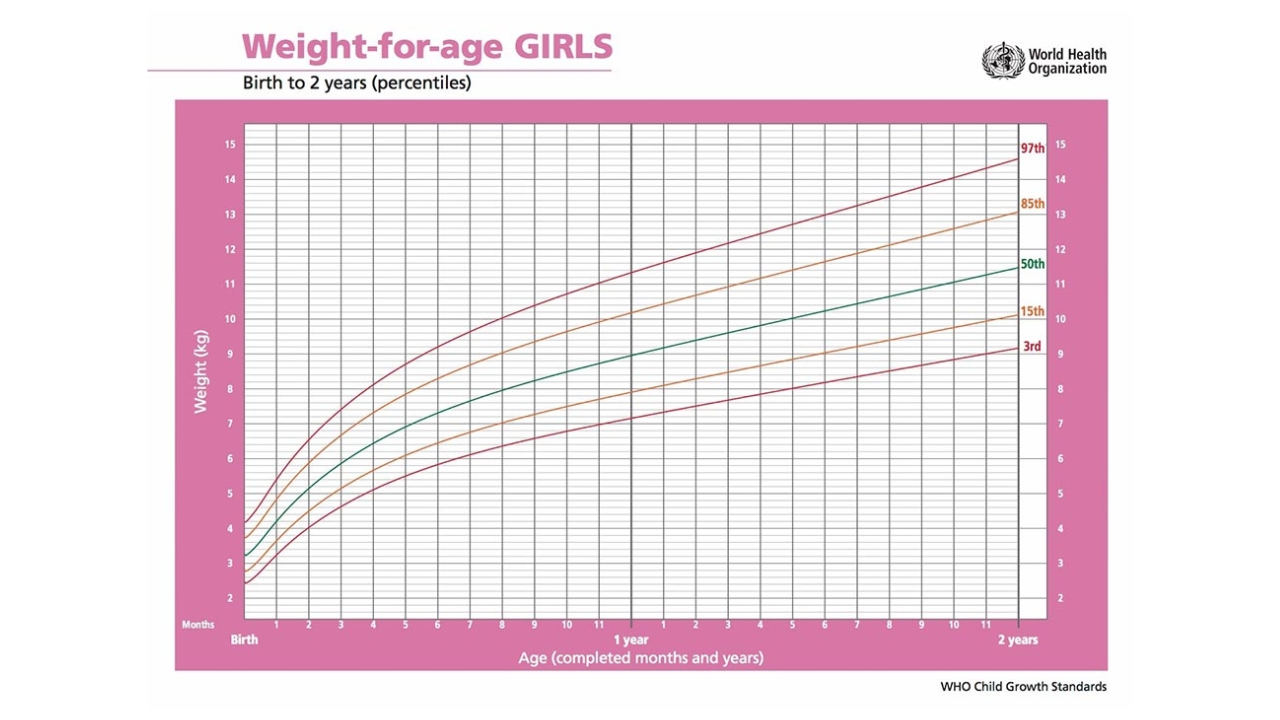
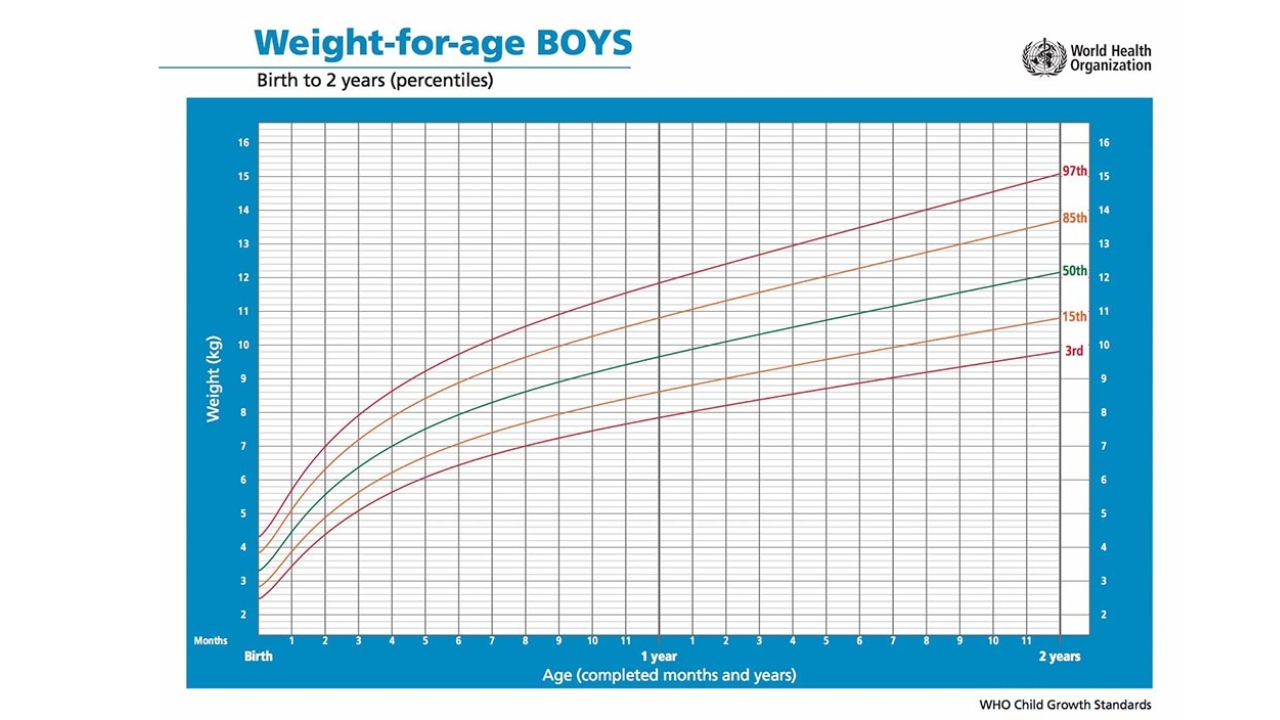
How To Decipher What Percentile Your Baby Is Using A Growth Chart?

Credits: Canva
An infant growth chart is a tool that helps parents, doctors, and other health professionals track a baby’s growth over time. By recording key measurements, it gives a clear picture of how your baby is developing compared to healthy growth standards.
The chart records three main measurements:
- Length (height)
- Weight
- Head circumference
These details are plotted so you can see how they change as your baby grows. The vertical axis shows the measurement, while the horizontal axis shows your baby’s age.
Growth charts are more than just numbers. They help assess your baby’s overall health and nutrition. Charts differ for boys and girls, as well as for infants and older children. For babies aged 0 to 2 years, the World Health Organization (WHO) growth standards are used. From 2 years onwards, most states and territories use growth charts based on the US Centers for Disease Control (CDC).
You will usually find a growth chart in your child’s personal health record, which may come in different colours depending on where you live. Parents can also register their child for a My Health Record, a digital platform where healthcare providers can upload growth information and other health updates.
What Are Percentiles?
Percentiles are a common way of showing growth patterns on a chart. They compare your baby’s measurements with those of other babies of the same age.
For example:
- A baby on the 50th percentile for weight is right in the middle. Half of babies the same age weigh less, and half weigh more.
- A baby on the 5th percentile for weight is lighter than 95% of babies that age.
- A baby on the 90th percentile for weight is heavier than 90% of babies that age.
ALSO READ: 99th Percentile Baby: What It Means, Risks, And What Parents Should Know
Every baby grows at their own pace. Some are naturally smaller, others naturally bigger. What matters most is that your baby follows a steady growth pattern over time.
How Growth Charts Are Used
Growth charts help identify whether your baby is following a healthy growth curve. While it is not necessary for a child to match the curve exactly, their growth should generally follow a consistent path.
Your baby is first weighed and measured at birth. It is normal for newborns to lose some weight in the first few days, which is why they are often weighed again at two weeks to check if they have returned to their birth weight. After that, regular growth checks are recommended, usually monthly in the first year.
Routine health checks continue throughout childhood, with growth charts used until a child turns 18. The timing of these checks may vary depending on your state or territory.
Measuring Your Baby
Special infant scales are used for babies up to 20 kilograms. Newborns are weighed lying down, without clothes or a nappy, to ensure accuracy. After the age of 2, children are weighed standing up in light clothing.
Head circumference is measured with a tape measure to track brain and skull growth.
For babies born prematurely, a corrected age is used until they are 2 years old. This adjustment accounts for the number of weeks they were born early. For example, a 4-month-old baby born one month early would have a corrected age of 3 months for growth chart purposes.
When to Seek Advice
A growth chart is a helpful tool, but it is not the only indicator of a baby’s health. Other signs of healthy development include:
- At least five very wet nappies each day
- Pale urine
- Soft, well-sized bowel movements
- Regaining birth weight by 14 days old
- Contentment between feeds
Most babies double their birth weight by around 4 months. If weight gain is slower than expected, it could be due to feeding difficulties, illness, or other health issues.
If your baby’s growth percentile drops significantly or weight gain remains low, speak to your doctor or child health nurse. They can assess the overall growth trend and investigate if needed.
Finally, avoid comparing your baby’s growth to others. Healthy growth looks different for every child, and the goal is steady development through infancy and beyond.
© 2024 Bennett, Coleman & Company Limited

