- Health Conditions A-Z
- Health & Wellness
- Nutrition
- Fitness
- Health News
- Ayurveda
- Videos
- Medicine A-Z
- Parenting
An Existing Drug Can Replace Steroids To Help Asthma And COPD Patients, Reveals Lancet Study

Credits: Canva
"During a flare-up, it’s almost impossible to explain how you feel—you can barely breathe,” said 77-year-old Pointing from Banbury, England, in a recent news release.
For people like Pointing, a new clinical trial offers hope. Benralizumab, an existing injectable drug, may significantly reduce the severity of asthma and COPD attacks and could make it far less daunting, report researchers. The study is published in The Lancet Respiratory Medicine. While the drug has already been approved for treating asthma patients, it could also replace steroid medication as the go-to treatment for flare-ups.
What did The Study find?
As per the findings in the study, the monoclonal antibody outperformed steroids in reducing symptoms like coughing, wheezing, breathlessness, and phlegm production.
Trial results also showed that after three months, individuals taking benralizumab were four times less likely to experience an asthma or COPD attack compared to those on the steroid prednisolone.
The lead researcher Dr Mona Bafadhel, who is also the chair of respiratory Medicine at King's College London said, "This could be transformative for people with asthma and COPD. Treatment for these exacerbations hasn’t evolved in 50 years, despite causing 3.8 million deaths globally each year. Benralizumab, a safe and effective drug already used for severe asthma, showed greater effectiveness when given at the point of an exacerbation compared to steroid tablets, which are currently the only option available."
Pointing who was one of the participant of the trial, praised the drug and said that it was "fantastic" and that he did not experience the usual side effects he gets with the steroid tablets. "“Steroids used to ruin my sleep, especially the first night. But with benralizumab, I slept well and could go about my life without issues.”
How does Benralizumab work?
It targets eosinophils, a type of white blood cell that drives lung inflammation during flare-ups. Eosinophilic exacerbations account for about 30% of COPD attacks and nearly half of asthma attacks. These episodes also involve a surge in eosinophiles in the lungs, and cause severe wheezing, coughing, and chest tightness.
The trial placed patients into three groups: one received benralizumab during flare-ups, another was given prednisolone tablets, and a third received both. The benralizumab group not only had fewer symptoms, but it also took longer to develop a serious episode that necessitated medical attention or hospitalization.
The researchers also discovered that the injections increased the individuals' overall quality of life.
Although the medicine is now provided by healthcare professionals, researchers anticipate it will be safe to administer at home or in a doctor's office in the future.
“Our study demonstrates enormous potential for asthma and COPD treatment,” said Dr. Sanjay Ramakrishnan, clinical senior lecturer at the University of Western Australia and one of the researchers. “COPD is the third leading cause of death worldwide, yet treatment remains outdated. We need life-saving options to prevent these patients from running out of time.”
With 3.8 million deaths annually attributed to asthma and COPD, researchers hope benralizumab can soon provide a modern, effective solution for managing these life-threatening conditions.
Adenovirus Cases Rise In UK, Health Authorities On Alert

Credits: Canva
Adenovirus, or what some people are calling the mystery disease is going to be the next worry in the UK, after superflu had already grappled the healthcare system. Along with H3N2 and its variant superclade K, people are now worrying about this mystery disease.
Adenovirus is highly contagious and causes mild cold or flu-like symptoms, though severe cases could lead to stomach flu and vomiting. Many describe this virus as 'heartier' than others. The reason is that the virus can survive longer on surfaces and even resist the common disinfectants used. This is what makes it highly transmissible.
Is There Any Treatment For Adenovirus?
As of now, there is no treatment for adenovirus, it could however be managed and monitored. What helps is regular handwashing and thorough cleaning of surfaces.
The good news is that cases of adenovirus are actually dropping in the UK, as confirmed lab reports. The cases last week were 1.2 per cent, whereas the week prior, it was at 1.7 per cent, as also reported by the Independent.
What Are The Symptoms Of Adenovirus?
While a lot of the symptoms mimics of those in flu or COVID, including shortness of breath, a sore throat and or a runny nose. However, there are certain unique symptoms of adenovirus that include:
- Diarrhea
- Pink Eye or conjunctivitis
- Ear infection or otitis media
- Swollen lymph nodes
- Pneumonia
- Stomach pain
- Nausea
- Vomiting
Other rare symptoms could also include impact on your bladder or nervous system. As viruses in your bladder can also cause urinary tract infections, and the same virus in your nervous system can cause condition that can affect your brain. These conditions also include encephalitis and meningitis.
The symptoms usually start to subside within two days, however, if the symptoms stay even after three days without any relief, it might be a red flag. The best thing to do during such a situation is to go consult your GP.
Also Read: Unique Symptoms Of Mysterious Adenovirus And How Long Infection Now Last
Is Adenovirus Spreading Faster Than Flu and Covid?
Experts have noted that due to its ability to stay longer in the environment and being highly transmissible, it is in fact, spreading faster than flu and COVID. Eric Sachinwalla, Jefferson Health's medical director said that this virus is still unfamiliar and thus not much can actually be done to treat adenovirus. Speaking to PhillyMad, he said, "It is pretty contagious because it is heartier than other viruses - soap and water, or everyday disinfectant, won't kill it, so it tends to live in the environment longer."
What Are The Ways To Stay Safe From Adenovirus?
Since adenovirus spreads through close contact and is resistant to many everyday disinfectants, hygiene remains the key. The best way to stay safe is by avoiding close contact, especially with those who are unwell. You may also keep an eye on your symptoms, including your body temperature and take steps to prevent the virus from spreading by taking precautions, as well as getting the flu jab.
WHO Approves Two COVID-19 Rapid Antigen Tests, Check The Details Here
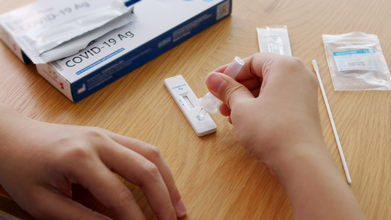
Credits: iStock
The World Health Organization (WHO) on December 24 prequalified two rapid antigen diagnostic tests (Ag-RDTs) for SARS-CoV-2. This virus is known to have caused COVID-19. As per the WHO, these two tests are called SD Biosensor STANDARD Q COVID-19 Ag Test and the ACON Biotech Flowflex SARS-CoV-2 Antigen Rapid Test (Self-Testing).
At first these tests got temporary emergency approval from the WHO during the pandemic. This was done so the countries could start using them quickly even though long-term data was limited. This emergency approval helped the tests reach over 100 countries when they were urgently needed.
What Has Changed Now?
The WHO has now given these tests full prequalification, which means it has a stronger and long-term approval. This means that the WHO has thoroughly checked and confirmed that the tests consistently meet global standards for quality, safety, and accuracy.
Why Does This Matter?
- The tests can now be officially bought and used by global organizations and governments
- They can be included in bulk purchasing to lower prices and increase supply
- This makes reliable COVID-19 testing more affordable and accessible, especially in low-and middle-income countries
COVID-19 Is Far From Being Over
Even though WHO officially ended COVID-19 emergency phase over two years ago, the virus is still circulating globally. In fact, this year, we have seen variants of COVID-19 circulating around, causing the most unique symptoms, including razor-blade like throat. Variants like JN.1, Stratus, Nimbus, LP8.1, and BA.3.2 were all that we saw in 2025.
While the good news is that infection levels are relatively stable, but the virus has not completely disappeared and testing is still necessary, especially in poorer countries.
Many low-income countries do not have easy access to labs or expensive PCR testing. So there is still a need for a strong, but cheaper and reliable way to detect COVID-19, and these tests may as well do that.
Why Rapid Antigen Test Matters
- Give results in 15–30 minutes
- Cost less than PCR tests
- Don’t require labs or specialized equipment
- This means they can be used in small clinics, community centers, mobile vans, or remote areas, where lab testing isn’t practical.
However, it is important to note that rapid antigen tests are not replacement for PCR tests. They simply complement the PCR tests by allowing faster, on-the-spot decisions, especially when the lab capacity is limited.
What Makes It Essential Today?
Rapid antigen tests could help with spotting and stopping local outbreaks quickly, protecting high-risk people and healthcare workers, and staying prepared for future respiratory pandemics.
The WHO is also pushing for decentralized, quality-checked testing as part of universal healthcare and global health security, so countries aren’t caught unprepared when the next outbreak happens.
When Is It A Right Time To Get Yourself Checked For COVID-19?
If you notice these following symptoms as noted by the Centers for Disease Control and Prevention (CDC), it is best that you get yourself a COVID-19 test:
- Fever or chills
- Cough
- Shortness of breath or difficulty breathing
- Sore throat
- Congestion or runny nose
- New loss of taste or smell
- Fatigue
- Muscle or body aches
Singapore, UK and Canada Issue Health Advisory Over Delhi’s Air Pollution

Credits: iStock
As Delhi's air quality levels and pollution continues to worsen, and people struggle to breathe, countries like Singapore, the United Kingdom, and Canada issued advisories for their citizens travelling to the capital city. However, the capital city's crisis continues to remain ignore, though CM Rekha Gupta did hold a review meeting on the same on Monday, with a follow-up scheduled on Thursday.
Singapore Travel Advisory On Delhi's Air Pollution
Singapore High Commission issued an advisory, which stated:
On 13 December 2025: The Indian Central Pollution Control Board invoked Stage 4, the highest level, of the Graded Response Action Plan (GRAP) in the Delhi National Capital Region. Under GRAP 4, construction and industrial activities are heavily restricted, and schools and offices are encouraged to shift to hybrid format. The Delhi authorities have urged residents to stay indoors, especially children and those with respiratory or cardiac ailments, and to use masks if stepping out. In this regard, the High Commission urges Singapore nationals in the Delhi National Capital Region to pay heed to this advice.
We also note that given the low visibility, flights to and from the Delhi National Capital Region are likely to be affected. The Indira Gandhi International Airport and several airlines have issued advisories. Travellers should take note of this, and check with the respective airlines for updates.
UK And Canada Too Issue Advisories On Delhi Pollution And Its Impact On People
UK's Foreign, Commonwealth & Development Office (FCDO) warned that air pollution could lead to serious health threats for those living in northern India, especially between the months of October and February. The UK advisory also stressed on the health of pregnant women and people with any heart or respiratory. The advisory noted that they must seek medical advice before travelling to India.
The statement read: Children, the elderly and those with pre-existing medical conditions may be especially affected. If you’re pregnant or have a respiratory or heart condition you may wish to consult a medical practitioner before you travel.
Canada too issued a similar notice, advising, especially those who are already struggling with respiratory issues and to continuously monitor air quality levels. The notice also highlighted the pollution that is caused by fog and smoke trends that are increasing in urban areas like Delhi, especially during the winters.
The advisory read: Smoke haze and other types of air pollution can be extremely hazardous in urban areas and cities such as Delhi. It’s typically at its worst in winter. In rural areas, air quality can be affected by agricultural burning. Dust storms also occur across northern India. Monitor air pollution levels, which change quickly, especially if you suffer from respiratory ailments or have pre-existing medical conditions.
As of today, Delhi's air quality remained in "very poor" category, and the AQI stood at 342 at 8am, as per the Central Pollution Control Board. The 24-hour average AQI was logged at 412 under the "severe" category on Tuesday evening when Delhi's quality peaked to record the fourth severe air day in the month of December.
© 2024 Bennett, Coleman & Company Limited

