- Health Conditions A-Z
- Health & Wellness
- Nutrition
- Fitness
- Health News
- Ayurveda
- Videos
- Medicine A-Z
- Parenting
- Web Stories
Autism May Be 14 Times More Likely with This Hidden Condition

A new study has revealed an unexpected link between autism and a rare genetic disorder, shedding new light on the causes of autism spectrum disorder (ASD). Scientists have discovered that people with myotonic dystrophy type 1 (DM1) — a rare, inherited neuromuscular disorder — are 14 times more likely to develop autism than the general population.
While autism touches an estimated 7 million Americans, DM1 touches about 140,000, making it far less common. Nevertheless, the discoveries are revolutionizing how scientists think about the genetic structure of autism and revealing possible biological mechanisms that could drive its development.
What Is Genetic Condition Called?
DM1 is an inherited disorder where muscles become weak and progressively lose their strength, muscles tire easily, there are uncontrollable movements of the face or limbs, and there is cognitive impairment. It is a result of DMPK gene mutation where the gene function is compromised by tandem repeat expansions (TREs), which are repetitions of DNA. This generates poisonous RNA that then interferes with the capacity of the body to synthesize crucial proteins in the muscles and the brain.
What is so worrisome about this disorder in the case of autism is that it has an effect on neural development and gene expression within the brain. DM1 may change the way the brain develops connections early in life — an age when developing communication skills, social behavior, and learning habits is most important, all of which are frequently affected in those with autism.
Genetic Insights: Connecting the Dots Between DM1 and Autism
In a comprehensive research conducted by the University of Nevada Las Vegas (UNLV) and published in Nature Neuroscience, scientists compared RNA in 38 sets of genes from people with and without autism. RNA is crucial in gene expression for enabling DNA instructions to be translated into functioning proteins.
The researchers found that when the DMPK gene experiences tandem repeat expansion, the resulting RNA abnormally binds to proteins essential for the splicing of genes — an important process for gene function in brain development. The misbinding depletes proteins and triggers a cascading effect of mis-spliced genes, the majority of which contribute to regulating brain function and development.
This is a new paradigm for how to think about the genetic landscape of autism," said Dr. Ryan Yuen, senior scientist at the Hospital for Sick Children and author of the study. "We now understand that defective RNA has the ability to behave like a sponge, attracting away vital proteins necessary for proper brain development. This may be the reason why DM1 has a connection to the social, behavioral symptoms we identify with ASD."
What is Tandem Repeat Expansions (TREs)?
TREs happen when DNA sections repeat more times than usual, leading to the risk of genetic mistakes. TREs are now found to happen more frequently in people with autism, with previous research by Dr. Yuen that found over 2,500 sites in the genome where TREs disproportionately occurred in ASD-diagnosed individuals.
In DM1, the increased repeats in the DMPK gene disrupt protein regulation throughout the genome. This interference not only leads to muscle weakness and heart disease but also potentially underlies some of the neurological features seen in autism — including repetitive behavior, poor coordination, and sensory sensitivities.
Perhaps the most thrilling implication of this breakthrough is its potential for targeted therapies. Scientists are now investigating how to restore protein balance by either releasing bound toxic RNA-bound proteins or reintroducing critical proteins into the genome. These approaches could lead to precision medicine that targets the genetic dysfunctions underlying both DM1 and ASD directly.
"By knowing the specific molecular pathways that are affected, we can start to create therapies that are really personalized," Dr. Yuen said. "It's no longer about treating autism symptoms—it's about fixing the underlying causes."
As the genetic link between DM1 and autism continues to unravel, yet another recent Chinese study is bringing hope in the guise of a non-surgical brain stimulation method called transcranial pulsed current stimulation (tPCS).
It's a therapy that uses electrodes placed on the scalp to deliver mild electrical impulses into target areas of the brain. In a 20-session trial with children between ages 3 and 14, the ones who got tPCS for four weeks improved significantly in sleep, language, sensory responsiveness, and social interaction. While still in the experimental stage, it promises that brain modulation technology could supplement genetic treatments for ASD in the future.
The sense of urgency is also heightened by the newest CDC statistics, which say that 1 in 31 children in the U.S. is now diagnosed with autism a rate that has skyrocketed from 1 in 150 in the early 2000s. Although some attribute the increase to improved screening and awareness, others think that environmental toxins, including exposure to pesticides, food additives, or too many ultrasound scans, could be playing a role.
Whatever the reason, what's certain is that autism is no longer an either-or condition that can be treated with blanket solutions. The connection between DM1 and ASD has made it necessary for all diagnostics and therapies to be based on the most advanced genetic knowledge.
Soccer Player 'Choclo' Suffered A Type 3A Muscle Injury Causing His Absence From Match Against Delfín
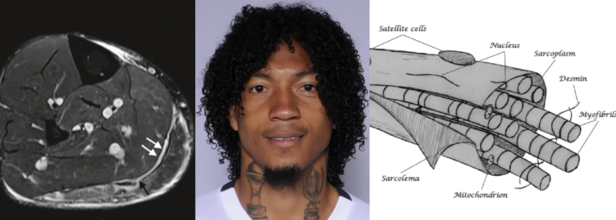
Source and in photos L to R: Minor, structural muscle injury (type 3a), source: SEMS Journal; player Choclo (source: LDU Quito); diagram of the muscle fiber, source: SEMS Journal
Liga Deportiva Univerrsitaria (LDU) has confirmed a new injury to its roster this Sunday. Defender José "Choclo" Quintero has a grade 3A muscle injury. This has been confirmed by team's official statement which has come from the club's medical department.
The player is currently undergoing rehabilitation and will begin strength training and physical therapy sessions. The official statement says that "Choclo" will have a reasonable amount of time before he returns to the field. He has so far played 19 matches and his return will depend on his progress.
José "Choclo" Qiuntero List Of Injuries
He had earlier suffered a skull fracture from August 30 2021 to October 4 2021 and as a result had missed three games in the season 21/22. Previously too in the season 16/17, he was in rehabilitation for 173 days due to a knew medial ligament tear, as a result of which he missed 31 games.
Also Read: Inner Child: Being Left Out And Rejected In Childhood Becomes A Social Seed For Deeper Connections
What Is a A 3A Muscle Injury?
As per the 2014 study published in Translational Medicine @ UniSa, Official Journal of the Medical School of the University of Salerno, a 3A muscle injury is part of the structural injuries, which are divided into 3 sub-groups as per the "entity of the lesion within the muscle".
A type 3A lesion is a minor partial lesion, which involves one or more primary fascicles within a secondary bundle.
3A Muscle Injury Symptoms
It usually is characterized by sharp pain, especially during a specific movement. The pain is, however, localized, and is easy to "appreciate on palpation and, at times, preceded by a snap sensation. On palpitation, it is not possible to detect the structural defect as it is too small and the contraction against manual resistance is painful," notes the study.
3A Muscle Injury Diagnosis
Another study from 2016, published in the journal Joints, a 3A involves a minor partial muscle tear with small maximum diameter and could be detected through MRI that shows fiber disruption.
A 2019 study published in the journal Sport and Exercise Medicine Switzerland, notes that Type 3A are of less than 5mm in size. Thus, it includes 1-5 primary muscle bundles. The study also notes that such injuries usually heal without defect, however, injury to the perimysium and the aponeurosis is found in type 3b injuries (> 5 mm), which is the cause for intermuscular hematoma formation.
Also Read: What Is Innotox? The ‘Korean Botox’ People Are Injecting At Home—And Why Doctors Are Worried
What Are The Common Muscle Injuries Among Football Players?
Type 3B injuries are moderate partial lesion, which involves at least a secondary bundle, with less than 50% of breakage surface. A Type 4 lesion is a sub-total tear with more than 50% of breakage surface or even a complete tear of the muscle. It also involves the muscle belly or the musculotendinous junction.
While these comprise structural injuries, Type 1 and Type 2 comprise the non-structural injuries.
It is the non-structural injuries, which are the most common and accounts for 70% of all muscle injuries in football players, mentions the 2014 study.
While the lesion may not be readily recognized in these injuries, they cause more than 50% of days of absence away from sport matches and training, the study notes. When they are ignored, they could turn into structural injuries.
Non-structural muscle injuries are classified into different types based on their underlying causes. Here's a breakdown of common types and what triggers them:
Type 1A Injury
These injuries are often the result of fatigue or sudden changes in training routines, running surfaces, or high-intensity activities. The muscle strain occurs due to the body not being fully adapted to new or excessive demands.
Type 1B Injury
This type of injury is linked to prolonged and excessive eccentric muscle contractions — when the muscle lengthens while under tension. This repeated strain can lead to overuse and damage.
Type 2A Injury
Type 2A injuries are typically associated with spinal issues. Often misdiagnosed, they stem from minor intervertebral disorders that irritate spinal nerves. This nerve irritation disrupts the normal control of muscle tone in specific “target” muscles. In such cases, treating the underlying spinal disorder becomes the main focus of care.
Type 2B Injury
These injuries are caused by a breakdown in the balance of the neuro-musculoskeletal system, particularly the mutual inhibition mechanism controlled by muscle spindles. When this balance is disrupted, the regulation of muscle tone suffers. Specifically, when the inhibition of agonist muscles is reduced, those muscles may become overly contracted to compensate — leading to dysfunction and injury.
You Don’t Have To Smoke To Get Lung Cancer—Air Pollution May Be Just As Dangerous

Credits: Canva
For decades, lung cancer has been synonymous with smoking. But the data is shifting—and fast. Today, 10–20% of lung cancer cases in the U.S. are found in people who have never smoked a single cigarette. A new large-scale international study has now unearthed some of the strongest evidence yet that air pollution may be a major culprit—and it’s leaving a genetic trail behind.
Researchers have discovered that fine particulate matter in polluted air, commonly from traffic, industrial emissions, and smog, is strongly associated with DNA mutations that are also found in smokers’ lung tumors. These mutations may be key drivers of lung cancer development in never-smokers.
The research, involving whole-genome sequencing of lung tumors from 871 never-smokers across 28 regions in four continents, found that individuals living in highly polluted environments had significantly more driver mutations—the kind that directly trigger cancer.
The investigators matched tumor samples with long-term air pollution exposure estimates, using ground and satellite data for fine particulate matter (PM2.5). They found that non-smokers exposed to high levels of pollution were nearly four times more likely to exhibit the SBS4 mutational signature—a genetic fingerprint commonly linked to tobacco smoke.
Additionally, they identified a 76% increase in a separate signature associated with accelerated biological aging. This is alarming, considering these were individuals with no direct tobacco exposure.
What makes this finding even more significant is that researchers discovered TP53 and EGFR mutations—both known to be aggressive lung cancer markers—more frequently in people living in polluted areas. These genetic changes are typically hallmarks of cancers in smokers.
This implies that air pollution could be triggering similar molecular pathways to those activated by cigarette smoke.
But there was a twist: a new mutational signature, SBS40a, was found in 28% of never-smokers but not in smokers. The origin of this marker remains unclear, but it suggests that pollution may not be the only hidden risk.
Rise of Environmental Carcinogens
The study adds to a growing body of evidence that air pollution is not just an irritant—it’s a carcinogen. Fine particles can be inhaled deep into the lungs, where they may damage DNA directly or trigger chronic inflammation that promotes tumor growth.
Even more surprising, another carcinogen showed up in the data: aristolochic acid, found in some traditional Chinese herbal remedies. This compound was associated with a distinct mutational signature in patients from Taiwan, hinting at a possible secondary environmental risk factor for lung cancer in never-smokers.
The rise of lung cancer in non-smokers is especially noticeable in East Asia, where rates remain disproportionately high—particularly among women. While genetic predisposition may play a role, this new evidence points clearly to environmental exposures as a key contributor.
And it’s not just an Asian problem. In Western countries, urban dwellers are also exposed to dangerously high levels of air pollution. The World Health Organization estimates that 99% of the world’s population breathes air that exceeds safe pollution thresholds. This means the risk is truly global.
The power of this new research lies in its use of whole-genome sequencing to link pollution to DNA changes. These mutational signatures act as a kind of molecular journal, recording every environmental insult a cell has endured.
The ability to map those changes and match them to known pollutants gives researchers a more precise way to trace cancer origins—not just infer them from epidemiological studies.
While this study can’t definitively prove causation, the strong correlation between pollution exposure and cancer-driving mutations makes it clear that dirty air is more than just a nuisance—it's a potential trigger for deadly disease.
Researchers acknowledge some limitations. Pollution estimates were regional, not personal, meaning it’s unclear how much exposure each participant had. Self-reported smoking histories can also be unreliable.
Still, the pattern is unmistakable. Air pollution behaves like a mutagen, leaving behind signatures that align with known cancer mechanisms. And it appears to affect never-smokers in a strikingly similar fashion to tobacco users—down to the very DNA damage.
This study raises serious public health questions: If environmental exposure to polluted air can cause DNA mutations tied to cancer, what safeguards are in place to protect those most vulnerable?
Governments and public health agencies may need to reconsider air quality regulations, urban zoning, and access to clean air—especially in densely populated cities where pollution levels remain dangerously high.
Healthcare systems might also need to adapt. Traditional lung cancer screenings focus on long-time smokers, but this research could shift how we think about early detection in non-smokers, especially those living in high-risk environments.
Lung cancer has long been viewed through the lens of personal responsibility: if you smoked, you knew the risks. But this research changes that narrative. The air we breathe—something no one can fully avoid—is now emerging as a significant threat.
For non-smokers around the world, especially women and urban residents, this is a wake-up call. Your lungs may be at risk not because of personal choices, but because of public ones—decisions about pollution control, urban planning, and clean energy.
The future of lung cancer prevention may lie not just in quitting cigarettes, but in cleaning up the air we all share.
Scientists Have Developed An AI Model To Help Predict Sudden Cardiac Risks 'Most Doctors Can't See'
Credits: Canva
Every year, thousands of seemingly healthy people—often young, active, and without obvious warning signs—die suddenly due to cardiac arrest. For decades, doctors have struggled to reliably identify which patients with heart conditions are at high risk and who might be unnecessarily undergoing invasive interventions. That may be about to change.
In a breakthrough that could transform how we predict—and prevent—sudden cardiac death, scientists at Johns Hopkins University have developed an artificial intelligence model that vastly outperforms current clinical standards in identifying people most at risk. Their new system, known as MAARS (Multimodal AI for Arrhythmia Risk Stratification), not only forecasts risk with up to 93% accuracy in vulnerable age groups, but also explains why someone is high risk—something most algorithms fail to do.
The focus of the study is hypertrophic cardiomyopathy (HCM), one of the most common inherited heart conditions. It affects around 1 in 200 to 500 people globally and is a leading cause of sudden cardiac death in athletes and young adults. While most individuals with HCM live normal lives, a subset is at high risk for lethal arrhythmias—heart rhythm disturbances that can cause the heart to stop without warning. And here’s the catch: right now, doctors only have a 50-50 shot at predicting who will be affected.
“Currently we have patients dying in the prime of their life because they aren’t protected,” said Dr. Natalia Trayanova, senior author of the study and a leading figure in AI cardiology research. “And others are putting up with defibrillators for the rest of their lives with no benefit.”
Trayanova is referring to implantable cardioverter defibrillators (ICDs)—tiny devices inserted into the chest that deliver electric shocks to correct abnormal heart rhythms. They save lives in the right patients but come with physical, emotional, and financial burdens when used unnecessarily.
The need for a more precise, personalized tool has never been greater.
What the AI Model Does Differently?
Published in Nature Cardiovascular Research, the new model represents a significant departure from traditional clinical guidelines used across the US and Europe.
MAARS doesn’t rely on a single data source. Instead, it analyzes a multimodal spectrum of information—ranging from electronic health records and patient histories to contrast-enhanced cardiac MRI images that reveal scarring, or fibrosis, within the heart.
Scarring is a key factor in determining sudden death risk in HCM. But interpreting these raw images is extremely challenging for even seasoned cardiologists. That’s where AI has the edge.
“People have not used deep learning on those images,” Trayanova explained. “We are able to extract this hidden information in the images that is not usually accounted for.”
The AI essentially spots dangerous patterns in the heart’s scar tissue that the human eye—and even conventional software—can’t see.
How Accurate Is It?
In clinical tests involving real-world patients from Johns Hopkins Hospital and Sanger Heart & Vascular Institute in North Carolina, the results were staggering:
- Traditional clinical guidelines correctly predicted sudden cardiac death risk only 50% of the time.
- The MAARS model achieved an overall accuracy of 89%.
- In patients aged 40 to 60—a group particularly vulnerable to undetected risk—the model was 93% accurate.
What makes this even more valuable is its ability to provide explanations. The system doesn't just say "this patient is high risk"—it breaks down the why, giving cardiologists critical information to tailor treatment plans.
“This significantly enhances our ability to predict those at highest risk compared to our current algorithms,” said co-author Dr. Jonathan Crispin, a Johns Hopkins cardiologist. “It has the power to transform clinical care.”
Why This Could Be Transformative?
MAARS isn't the first AI model from Trayanova’s lab. In 2022, her team built another tool that provided survival predictions for patients with prior heart attacks, known as infarcts. But this latest model breaks new ground by tackling one of the most elusive forms of cardiac risk—arrhythmias caused by scarring in inherited heart conditions. The potential benefits are wide-ranging:
- Lives saved by identifying at-risk patients who might otherwise be missed.
- Better quality of life for patients who avoid unnecessary ICD implantation.
- More personalized treatment plans based on detailed, AI-generated insight.
Importantly, the model was trained and validated across diverse demographics, showing consistent performance regardless of age, gender, or ethnicity.
The researchers aren’t stopping here. They plan to expand MAARS to include other forms of arrhythmia-related heart diseases, such as cardiac sarcoidosis and arrhythmogenic right ventricular cardiomyopathy—conditions that also carry a high risk of sudden death but suffer from diagnostic ambiguity.
They’re also working to test the model in larger, more varied populations to move it closer to clinical adoption.
A New Era in Cardiology?
Artificial intelligence has long been hyped as the future of medicine. But MAARS is more than hype—it’s a working proof of concept that shows how deep learning can complement medical expertise, not replace it.
AI may soon become your cardiologist’s most powerful diagnostic tool—one that sees what even the best-trained human eyes might miss. And when lives are on the line, that kind of clarity could mean everything.
© 2024 Bennett, Coleman & Company Limited

