- Health Conditions A-Z
- Health & Wellness
- Nutrition
- Fitness
- Health News
- Ayurveda
- Videos
- Medicine A-Z
- Parenting
Postpartum Nutrition Guide: Foods Every New Mom Needs For Recovery And Lactation

Becoming a mother is a life-changing experience that goes far beyond delivery. The postpartum period, sometimes referred to as the "fourth trimester," is an important time for physical recovery and emotional adjustment. Nutrition is a critical component in this period of replenishing the body, facilitating healing, and aiding lactation. A very restrictive diet might have been allowed during pregnancy. In contrast, the postpartum diet will be more accommodating of a diversity of nourishing foods that your body and your baby need to thrive.
Having carried a baby for nine months, endured the pain of labor, and labored through delivery, your body now needs to heal. Nutrition provides the basis of energy restoration, healing tissues, and support for the production of milk in breastfeeding.
As Avni Kaul, Nutritionist, Dietician, and Wellness Coach, puts it, "This time is associated with tremendous physiological changes and psychological shifts. An appropriate diet in the postpartum period helps in healing, increases milk production, and overall health."
Benefits of a Nutrient-Rich Postpartum Diet
- Speeds Recovery: Nutrient-rich foods help in tissue repair, iron replenishment, and prevention of complications like postpartum anemia.
- Helps Produce Milk: Proper hydration and nutrition help in achieving the necessary quality milk supply.
- Boosts Wellness: Balanced diet offers energy required for a new mother's challenging role.
- Overindulgence is permissible once in a while, but it is the healthier diet that would prove best for effective recovery and lactation.
Essential Nutrients for Postpartum Recovery
1. Protein: The Basis of Recovery
Protein will assist your body to rebuild and regenerate tissues of damaged parts that need repairing in cases after delivery and in making more protein for production of the milk into the baby. Top sources are: eggs, lean meats, poultry, fish, tofu, lentils, beans, and dairy products.
2. Iron: Replace your depleted reserves
Blood loss during delivery can cause a decrease in iron levels, which may lead to weakness and a weakened immune system. Iron-rich foods with vitamin C can help restore these levels and prevent anemia.
Top sources: Spinach, red meat, liver, beans, fortified cereals, and broccoli.
Vitamin C-rich foods: Citrus fruits, bell peppers, tomatoes, and strawberries.
3. Fiber: Maintaining Digestive Health
Constipation is common postpartum due to hormonal changes and reduced physical activity. Fiber-rich foods aid digestion and prevent constipation.
Top sources: Whole grains, oats, fruits, vegetables, and legumes.
4. Hydration: The Backbone of Milk Production
Lactation and hydration depend on adequate fluid intake. Target 8-10 glasses of fluids daily, including water, herbal teas, and broths. Electrolyte-rich fluids can also balance the body after delivery.
5. Vitamin B12 and Folate: Energizing and Restoring Nerve Health
B vitamins include B12 and folate. They play an important role in energy production, nerve function, and blood cell formation. These vitamins can combat postnatal fatigue and replace the blood that has been lost in delivery.
Top sources: Eggs, dairy products, beef, fish, fortified cereals, and leafy greens such as spinach and kale.
Postpartum Superfoods for Recovery and Lactation
Some foods go beyond supporting postpartum recovery and milk supply:
- Turmeric: It is the ant-inflammatory remedy in which inflammation swelling is decreased to heal well and fast.
- Fenugreek: It was historically used to augment milk.
- Oats rich in fibers with iron it keeps digestion very simple and can easily take energy with ease.
- Almond: Rich with Healthy fats and calcium almonds ensure tissue repairing.
Foods to Avoid During Postpartum
While most foods are safe, certain items should be limited or avoided for better recovery and breastfeeding outcomes:
- Caffeine: Excessive caffeine can pass into breast milk, disrupting your baby's sleep.
- Alcohol: If consuming alcohol, wait several hours before breastfeeding to ensure it doesn’t affect your milk.
- Highly Processed Foods: These are often nutrient-deficient and may contribute to fatigue.
Should New Moms Take Postpartum Vitamins?
Consult your doctor about continuing prenatal vitamins or switching to a postpartum-specific supplement. According to Avni Kaul, "Some women may need to continue prenatal vitamins while breastfeeding, while others might benefit from standard multivitamins." A healthcare provider can tailor recommendations based on your individual needs.
When Breastfeeding Twins Should You be Doubling Your Nutrition?
For mothers who nurse twins, there is an addition of around 500 calories a day per baby. Adequate hydration and the intake of calorie-rich foods is essential for each baby to thrive. Checking on wet and soiled diapers can also assure that each is being fed and hydrated correctly.
Postpartum nutrition is more than just sustenance. It fuels recovery, supports lactation, and empowers new mothers to take on the physical and emotional challenges of early motherhood. A diet rich in real, nutrient-dense foods aids in healing, replenishes energy, and strengthens the bond between mother and baby.
As Avni Kaul emphasizes, "Proper nutrition is the cornerstone of recovery, providing the strength and vitality needed during this transformative time." For personalized guidance, consulting a nutritionist or healthcare provider can help ensure your postpartum diet meets your unique needs.
Avni Kaul is a Nutritionist, Dietician and a Wellness Coach with Specialisation in Pregnancy Health and Founder of Nutri Activania in India.
COVID Vaccination Is Not Linked To Reduce In Childbirth, Says Study

Credits: iStock and Canva
A large population-based study from Linköping University in Sweden has found no evidence that COVID-19 vaccination caused a decline in childbirth during the pandemic, countering persistent rumors that mRNA vaccines affect fertility. The findings have been published in the peer-reviewed journal Communications Medicine.
The study was conducted amid widespread misinformation, particularly on social media, suggesting that COVID-19 vaccines reduce the chances of becoming pregnant. These claims gained traction as several countries, including Sweden, recorded a drop in birth rates during the later stages of the pandemic, prompting questions about a possible link to vaccination.
“Our conclusion is that it’s highly unlikely that the mRNA vaccine against COVID-19 was behind the decrease in childbirth during the pandemic,” said Toomas Timpka, professor of social medicine at Linköping University and one of the study’s authors.
Why Researchers Investigated the Claim
Since the early months of the pandemic, unverified claims about vaccines and fertility have circulated widely online. When official data later showed fewer babies being born in some regions, researchers decided to examine whether vaccination could plausibly explain the trend or whether other social and demographic factors were at play.
Read: Ahmedabad Toddler Swallows Hulk Toy, Showed X-Ray, Doctors Remove It Via Endoscopy
To address the issue, the research team carried out an extensive analysis using real-world healthcare data rather than surveys or self-reported outcomes.
Study Looks at Nearly 60,000 Women
The study analyzed health records of all women aged 18 to 45 years living in Region Jönköping County, a region with a total population of around 369,000 people. This amounted to nearly 60,000 women included in the analysis.
Between 2021 and 2024, about 75 per cent of these women received at least one dose of a COVID-19 vaccine. Researchers examined data on childbirths, registered miscarriages, vaccination status and deaths using official healthcare records, allowing for a comprehensive comparison between vaccinated and unvaccinated groups.
Importantly, the researchers adjusted their analysis for age, recognizing that age is one of the most significant factors influencing fertility and pregnancy outcomes.
No Difference in Births or Miscarriages
When childbirth rates were compared between vaccinated and unvaccinated women, the researchers found no statistically significant difference. The same held true for miscarriage rates among women who became pregnant during the study period.
“We see no difference in childbirth rates between those who have taken the vaccine and those who haven’t,” said Timpka. “We’ve also looked at all registered miscarriages among those who became pregnant, and we see no difference between the groups there either.”
These findings align with several earlier international studies that have similarly found no association between COVID-19 vaccination and reduced fertility.
Other Factors Likely Behind Falling Birth Rates
According to the researchers, the decline in childbirth observed during the pandemic is more plausibly explained by broader demographic and social trends.
People currently in their 30s, the age group most likely to have children, were born in the second half of the 1990s. That period was marked by economic challenges and lower birth rates in Sweden, meaning today’s pool of potential parents is smaller than in previous generations.
In addition, pandemic-related factors such as health concerns, economic uncertainty, delayed family planning and lifestyle changes during lockdowns may have contributed to fewer pregnancies.
One of the study’s key strengths is its large, representative sample drawn from an entire region rather than a selected group. By using verified healthcare records and accounting for age-related effects, the researchers aimed to minimize bias and improve reliability.
The study received financial support from several sources, including the Swedish Research Council.
Ahmedabad Toddler Swallows Hulk Toy, Showed X-Ray, Doctors Remove It Via Endoscopy
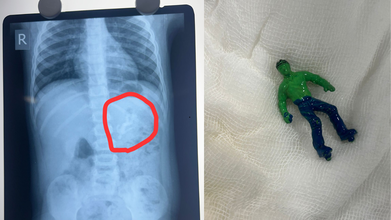
Credits: X
Ahmedabad toddler, one-and-a-half-year-old boy swallowed a 'Hulk' toy, which is based on a popular comic superhero. The toy was stuck in his stomach when his parents took him to the Civil Hospital. According to reports by News18, the child is identified as Vansh who showed the signs of discomfort and began vomiting. This is what alarmed the parents.
As per the News18 report, his mother Bhavika was suspicious when she noticed that one of his toys was missing. The child was rushed to the hospital and an X-ray revealed that he had swallowed the entire plastic toy. The toy was not broken.
Hindustan Times reported that Dr Rakesh Joshi, Head of the Department of Pediatric Surgery removed the toy through upper GI endoscopy. "Had it been a little late, the toy could have moved further from the stomach and got stuck in the intestines. In that case, there would have been a risk of intestinal blockage and even rupture," the senior doctor said.
"There is a natural valve between the esophagus and the stomach. The biggest challenge was to take out a whole toy through this valve. When we tried to grab it with the endoscope, the toy kept slipping because of the air in the stomach. Pulling the toy by its hand or foot raised the possibility of it getting stuck in the valve and causing it permanent damage," he said.
The doctor noted that if the toy had further slipped down, it would have increased the risk of intestine rupturing.
Ahmedabad Toddler Swallows Hulk Toy: What Parents Must Keep In Their Mind
Under the Toys (Quality Control) Order, 2020 issued by the Department for Promotion of Industry and Internal Trade under the Ministry of Commerce and Industry, toy safety in India was brought under mandatory BIS certification from September 1, 2020. The move aims to ensure safer toys for children while also supporting the government’s policy of curbing non-essential imports.
Industry sources estimate that more than 85 percent of toys sold in India are imported. Officials say the Toys Quality Control Order is a key step in preventing the entry of cheap and substandard toys into the domestic market, many of which fail to meet basic safety requirements.
Ahmedabad Toddler Swallows Hulk Toy: Standards for Electric and Non-Electric Toys
The quality control order clearly defines safety standards based on the type of toy. Non-electric toys such as dolls, rattles, puzzles, and board games must comply with IS 9873 (Part 1):2019. These toys do not rely on electricity for any of their functions.
Electric toys, which include at least one function powered by electricity, are required to meet the standards outlined under IS 15644:2006. Compliance with these standards is mandatory before such toys can be sold in the Indian market.
Ahmedabad Toddler Swallows Hulk Toy: Risks Linked to Untested Toys
Toys that are not tested by NABL-accredited toy testing laboratories can pose serious health risks to children. Sharp edges and poorly finished parts can cause cuts and injuries. PVC toys may contain phthalates, which are considered harmful chemicals.
Many low-quality toys have also been found to contain lead, a substance known to be particularly damaging to brain development in children. Soft toys with fur or hair can trigger allergies or become choking hazards. In some cases, small body parts can get stuck in gaps or holes, increasing the risk of injury.
Testing by NABL-accredited laboratories ensures that toys are safe, durable, and suitable for specific age groups. Parents are advised to check for IS marks on toys before purchasing, as this indicates compliance with Indian safety standards.
Ahmedabad Toddler Swallows Hulk Toy: What Parents Should Check Before Buying Toys
Experts recommend avoiding toys with small detachable parts for toddlers and young children, as they are more likely to put objects in their mouths. Toys should always match the child’s age, skill level, and interests.
Parents are also urged to look for IS marks, which confirm that the toy has been tested and certified. Loud toys should be avoided, as prolonged exposure to sounds above 85 decibels can harm a child’s hearing.
Electric toys with heating elements should be used with caution or avoided altogether due to burn risks. Finally, toys with sharp edges or shooting components should be carefully examined to prevent cuts and injuries.
Tech And Devices Have 'Horrific' Impact On Kids, Says Study

Credits: iStock
Doctors across the UK are raising the alarm over what they describe as mounting evidence of serious health harms linked to excessive screen time and unrestricted access to digital content among children and young people.
The Academy of Medical Royal Colleges (AoMRC), which represents 23 medical royal colleges and faculties, says frontline clinicians are witnessing deeply concerning patterns across the NHS. According to the academy, doctors working in primary care, hospitals and community settings have shared firsthand accounts of what they describe as “horrific cases” affecting both physical and mental health.
Evidence From the Frontline
The academy has now launched a formal evidence-gathering exercise to better understand the harms clinicians are repeatedly encountering and whether these can be attributed to technology use and digital devices.
Its aim is twofold. First, to shine a light on risks that often go unnoticed, including prolonged screen time and exposure to harmful online content. Second, to develop guidance for healthcare professionals on how to identify, address and manage these issues in clinical practice.
In a statement, the AoMRC said it already has evidence pointing to significant impacts on children’s wellbeing, ranging from physical concerns to mental health challenges linked to both excessive device use and harmful online material. The work is expected to be completed within three months.
A Public Health Emergency?
Dr Jeanette Dickson, chair of the academy, said the scale of the problem is becoming impossible to ignore. Speaking to The Sunday Times, she warned that clinicians may be witnessing the early stages of a public health emergency.
“Everywhere we look, we see children and adults glued to their screens,” she said. “I really worry for children, some of whom are self-evidently imprisoned in a digital bubble.”
Copies of the academy’s letter outlining these concerns have been sent to Health Secretary Wes Streeting and Science and Technology Secretary Liz Kendall, as well as Lucy Chappell, chief executive of the National Institute for Health Research, and the government’s chief medical adviser, Sir Chris Whitty.
Government Action and Global Trends
The warnings come as the UK government prepares to consult on possible restrictions on social media use for under-16s. Options under consideration range from a complete ban to more targeted measures such as time limits and tighter controls on algorithms.
Recent government research has already linked screen time to poorer speech development in children under five. Internationally, the debate is gaining pace. Australia introduced a ban on under-16s holding social media accounts in December, while countries including France, Denmark, Norway and Malaysia are weighing similar steps.
Why Some Groups Oppose a Blanket Ban
Not everyone agrees that an outright ban is the answer. A joint statement signed by 43 child protection charities and online safety groups, including the NSPCC and the Molly Rose Foundation, warns that blanket bans could backfire.
Andy Burrows, chief executive of the Molly Rose Foundation, said parents and policymakers are being offered a false choice. “It’s being framed as either a total ban or the current appalling status quo,” he said. “Those aren’t the only options.”
Chris Sherwood, chief executive of the NSPCC, echoed the concern, pointing out that for many children, the internet provides vital support. “A blanket ban would take those spaces away overnight,” he said, “and risks pushing teenagers into darker, unregulated corners of the internet.”
Both organizations argue that the focus should shift to holding tech companies accountable for harmful design choices, unsafe algorithms and failures to protect young users.
© 2024 Bennett, Coleman & Company Limited

