- Health Conditions A-Z
- Health & Wellness
- Nutrition
- Fitness
- Health News
- Ayurveda
- Videos
- Medicine A-Z
- Parenting
- Web Stories
Can Potatoes Help Control Obesity? Researchers Say Yes; Know Why, How and More

Long seen as the enemy of healthy diets and weight loss plans, the humble potato may be getting a new lease of life, this time, as a key ingredient in fighting obesity. Kolkata researchers have found a way to turn starchy potatoes into a powerful dietary ally. At the Food Technology and Science Institute (FTSI), under TCG CREST, scientists have devised a method to convert potato starch into high-functioning dietary fibre. This fibre is designed to improve gut health and support weight management.
According to the team, the fibre works as a prebiotic, feeding the gut’s existing good bacteria and helping them thrive, an essential part of maintaining digestion, metabolism, and overall wellness.
Challenging the Potato’s Bad Reputation
Potatoes have long been excluded from weight-loss diets, blamed for belly fat and seen as calorie-dense comfort food. But the development out of FTSI challenges this narrative. The innovation arrives at a time when demand for functional foods is booming in India, with consumers increasingly seeking clean-label, plant-based, and gut-friendly options.
“Much of the core fibre ingredients like inulin, FOS, GOS, and glucans are still imported, mainly from China,” said Prof. Parthasarathi Bhattacharya, Head of FTSI. “That has created concerns around pricing, quality control, and long-term supply.”
Also Read: Eating More Ultra-Processed Foods Linked to 41% Higher Lung Cancer Risk, Study
India’s Potato Surplus Finds New Purpose
India harvested more than 60 million tonnes of potatoes in the 2024–25 crop year, making it the second-largest producer in the world. A significant portion of this crop ends up in surplus.
The key lies in a proprietary enzyme developed by the institute. This enzyme can convert starch from potatoes or other carbohydrate-rich crops into dietary fibre.
“We’re using what India already grows in abundance and giving it a new role,” said Prof. Bhattacharya.
Potatoes as the Future of Functional Snacking
Plans are already underway to integrate this fibre into a range of everyday food products. These include vegan ice creams made from potato “milk”, gummies, protein-rich cones, and high-protein snack bars. Designed to appeal to urban consumers, these products aim to provide indulgent snacking experiences without compromising on health goals.
This trend marks a larger consumer shift, from isolated supplements to functional foods that naturally support wellbeing. Unlike probiotics, which involve introducing live bacteria into the body, prebiotics like potato fibre simply nourish the good microbes already present in the gut, making them easier to incorporate into daily diets.
Beyond potato fibre, the team at FTSI is also working on a range of other innovations such as prebiotic gummies, fungi-based proteins, and preliminary research on postbiotics. The overarching goal remains the same: to create functional food ingredients that are rooted in Indian crops and traditional food practices.
With increasing awareness around health and a growing emphasis on ingredient security, the potato, long vilified in diet culture, could be poised for a comeback. This time, not as a source of guilt, but as a scientifically backed, fibre-rich, gut-friendly food that supports weight control and overall wellness.
With Nearly 5,000 Active Cases Of This Deadly Virus, CDC Considers Travel Warning For China

Credits: Canva
The US Centers for Disease Control and Prevention (CDC) is considering a travel advisory for China, following a sharp and unexpected outbreak of chikungunya virus, a mosquito-borne illness known for causing severe joint pain and long-term complications. With nearly 5,000 confirmed cases in China—most centered in the densely populated Guangdong Province the outbreak is drawing concern not only for its scope but also for its potential to spread far beyond Chinese borders.
For global travelers and health officials alike, the news echoes the early days of COVID-19, when regional outbreaks quickly became international crises. Now, as the WHO calls for urgent action, the spotlight returns to international coordination, vector control, and public health preparedness.
The current outbreak began on July 8, with a single imported case reported in Foshan’s Shunde district. Since then, cases have exploded Foshan alone now reports over 5,155 infections, prompting the city to elevate its public health emergency response to Level III, denoting a “relatively major” event in China’s four-tier alert system.
The spread has not been confined to Guangdong. The European Centre for Disease Prevention and Control reports that over 240,000 chikungunya cases have emerged across at least 16 countries this year, with 90 related deaths globally.
According to Diana Rojas Alvarez, medical officer at the WHO, one key factor is viral adaptation. Since 2004, chikungunya has evolved to spread more efficiently, particularly through urban-adapted mosquitoes that thrive in warm, humid cities with poor water management.
Alvarez warns that 5.6 billion people in 119 countries now live in regions at risk of chikungunya outbreaks.
That’s not just a developing-world problem. The Aedes mosquito has already been spotted in parts of the southern United States, including Florida, Texas, and Louisiana making travel-related cases a direct risk to US public health.
What Is China Doing To Curb The Outbreak?
In a blend of traditional vector control and innovative science, China has deployed extraordinary measures to curb the outbreak:
- Mass mosquito eradication programs, including spraying and habitat destruction
- Drones to detect standing water on rooftops
- Larva-eating fish released into lakes and ponds
- Public advisories encouraging residents to eliminate breeding grounds
But the most headline-grabbing strategy? Elephant mosquitoes.
First identified in Tanzania in 1952, chikungunya is not new—but its aggressive resurgence in recent years has alarmed epidemiologists. The virus is transmitted primarily through the Aedes aegypti mosquito, which also spreads dengue, Zika, and yellow fever. Infected individuals can experience:
- Sudden onset of fever
- Severe joint pain (often debilitating and long-lasting)
- Muscle aches, headaches, joint swelling
- In some cases, vomiting or rash
Though rarely fatal, chikungunya can cause long-term disability, particularly in older adults or those with preexisting conditions. There is no antiviral treatment or vaccine, making prevention and early containment vital.
These oversized insects, known scientifically as Toxorhynchites splendens, are natural predators of Aedes mosquitoes. Released by a research team at Sun Yat-sen University’s Zhongshan School of Medicine, these giant mosquitoes do not bite humans, but their larvae feast on the mosquito species responsible for spreading chikungunya.
This approach, while unconventional, highlights the urgency and scale of the threat China is facing.
Prevention Measures to Pick From COVID-19 Playbook
The outbreak has prompted Chinese authorities to revive some of the pandemic-era containment strategies that became familiar worldwide:
- Mass PCR testing
- Isolation protocols for infected individuals
- Disinfection campaigns across neighborhoods
Designated hospitals with isolation beds have been set up in affected regions, and border control checks have been reinforced in Hong Kong to prevent imported cases.
The CDC has stated that it is closely monitoring the outbreak and may issue a Level 1 or Level 2 travel health notice. These advisories typically urge travelers to take extra precautions, such as using insect repellent, wearing protective clothing, and avoiding peak mosquito hours, especially in tropical or subtropical zones.
The US currently has no reported local transmission of chikungunya, but imported cases have occurred before, particularly in travelers returning from South Asia or the Caribbean. Public health experts warn that now is the time for vigilance, not complacency.
What Travelers Need to Know?
If you're planning a trip to China or anywhere with ongoing mosquito-borne virus activity—consider these guidelines:
- Use EPA-registered insect repellent with DEET or Picaridin.
- Sleep under mosquito nets, especially in areas with poor indoor mosquito control.
- Wear long sleeves and pants to reduce skin exposure.
- Monitor local health advisories and avoid travel to outbreak hotspots, especially if pregnant or immunocompromised.
The chikungunya outbreak in China is not just a national issue, it’s a global health stress test. With memories of COVID-19 still fresh, this sudden surge is a reminder that climate change, globalization, and urbanization are combining to amplify infectious disease risks.
If the US does issue a formal travel advisory, it will mark another chapter in the growing tension between health security and international mobility.
Had COVID? Your Next Flu Could Reactivate Dormant Breast Cancer Cells, Researchers Warn
Credits: Canva
Breast cancer survivors have lived with a guarded sense of relief. Even after beating the disease, the possibility of recurrence remains a faint shadow but new research has raised an alarming possibility- respiratory viruses, including common ones like influenza and SARS-CoV-2, may act as a catalyst, reawakening dormant breast cancer cells that linger quietly in the lungs long after remission.
In a new study published in Nature, researchers from the University of Colorado and Utrecht University have found that viral infections can reignite cancer’s flame literally. Dormant cancer cells are like the embers left in an abandoned campfire, and respiratory viruses are like a strong wind that reignites the flames.
This study marks a crucial turning point in how we understand long-term remission and highlights the importance of continued vigilance among cancer survivors.
Why COVID-19 Infection Is First Red Flag?
The investigation kicked off in the aftermath of the COVID-19 pandemic. Clinicians and researchers began to notice an uptick in metastatic cancer cases, especially among individuals previously in remission. Something wasn’t adding up. Cancer recurrences were occurring at an unusual rate and too often to be dismissed as coincidence.
The researchers turned to two key data sources: the UK Biobank and a large U.S. breast cancer database with over 37,000 patient records. In the UK Biobank cohort, survivors who had contracted COVID-19 exhibited a twofold increase in cancer-related mortality. In the U.S. dataset, those with prior SARS-CoV-2 infection faced a more than 40% increase in metastatic breast cancer, particularly in the lungs.
The extent of this increased risk is almost unheard of in cancer epidemiology, it’s a significant effect.
What’s Happening in the Body?
To understand the mechanics, the researchers turned to mouse models—long used as reliable proxies for studying human disease behavior. When the mice with previously dormant breast cancer cells were infected with either SARS-CoV-2 or influenza A, it took only days for those latent cells to wake up. Within two weeks, there was a more than 100-fold increase in metastatic tumor burden in the lungs.
Here’s the crucial insight, the cancer cells didn’t reawaken because the virus directly interacted with them. Instead, the viruses triggered an inflammatory immune response, rich in signaling proteins called cytokines—especially interleukin-6 (IL-6). This cytokine storm appeared to create an environment ripe for dormant cancer cells to start proliferating again.
According to lead researcher Shi Chia from the University of Colorado, “Although species differences warrant caution in interpreting mouse data… collectively, these findings underscore the substantial metastatic risk COVID-19 posed to cancer survivors.”
Role of Viruses in Cancer Biology
The link between viruses and cancer isn’t new. Human papillomavirus (HPV) has long been known to cause cervical and other cancers. The Epstein-Barr virus (EBV) has been implicated in several types of lymphoma. In fact, EBV has been found in five times higher concentrations in breast cancer tissue compared to healthy tissue.
The idea that viruses could influence cancer development or recurrence has been around since the 1930s, particularly in mouse models. But this new research is among the first to show how non-oncogenic, respiratory viruses—those not traditionally associated with cancer—might still play a key role in its resurgence.
Role of Inflammation and the Immune System
One of the most compelling parts of the study is the insight into how the immune system's response, not the virus itself, may be the real driver of cancer recurrence.
After remission, it’s common for a few cancer cells known as dormant disseminated cancer cells (DCCs), to remain hidden in tissues like the lung, bone, or liver. These DCCs are typically inactive, posing no threat unless triggered.
Inflammatory responses to infections, especially those that involve cytokines like IL-6, appear to disturb this dormancy. In simple terms, inflammation acts like a wake-up call for these sleeping cells.
The researchers demonstrated that only when the viral infections resulted in elevated levels of inflammatory markers did the dormant cells awaken. This opens up new avenues for therapeutic research focused on blocking inflammation, rather than targeting cancer cells directly.
What This Means for Breast Cancer Survivors?
This is not a reason for panic but it is a call for caution. As DeGregori explains, “If you are a cancer patient who has these dormant cells, you may end up living a normal life and dying with these dormant cells, instead of dying because those dormant cells awakened. But if you get a respiratory virus like influenza or COVID, your chance of dying from those dormant cells awakening is much greater.”
Millions of breast cancer survivors around the world, many of whom are years or even decades into remission—could unknowingly carry dormant cells. For them, a common respiratory illness may no longer be just an inconvenience; it may be a risk factor for relapse.
Could Vaccination Be Protective?
Can we reduce this risk with vaccines? It’s too early to say definitively, but the idea is promising. If viral infections act as a trigger, then preventing infection might, in turn, prevent relapse.
DeGregori’s team is now exploring whether flu and COVID-19 vaccinations could lower the likelihood of dormant cell reactivation. This would have wide-ranging implications not just for cancer survivors, but for public health policy as a whole.
The idea that a respiratory virus could reignite cancer long after remission is unsettling but not entirely surprising. As science continues to unravel the complex relationship between our immune system, viruses, and cancer, this study offers one clear message:
Remission isn’t always the end and staying healthy may mean more than avoiding recurrence it could mean avoiding infection altogether.
Legionnaires Outbreak: All That You Need To Know About The Disease That Killed 1 And Left 22 Sick In New York
Credits: Canva
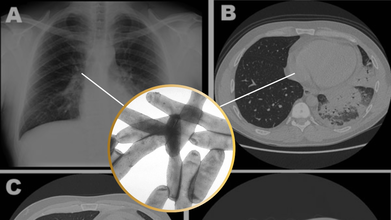
With 6,000 cases of Legionnaires reported annually in the United States, scientists still think it is underdiagnosed as it could be hard to distinguish from other kinds of pneumonia or respiratory issues.
As of now, New York City has fallen prey to Legionnaires' disease outbreak. At least 22 people have fallen ill, and one person has been declared dead in Harlem, as per the New York City Health Department.
The Reason Of This Spread
As per the city health officials, people became ill after breathing in bacteria sprayed from cooling tower in central Harlem. Cooling towers help regulate building temperature. The city health department also said in a news release on Wednesday that it was testing cooling towers in the area and are continuously investigating the outbreak.
What Is The Legionnaire's Disease?
As per the Centers for Disease Control and Prevention (CDC), Legionnaire's disease is a serious type of pneumonia that is caused by Legionella bacteria. This bacteria is known for causing two types of diseases, one of them being Legionnaire's disease, a severe form of pneumonia; while the other one is Pontiac fever, which is a mild illness that can include fever, muscle aches and headaches.
It is very rare that this bacteria can cause infection outside of the lungs and affect heart or wound infections, notes CDC.
Common Symptoms
Legionnaires' disease symptoms usually develop 2 to 14 days after exposure to Legionella bacteria, but it can take longer.
The symptoms of Legionnaires' disease are similar to other types of pneumonia.
Symptoms include:
- Cough
- Fever
- Headaches
- Muscle aches
- Shortness of breath
Other symptoms, such as confusion, diarrhea, or nausea can also occur.
After this outbreak, which has been linked with a cluster, the deputy commissioner of division of infectious diseases at the New York City Department of Health and Mental Hygiene, Dr Celia Quinn, said that the risk is low for most people, however, there could be additional cases linked with this cluster.
Legionnaire's Disease in the US
Cases have been steadily rising over the past two decades. While there isn’t a single known cause for this increase, experts believe several factors may be contributing, including aging water infrastructure, poor system maintenance, rising water temperatures, and improved disease tracking and awareness.
Outbreaks are more common during the warmer months, particularly summer, when more buildings rely on cooling towers for air conditioning systems.
Health professionals note that while a similar report in winter might raise fewer concerns, the combination of summer heat and rising case numbers highlights the importance of staying vigilant during peak Legionella season.
Who Are At Risk?
While most healthy people exposed to the bacteria do not get sick, people who are 50 or older, or are current or former smokers, or people with a weakened immune system or chronic conditions, such as cancer, lung disease, diabetes or kidney and liver failure may be at a higher risk.
Legionnaires’ disease often becomes more severe within the first week of symptoms. In serious cases, patients may need hospitalization and oxygen support. If the illness progresses, it can lead to complications like lung failure or heart damage. According to the CDC, about 1 in 10 people who contract Legionnaires’ disease do not survive.
Is It Contagious?
Legionnaires’ disease doesn’t spread from person to person. It’s usually contracted by breathing in mist or vapor contaminated with the bacteria. Outbreaks are often linked to cooling towers in large cities. In rare instances, the illness can also be caused by inhaling contaminated soil.
© 2024 Bennett, Coleman & Company Limited

