- Health Conditions A-Z
- Health & Wellness
- Nutrition
- Fitness
- Health News
- Ayurveda
- Videos
- Medicine A-Z
- Parenting
- Web Stories
Are Gen-Z And Millennials More Prone To Cancer? Yes, Says A Recent Study

Credits: Canva
Gen-Z and millennials are living at a time of historically high technical breakthroughs, information availability and chances for both career and personal development. However, this age is also accompanied by a worrisome increase in a number of health issues— particularly cancer.
The contrast between healthy lifestyles and the constant threat of this fatal illness highlights the urgent need for increased awareness and preventative healthcare interventions.
Worrisome Data
Recent research that was published in the Lancet Public Health reveals alarming patterns in the incidence of cancer in Americans of all ages. According to the study, there has been a noticeable increase in the incidence of 17 different cancer kinds.
For several of these cancers, people born in 1990 had 2-3 times higher rates than people born in 1955. This concerning rise emphasises how critical it is to comprehend the fundamental causes.
India’s Story: Not Too Different
Even though the data comes from the US, India's incidence is not all that different.
According to research from the Delhi State Cancer Institute (DSCI), colon cancer is now more common in adults between the ages of 31 and 40 rather than the elderly, over 50.
According to the National Centre for Disease Informatics and Research (ICMR-NCDIR), in 2022, the projected number of new cancer cases in India was 1,461,427, with a crude incidence rate of 100.4 per 100,000 individuals.
The ICMR-NCDIR estimates that one in nine Indians will be diagnosed with cancer at some point in their lives.
Changes To Keep Afloat: Causes And Cures
Cause #1: Smoking, drinking more alcohol, and consuming more processed foods can all raise the risk of cancer.
Cure: Eat a diet high in fruits, vegetables, and whole grains and well-balanced. Drink in moderation and abstain from smoking. A healthy weight can also be maintained with regular activity.
Cause #2: Sleep deprivation and irregular sleep schedules can throw off hormone balance and raise the risk of cancer.
Cure: Try to get seven to nine hours of good sleep every night. Make sure you follow proper sleep hygiene and have a regular sleep pattern.
Cause #3: Genetic alterations that raise the risk of cancer may be inherited by some millennials.
Cure: Genetic counselling and routine testing can assist in early risk identification. Consult a healthcare professional about family history to customise preventative care.
Cause #4: Cancer risk can be raised by extended periods of inactivity brought on by desk occupations and sedentary leisure pursuits.
Cure: Make exercise a regular part of your day. Try to get in at least 150 minutes a week of moderate exercise or 75 minutes of intense exercise.
Cause #5: Long-term stress and mental health problems might affect immune system performance and increase the risk of developing cancer.
Cure: Preventive measures include practising stress-reduction methods including yoga, meditation, and counselling. Make mental health a priority and, if necessary, seek professional assistance.
Some Other Preventative Techniques
- A nutritious diet should emphasise foods high in vitamins, minerals, and antioxidants.
- To preserve general health, partake in physical activity on a regular basis.
- For early detection, adhere to suggested screening protocols.
- Minimise your exposure to hazardous materials and environmental pollutants to prevent cancer.
RFK Jr. And Trump Cabinet Want Psychedelics To Be Legal After FDA Shut Down; What This Means For The Controversial Drug?

In a move that would have seemed unthinkable just a decade ago, a new presidential administration is placing psychedelics front and center in its health policy agenda. Health Secretary Robert F. Kennedy Jr. told Congress that psychedelic-assisted therapy—long stigmatized and sidelined—is on track for federal approval “within 12 months.”
That timeline stunned even long-time advocates. But it aligns with a wider political shift, not just in progressive strongholds but also in conservative territories like Texas. Former Trump officials including ex-Governor Rick Perry and Secretary of Veterans Affairs Doug Collins have expressed support for expanding access to psychedelics for treating PTSD, depression, and addiction.
The timing is no accident. The U.S. Food and Drug Administration (FDA) recently dealt a heavy blow to advocates by rejecting MDMA-assisted therapy for PTSD, citing concerns over research integrity. The decision was a major setback for the psychedelic movement—but it may also have sparked a political counter-response.
MDMA, also known as ecstasy, had long been the frontrunner in the race to integrate psychedelics into clinical medicine. The Multidisciplinary Association for Psychedelic Studies (MAPS), which backed MDMA research for decades, had hoped for a groundbreaking FDA approval this year.
Instead, FDA advisors voted overwhelmingly against it, criticizing data collection methods, researcher bias, and missing adverse event reports. One panelist described the trial environment as bordering on “cult-like.” Critics argued that while results appeared promising, the data lacked scientific rigor.
The agency hasn’t entirely shut the door on MDMA, but it's clear that any future approval will come with strict conditions—or require new clinical trials entirely.
Rather than retreating, psychedelic advocates now seem to be finding powerful allies. Kennedy’s endorsement of psychedelic therapies stems in part from personal experience—he’s spoken openly about family members and friends who found healing through these substances.
Meanwhile, Rick Perry and other Republican figures are pushing forward with state-level projects that bypass the slow-moving federal process. Texas recently approved $50 million to fund research into ibogaine, a powerful and controversial psychedelic derived from a West African plant.
Ibogaine remains a Schedule I substance, in the same legal category as heroin. But veterans and policymakers in Texas are betting on it to address the state’s opioid crisis and support those suffering from war-related trauma.
“It’s not just red states or blue states anymore—it’s veterans, families, people from across the spectrum who are saying: what we’re doing isn’t working,” said Bryan Hubbard, co-founder of Americans for Ibogaine.
What is The Ibogaine Experiment?
Ibogaine is not your typical psychedelic. While small studies suggest it may reset the brain’s reward system and break addictive cycles, it’s also known for severe side effects—including potentially lethal heart arrhythmias.
Veterans like Marcus Capone say it changed their lives. Capone, a former Navy SEAL, describes his first ibogaine experience as “a complete purge.” After years of therapy and medication, one session left him with “no more anxiety, no more depression.”
His nonprofit, VETS, has already sent over 1,000 veterans abroad for psychedelic treatment. But federal officials remain cautious. Former NIDA director Nora Volkow acknowledged ibogaine’s promise but warned it “would be dead in the water” for FDA approval in its current form due to toxicity risks.
Still, the National Institutes of Health is now supporting development of synthetic ibogaine analogs—evidence that even federal agencies are evolving.
Fast-Tracking Psychedelic Drug Approval—At What Cost?
FDA commissioner Marty Makary, who reports to RFK Jr., recently announced efforts to accelerate drug approvals that serve “American health interests.” One proposed framework could shrink the FDA’s review process from six months to just one.
Makary has also floated the idea of relaxing placebo-controlled trial requirements—controversial in psychedelic research because participants often know if they received the real drug. That change could open the door for faster results, but it also raises concerns about scientific integrity.
Critics like Yale psychiatrist Philip Corlett are sounding the alarm. “The public is ahead of the science right now,” he warns. “If RFK and others are serious, they should stick to the benchmarks of clinical research. Otherwise, this could backfire.”
What Happens to MDMA Now?
The future of MDMA therapy is uncertain. FDA regulators could override the advisory panel’s vote and approve the drug with new safeguards, such as risk evaluation and mitigation strategies (REMS). Another possibility: conditional approval with a requirement for post-market research.
But there’s also a chance the drug could be shelved, at least temporarily, while Lykos—the company behind the MDMA trials—regroups and launches a new study. That could delay approval by years.
“The hope was that if we did the science right, the data would speak for itself,” said trial investigator Ingmar Gorman. “But that’s not how it played out.”
The psychedelic renaissance now finds itself in a paradox: increasingly mainstream and bipartisan in political circles, but still fragile in the eyes of regulatory science.
States like Texas and Oregon are forging ahead. Veterans and nonprofits are doing the groundwork. And the federal government, under a high-profile and controversial health secretary, appears willing to fast-track approval processes but speed and politics won’t substitute for rigorous evidence. If the next wave of psychedelic approvals is rushed or mishandled, it could risk discrediting therapies that millions of patients might one day benefit from.
This Age-Old Killer Is Spreading Fast, Why Super Typhoid Isn’t Just A ‘Poor Country’ Problem Anymore
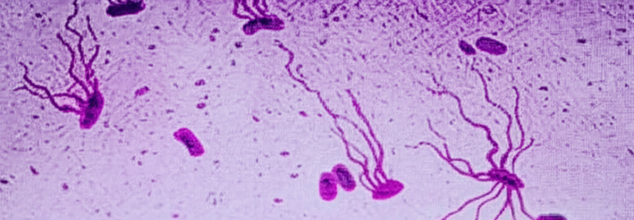
Representational
Typhoid fever is not the kind of illness most people in developed nations worry about. It's often written off as a disease of the past—something that plagued ancient societies before clean water systems and antibiotics. But here’s the thing: typhoid never went away. And now, it's evolving into something much more dangerous—something even modern medicine might not be able to stop.
A large genomic study published in The Lancet Microbe in 2022 has sounded the alarm. The bacterium responsible for typhoid, Salmonella enterica serovar Typhi (or S. Typhi), is rapidly acquiring resistance to nearly all antibiotics used to treat it. More disturbingly, strains resistant to multiple drug classes are spreading beyond their traditional strongholds in South Asia and appearing across continents—including in the United States, United Kingdom, and Canada.
This is no longer a regional concern. It’s a global one.
What is Super Typhoid?
The study involved sequencing over 3,400 S. Typhi strains collected between 2014 and 2019 from patients in India, Pakistan, Nepal, and Bangladesh. The results were stark. Not only were extensively drug-resistant (XDR) strains of typhoid rising rapidly, but they were also outcompeting and replacing less resistant versions.
XDR typhoid strains are already immune to several older antibiotics—ampicillin, chloramphenicol, and trimethoprim/sulfamethoxazole. But here’s where it gets worse: many are now developing resistance to newer and more potent drugs like fluoroquinolones and third-generation cephalosporins, which until recently were mainstays of typhoid treatment.
Even the last reliable oral antibiotic—azithromycin—is showing signs of failure. The study found emerging mutations that could potentially render azithromycin ineffective. These haven’t yet converged with XDR strains, but scientists warn that it’s only a matter of time. If that happens, oral treatment options could become entirely obsolete.
For now, South Asia remains the epicenter of the crisis, accounting for about 70% of the global typhoid burden. But this doesn’t mean the threat is contained.
Researchers tracked nearly 200 instances of international transmission since the 1990s, most involving travel or migration. Typhoid "superbugs" have been detected in Southeast Asia, East and Southern Africa, and in wealthy nations where the disease was thought to be virtually eradicated.
“The speed at which highly-resistant strains of S. Typhi have emerged and spread is a real cause for concern,” said Dr. Jason Andrews, an infectious disease specialist at Stanford University who co-authored the study.
Why Is Treatment Is Failing?
If antibiotics are failing, what’s next? For starters, prevention. Experts say the most immediate and scalable solution lies in typhoid conjugate vaccines (TCVs). These vaccines offer strong, long-lasting protection and are safe for children as young as six months old. But access is patchy.
Pakistan became the first country to introduce TCV into its national immunization program in 2019—an urgent response to the first major outbreak of XDR typhoid that hit its population. Since then, the move has become a case study in how vaccination can cut off the disease at its roots.
India, Bangladesh, and Nepal have followed suit with pilot programs and localized rollouts, but global coverage remains far too low. Meanwhile, high-income countries have not prioritized TCV access at all, largely because typhoid isn’t seen as a domestic threat.
Antibiotic Resistance Crisis at Large
This typhoid crisis isn’t an isolated story. It’s part of a larger, systemic problem: antibiotic resistance is now one of the top global causes of death. A 2019 study published in The Lancet estimated that antimicrobial resistance was directly responsible for 1.27 million deaths worldwide, surpassing HIV/AIDS and malaria.
Typhoid is just the latest face of that threat. If azithromycin fails, intravenous treatments will be the only remaining option. This is not sustainable for low-resource settings, where typhoid is most rampant.
And as the S. Typhi genome continues to adapt, the search for novel antibiotics becomes more urgent but the global antibiotic pipeline is worryingly dry. Very few new drugs are being developed, and those that are rarely target neglected tropical diseases like typhoid.
How Globalization Makes It Everyone’s Problem?
COVID-19 reminded us how quickly a localized health threat can go global. Typhoid is no different. The bacteria travel with people—through tourism, immigration, and international trade.
The difference is: we already have tools to stop this. TCVs work. Better sanitation and access to clean water help. Public health messaging and travel guidelines can make a difference. But we’re not moving fast enough.
A recent Indian study estimated that vaccinating children in urban areas could reduce typhoid cases and deaths by up to 36 percent. That’s a significant dent—especially when combined with infrastructure upgrades and careful antibiotic stewardship.
What Happens If We Do Nothing?
If left unchecked, drug-resistant typhoid could become nearly impossible to treat in outpatient settings. That means more hospitalizations, more strain on health systems, more deaths—particularly among children in developing nations.
With around 11 million cases of typhoid annually, even a small increase in resistance could tip the balance into a major health crisis.
And if XDR strains gain resistance to azithromycin, we will be left with zero effective oral drugs, none. The path forward is clear—and urgent. Here’s what needs to happen:
- Expand global access to typhoid conjugate vaccines, especially in endemic regions.
- Invest in next-generation antibiotics that target typhoid and other neglected infections.
- Implement stricter regulations on antibiotic use in agriculture and medicine.
- Strengthen global surveillance systems to detect resistant strains early and contain outbreaks.
- Raise awareness that typhoid is not just a problem for the developing world.
Antibiotic resistance isn’t science fiction. It’s a biological reality. And typhoid is just one example of how quickly things can unravel when we underestimate an ancient enemy.
We can still turn the tide but only if we act with urgency and coordination. The warning signs are flashing red. Typhoid isn’t gone. It’s evolving. And this time, it may be deadlier than ever.
1 In 4 Indian Couples Are Overweight, Finds ICMR; How Obesity Is Now Becoming A Relationship Problem?

Credits: Canva
Obesity is no longer just a health issue, it is increasingly becoming a social phenomenon and a lifestyle disease. A recent study published in Current Developments in Nutrition, led by the Indian Council of Medical Research (ICMR) has found that 27.4% of Indian married couples share similar overweight or obese status.
Analyzing data from over 52,000 married couples across India using the National Family Health Survey (NFHS-5, 2019–21), the study points to a troubling pattern- in wealthier, urban households, especially among young couples, there is a significantly higher risk of both partners becoming overweight or obese. At its core, this research uncovers how daily habits, routines, and food choices within marriages are driving a quiet but dangerous health trend across the country.
Are Shared Habits A Risk Factor for Married Couples?
Unlike genetically linked conditions, obesity in married couples cannot be attributed to shared biology. So how does this mirroring occur? It is in environmental exposure, mutual behaviors, socio-economic context, and emotional co-regulation.
According to lead researcher Dr. Prashant Kumar Singh of ICMR’s National Institute of Cancer Prevention and Research, spousal similarities in health outcomes ranging from obesity and hypertension to smoking and sedentary behavior stem from shared lifestyles. These include eating patterns, physical activity (or lack thereof), screen time, media consumption, and stress management. Over time, habits converge especially in nuclear families with fewer social checks and less structured meal routines.
The study found that urban couples had a 38.4% concordance rate, significantly higher than rural couples (22.1%). Among the wealthiest households, this figure jumped to 47.6%, compared to only 10.2% in the poorest.
Where Obesity in Couples Is Rising Fastest In India?
Geographic disparities highlight how development and affluence correlate with rising obesity. States and territories with the highest spousal obesity concordance include:
- Kerala (51.3%)
- Jammu & Kashmir (48.5%)
- Manipur (47.9%)
- Delhi (47.1%)
- Goa (45.0%)
- Tamil Nadu (42.7%)
- Punjab (42.5%)
By contrast, states in eastern and northeastern India—where economic development is slower—showed much lower concordance rates, typically ranging from 19% to 22%.
“These figures underscore India’s uneven nutrition transition,” explains Dr. Shalini Singh, senior co-author of the study. “In wealthier regions, processed food consumption and reduced physical activity are becoming the norm. Marriage and cohabitation intensify these shared exposures, turning households into hotbeds of metabolic dysfunction.”
Is This A Disturbing Trend Among Under-30 Couples?
Perhaps the most concerning revelation is the early onset of weight gain in young couples. The study shows particularly high obesity concordance in couples under the age of 30, especially in Kerala (42.8%), Goa (37%), Jammu & Kashmir (31.6%), and Tamil Nadu (29.6%).
“This trend is alarming because early obesity increases the lifetime risk of chronic conditions like type 2 diabetes, cardiovascular disease, PCOS, and metabolic syndrome,” says Dr. Singh. “We’re seeing the impact of lifestyle-driven diseases unfold during what should be the most productive and healthiest years of life.”
The study also examined behavioral patterns that reinforce spousal weight concordance. For instance, 32.8% of couples reported regular television watching, while 39.6% reported newspaper reading, both indicative of sedentary behavior. Dependence on processed and ultra-processed food, especially in nuclear households, was another major contributor.
Interestingly, couples with similar education levels (about 45.2%) showed higher obesity concordance (31.4%), likely due to aligned food preferences, media consumption, and leisure routines.
The type of family structure also mattered. Nuclear families had a 28.9% concordance rate, higher than the 25.9% seen in joint families, where shared responsibilities and traditional food habits often foster more physical activity and balanced meals.
This Indian data fits into a much broader global trend. According to the World Obesity Atlas 2022, over 2.5 billion adults (43% of the global population) were overweight, and 890 million (16%) were obese. The burden of obesity now surpasses many infectious diseases and contributes to over 160 million years of healthy life lost annually due to comorbidities like heart disease, stroke, sleep apnea, and several cancers.
In India alone, obesity rates among adults are expected to climb significantly by 2040—27.4% of women and 30.5% of men, up from roughly 24% in 2021. If the patterns observed in married couples hold, these numbers could surge even faster than projected.
The study calls for a paradigm shift in how health interventions are designed. Rather than focusing on individuals, researchers urge a couple-based or household-level approach that takes into account the social dynamics of behavior change.
“Obesity is socially transmissible,” Dr. Singh emphasizes. “So the solution must also be social. Targeted public health messaging, fitness programs designed for couples, dietary counseling for families, and insurance incentives for preventive care at the household level are the need of the hour.”
Additionally, there’s a need to engage urban, affluent, and media-exposed demographics—who are often the earliest adopters of fast food, sedentary habits, and digital lifestyles—with interventions that feel relevant, aspirational, and sustainable.
As global health systems grapple with the rising burden of noncommunicable diseases, the Indian study offers a crucial insight: marriage can amplify risk—but also holds the key to prevention. By targeting couples early and acknowledging the influence of shared environments, public health systems can make strides in reversing obesity trends.
© 2024 Bennett, Coleman & Company Limited

