- Health Conditions A-Z
- Health & Wellness
- Nutrition
- Fitness
- Health News
- Ayurveda
- Videos
- Medicine A-Z
- Parenting
- Web Stories
14-year-old Instagram Influencer Diagnosed With Acute Myeloid Leukemia Passes Away

Credits: Instagram
Zuza Beine, a 14-year-old Instagram influencer from Wisconsin who openly documented her battle with acute myeloid leukemia (AML), has died, her family announced Tuesday.
Diagnosed with AML at the age of 3, Zuza spent much of her childhood undergoing treatment. Despite the challenges, she connected with 1.8 million followers on her Instagram account, @zuzas_way_to_healing, where she shared both the struggles and small joys of living with cancer.
Her family confirmed her passing in a heartfelt statement on Instagram:
"It is with broken hearts that we share that Zuza died yesterday morning. She lived 11 of her 14 years with a relentless cancer, yet lived more fully and gratefully than most. Her being changed us forever, and her dying will too."

Over the years, Zuza became known for her candid videos, including her popular “Get Ready With Me” posts, where she openly discussed treatment, pain management, and daily routines. Just days before her death, she told followers about the intense pain she was experiencing. “I’m constantly on pain medicine because my body hurts so, so, so bad,” she said in a video posted last Thursday.
One day later, she shared another update: “I can barely walk right now I’m in so much pain.” Yet, her final video on Sunday, just hours before her passing, reflected gratitude for life’s smallest moments, a recurring theme in her posts.
Her family described Zuza as both brave and honest, saying her openness inspired many to find beauty even in hardship. “More than anything, she wanted to be a normal, healthy kid. But what made her life so beautiful was how she faced the hardest circumstances and still lived fully,” they wrote.
What Is Acute Myeloid Leukemia (AML)?
According to the National Institute of Health, US, AML is a rapidly progressing myeloid neoplasm characterized by the clonal expansion of primitive hematopoietic stem cells, known as blasts, in the bone marrow.
In other words, as the American Cancer Society describes, it is a type of cancer that starts in the blood-forming cells of the bone marrow. The Cancer Research UK explains that it starts from young white blood cells called granulocytes or monocytes in the bone borrow.
It is a rare cancer and happens when certain genes or chromosomes mutate.
Types of AML
Myeloid leukemia: Involves cells that would normally produce neutrophils, a type of white blood cell.
Acute monocytic leukemia (AML-M5): Affects cells that develop into monocytes, another white blood cell.
Acute megakaryocytic leukemia (AMLK): Involves cells that should produce platelets or red blood cells.
Acute promyelocytic leukemia (APL): Affects immature white blood cells called promyelocytes, preventing them from developing normally.
AML affects about 4 in every 100,000 adults each year. Roughly 1,160 children are diagnosed annually in the U.S.
Symptoms of Acute Myeloid Leukemia
In its early stages, AML can feel like a lingering cold or flu. Because it is aggressive, symptoms usually progress quickly and may include:
- Fatigue, weakness, or dizziness
- Fever and night sweats
- Easy bruising or bleeding (such as nosebleeds or bleeding gums)
- Frequent or persistent infections
- Loss of appetite and unexplained weight loss
- Shortness of breath
- Pale or cold skin
- Headaches or swollen lymph nodes
- Bone, back, or abdominal pain
- Tiny red spots on the skin (petechiae)
- Wounds or sores that don’t heal
'Nightmare Bacteria' Cases Increase By Nearly 70%, CDC Report Reveals: What Is It And How To Recognize It's First Signs

(Credit-Canva)
A recent report revealed that the number of infections from drug-resistant "nightmare bacteria" has jumped significantly in the US. The numbers of cases increased by almost 70% from 2019 to 2023. This information comes from a new report by scientists at the Centers for Disease Control and Prevention (CDC), US. These bacteria are becoming a major concern because they are harder to treat, making common infections potentially dangerous.
What Is Nightmare Bacteria?
According to the Association for Professionals in Infection Control and Epidemiology (APIC), "nightmare bacteria" are extremely dangerous germs because they have become resistant to almost all antibiotics, making them nearly impossible to treat. Some examples include VRSA (Vancomycin-resistant Staphylococcus aureus), Candida auris, and CRE (Carbapenem-resistant Enterobacterales). The CDC also estimates that more than 23,000 Americans die each year from infections that are resistant to antibiotics.
What Makes This Bacteria Immune To Drugs?
A big reason for this increase is a specific type of bacteria that has the NDM (New Delhi metallo beta lactamase) gene. This gene makes the bacteria resistant to most antibiotics. According to the CDC researchers, only two antibiotics can fight these infections, and they are expensive and have to be given through an IV (intravenous drip).
These bacteria with the NDM gene were once very rare in the U.S., usually found only in people who had received medical care in other countries. However, the number of U.S. cases has increased more than five times in recent years. Experts called this rise a "grave danger" and "very worrisome."
The CDC scientists also warned that many people might be carrying these drug-resistant bacteria without even knowing it, which could lead to them spreading easily in communities. This means that infections that have always been simple to treat, like a urinary tract infection (UTI), could become a long-term problem.
How Many Cases of Nightmare Bacteria Have Been Reported?
The researchers gathered data from 29 states that have the necessary systems to test for and report these drug-resistant bacteria. In 2023, they counted 4,341 cases of carbapenem-resistant infections in those states. Out of these, 1,831 were caused by the NDM-type bacteria. The report didn't mention how many people died from these infections.
The rate of carbapenem-resistant infections went from just under 2 per 100,000 people in 2019 to more than 3 per 100,000 in 2023, which is a 69% increase. Even more alarming, the rate of NDM cases shot up from about 0.25 to 1.35 per 100,000, an incredible 460% increase.
Experts believe this rapid increase is likely connected to the COVID-19 pandemic. They noted that there was a huge spike in antibiotic use during the pandemic, which probably led to the rise in drug resistance.
How Do You Contract Nightmare Bacteria?
APIC explains that you can only get sick from nightmare bacteria if you are exposed to them. They are most common in healthcare settings like hospitals and nursing homes. Patients who have devices like catheters, tubes, or drains may be at the highest risk.
Symptoms of these infections can vary.
- You might have a wound that won't heal or a serious bloodstream infection that leads to sepsis.
- It's also possible to carry these bacteria without showing any symptoms at all.
How Do You Prevent Getting Infected With Nightmare Bacteria?
Since these infections are so difficult to treat, prevention is key. Since these infections are so difficult to treat, prevention is key.
- Wash your hands often with soap and water or use an alcohol-based hand sanitizer.
- Ask others to clean their hands before they touch you or your surroundings.
- Tell your doctor if you have recently been cared for in another country or medical facility.
- Talk to your healthcare provider about how you can reduce your risk of infection, especially if you have a chronic health condition.
- Learn about antibiotics so you know when it's appropriate to take them, which helps prevent the spread of resistant germs.
Can Aspirin Stop Colorectal Cancer From Returning?
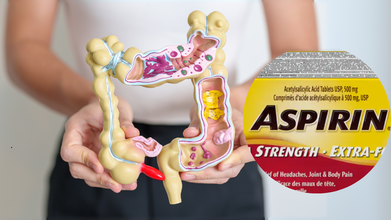
Credits: Canva
A daily low dose of aspirin could significantly reduce the risk of colorectal cancer returning in certain patients, according to a clinical trial published in the New England Journal of Medicine.
The study, conducted by researchers at the Karolinska Institute and Karolinska University Hospital in Sweden, involved 626 participants with stages 1 to 3 colon or rectal cancer whose tumors carried specific genetic mutations.
Why This Study Matters
Colorectal cancer affects about 2 million people worldwide every year, and between 30 to 40% of them experience a recurrence. Identifying low-cost, widely available treatments that can prevent relapse is critical in improving survival rates and easing the burden on healthcare systems.
This trial is particularly significant because while earlier observational studies suggested aspirin might benefit cancers with mutations in the PIK3 signaling pathway, this is the first time the theory has been tested in a randomized clinical trial.
The Trial Results
Participants were randomly assigned to either receive low-dose aspirin daily or a placebo. Over a follow-up period of three years, those in the aspirin group were up to 55 percent less likely to see their cancer return.
Aspirin group: 7.7% recurrence rate within three years
Placebo group: 14.1 to 16.8% recurrence rate, depending on mutation type
“Aspirin is a drug that is readily available globally and extremely inexpensive compared to many modern cancer drugs, which is very positive,” said lead researcher and surgeon Anna Martling from the Karolinska Institute.
How Aspirin May Work Against Cancer
Researchers believe aspirin helps prevent cancer recurrence in multiple ways:
- Reducing inflammation, which plays a role in tumor growth
- Restricting tumor cell proliferation
- Limiting platelet function, which cancer cells often exploit to spread and protect themselves
- Potentially disrupting the PIK3 pathway, slowing tumor development
While the exact molecular mechanisms remain unclear, the study provides strong biological evidence that aspirin could be effective in genetically defined subgroups of colorectal cancer patients.
Precision Medicine Potential
One major advantage highlighted by the researchers is that colorectal cancers are already screened for genetic mutations. In this study, more than one-third of cases involved the relevant PIK3 mutations. That means many patients could easily be identified as candidates for aspirin therapy without requiring additional costly tests.
“Aspirin is being tested here in a completely new context as a precision medicine treatment,” Martling noted. “This is a clear example of how we can use genetic information to personalize treatment and at the same time save both resources and suffering.”
Benefits and Risks
Low-dose aspirin has long been recognized for lowering the chances of repeat heart attacks and strokes. However, it is not without risks. Previous studies have linked aspirin use to an increased likelihood of internal bleeding and other complications.
The researchers stress that while the results are encouraging, more work is needed to confirm long-term benefits, identify which patients are most likely to benefit, and balance the risks against the potential advantages.
With millions of new colorectal cancer cases each year and a significant portion facing recurrence, this research opens the door to a simple, cost-effective approach to treatment. If confirmed in larger studies, aspirin could become a powerful tool in the fight against one of the world’s most common cancers.
What Is Jess's Rule? How A Missed Cancer Diagnosis Led To A New Rule For General Practitioners

(Credit-Andrea Brady)
GPs in England are being urged to adopt a “Jess’s Rule”, an initiative that urges doctors to rethink their treatment if, even after three patient appointments, the patient is still experiencing the same undiagnosed symptoms. This new initiative, called Jess's Rule, is being rolled out across the NHS to help prevent avoidable deaths by catching serious illnesses earlier, especially in young people. The rule is not a law, but a strong directive designed to make a more thorough diagnostic process standard practice nationwide.
Who Is Jess from Jess’s Rule?
While this new rule may help many people, it is a direct result of the tragic story of Jessica Brady. At just 27, she passed away from advanced stage 4 cancer in 2020. Before her diagnosis, she had more than twenty appointments with her GP practice over five months, all while her symptoms were getting progressively worse. Despite her persistence, her condition was repeatedly misdiagnosed or dismissed.
Ultimately, her family had to seek private care, and only then was she diagnosed with a type of cancer so advanced that no treatment was possible. She died just three weeks after her diagnosis. Jessica's story highlights the critical need for a system that ensures a patient's concerns are taken seriously, especially when initial treatments or diagnoses aren't working.
Who Is At Risk For Less Cancer Diagnoses?
A big aspect of Jess's Rule is its focus on reducing health inequalities. Studies have shown that younger patients and those from minority backgrounds often face delays in getting a proper diagnosis. One of the reasons given was that their symptoms might not fit the typical patterns seen in older or white patients, which then leads to their concerns being dismissed.
According to Gov.UK, a report found that half of all 16 to 24-year-olds with cancer needed three or more appointments to get a diagnosis. Jess's Rule is made to combat this problem by focusing on the fact that a patient's age or background should not be a reason to overlook a potential serious illness.
The NHS hopes that this rule, which is urged to be followed across the nation, will help ensure everyone receives the same high standard of care. This initiative is a tribute to Jessica's legacy and her family's tireless efforts to prevent other families from enduring similar grief.
How Does Jess’s Rule Work?
Jess's Rule isn't a strict law, but it's a guide for medical professionals. When a patient's symptoms don't improve after three appointments, the rule suggests that the GP should take further action. This step might include moving from phone consultations to a face-to-face appointment, conducting a more in-depth physical examination, or ordering additional tests.
It also encourages doctors to review the patient's records carefully, consult with a colleague for a second opinion, or refer the patient to a specialist. The aim is to formalize what many good doctors already do: if something isn't right, don't give up.
According to Health and Social Care Secretary Wes Streeting, Jessica's death was a "preventable and unnecessary tragedy," and Jess's Rule will ensure that every patient receives "thorough, compassionate, and safe care." The initiative is a collaborative effort between the Royal College of General Practitioners (RCGP) and NHS England.
© 2024 Bennett, Coleman & Company Limited

