- Health Conditions A-Z
- Health & Wellness
- Nutrition
- Fitness
- Health News
- Ayurveda
- Videos
- Medicine A-Z
- Parenting
Dr. Mathew Kalarickal, 'The Father of Angioplasty' In India Passes Away At 77; How The Procedure Transformed Heart Care?

Dr. Mathew Samuel Kalarickal, a pioneer of interventional cardiology, has passed away on April 18, 2025, in Chennai, at the age of 77, marking an end to an era in coronary angioplasty and stenting technology. Popularly known as the 'Father of Angioplasty in India,' Dr. Kalarickal transformed heart care, changing the lives of thousands of patients and redefining the face of contemporary interventional cardiology.
Born on January 6, 1948, in Kerala, Dr. Kalarickal's journey to becoming one of the world's most renowned cardiologists was set early in life. After completing his medical studies at Kottayam Medical College, he went on to pursue specialization in cardiology from Chennai but his stint in the United States of America, under the guidance of Dr. Andreas Gruentzig—the man universally accepted as the 'Father of Coronary Angioplasty'—would establish the foundation for his groundbreaking career.
Dr. Kalarickal's return to India in 1985 proved to be turning point. Coronary angioplasty was a new, unexplored area in India at that time, and one that fell behind progress in the U.S. and Europe. Sensing this lacuna, Dr. Kalarickal chose to introduce this revolutionary procedure to India, with a vision of making lifesaving heart procedures reach more people.
First Angioplasty in India
In 1986, Dr. Kalarickal performed the very first angioplasty in India, a process which would subsequently alter the direction of heart treatment in the country. Angioplasty at that time was not a widely known procedure in India, and coronary artery disease was on the rise. During the first year, he had only treated 18 patients. But by 1987, that figure had risen to 150, an unmistakable indicator of both the increasing demand for this life-saving operation and the confidence that patients had in Dr. Kalarickal's skills.
His success in India did not remain confined to its borders, Dr. Kalarickal played a key role in setting up angioplasty centers in various nations in the Asia-Pacific region, such as Pakistan, Bangladesh, Sri Lanka, the United Arab Emirates, Indonesia, Thailand, and Malaysia. His relentless efforts to educate and train physicians in these nations helped ensure that this new technique spread like wildfire, eventually saving countless lives and making heart procedures more available worldwide.
Role of Dr. Kalarickal in Expanding Angioplasty Globally
Dr. Kalarickal's role was not just to bring angioplasty to India and the rest of the region. As an innovator, he was a pioneer in bringing new innovations to the world of angioplasty and stenting. One of his greatest feats was becoming the first Indian cardiologist to introduce and practice the application of drug-eluting bio-absorbable stents, which improved the efficacy of angioplasty by a large margin and minimized the threat of re-blockage in coronary arteries.
Having done more than 10,000 angioplasties, Dr. Kalarickal's expertise and commitment to improving heart health were second to none. He also contributed significantly to academia, establishing the National Angioplasty Registry of India, through which data on angioplasty operations could be gathered and analyzed to streamline and enhance practice nationwide. His contributions had an effect on the medical fraternity and made him a mentor to numerous budding cardiologists in India and overseas.
Dr. Kalarickal's success was not limited to the operating room. His leadership positions in major medical societies demonstrate his reputation as a world leader in interventional cardiology. He was president of the Asian-Pacific Society of Interventional Cardiology from 1995 to 1997 and then went on to chair the Asian-Pacific Society of Cardiology section of Interventional Cardiology between 1995 and 1999. His presidency in these societies promoted the use of angioplasty and stenting procedures around the world and consolidated the group of cardiologists in Asia.
His work was duly appreciated in many awards and honors. Dr. Kalarickal received the esteemed Padma Shri award in 2000, one of the highest civilian awards in India, for his outstanding work in cardiology. He was also awarded the Dr. B.C. Roy Award in 1996 for his notable contributions to medicine, the Doctor of Science Award by Dr. M.G.R. University in 2003, and a Lifetime Achievement Award in 2008.
While Dr. Kalarickal was well-known for his medical knowledge, he was as much admired for being a mentor. Dr. Sai Satish, who is a senior interventional cardiologist in Chennai, was trained by Dr. Kalarickal and collaborated with him for more than two decades. Talking about his experiences during his mentor's time, Dr. Satish stated, "There will never be another Dr. Mathew Samuel Kalarickal in my life.". He taught me in ways that few people ever managed, and I will miss him every time I enter a cath lab." This is a sentiment shared by many other cardiologists who were fortunate enough to learn from him. His dedication to educating and empowering the future generation of heart doctors has left an invaluable legacy on the specialty of cardiology.
Dr. Kalarickal's contributions have saved thousands of lives, and his legacy will never be lost in the profession of interventional cardiology. His vision, commitment, and pioneering attitude have revolutionized heart disease treatment in India and across the globe. With the advent of angioplasty, he revolutionized the procedure that used to be an extremely invasive and dangerous one and turned it into a routine, life-saving one.
How Angioplasty Saves Your Heart?
Angioplasty is a minimally invasive procedure to open up narrowed or blocked coronary arteries due to a buildup of fatty plaques. Plaque buildup in the arteries over time can limit blood supply to the heart, resulting in angina (chest pain) or even heart attacks. Angioplasty is done to relieve these blockages, restore normal blood flow, and prevent heart-related complications. But in what way precisely does angioplasty save the heart?
While undergoing angioplasty, a catheter is inserted into the clogged artery with a balloon at the end. The catheter is advanced through the bloodstream with great caution until it enters the area where the blockage is. Having reached its destination, the balloon is inflated, pushing the plaque against the artery walls, effectively opening up the artery and reinstating blood circulation to the heart. In most instances, a tiny mesh tube known as a stent is also inserted to keep the artery open and prevent it from closing again.
Angioplasty can be carried out in patients with different types of coronary artery disease, such as patients who have experienced heart attacks, those with chronic angina, and those at high risk for cardiac events due to plaque deposition. Angioplasty is commonly carried out on patients who are not ideal candidates for standard open-heart surgery.
Instant Relief and Long-term Advantages
Perhaps the greatest benefit of angioplasty is the relief that it brings promptly to the patient. Post-procedure, patients can notice dramatically decreased symptoms of chest pain, shortness of breath, and tiredness, all typical with clogged arteries. The normalization of blood flow tends to keep the heart from working as hard and lowers the risk of heart attacks.
In the long run, angioplasty ensures that the heart is not subjected to further harm by providing it with a sufficient supply of oxygenated blood. This is particularly vital in individuals suffering from coronary artery disease because continuous blood flow is crucial to maintaining heart muscle health. Angioplasty can greatly eliminate the risk of heart failure, heart attack, or stroke by opening up clogged arteries. Also, the procedure has been demonstrated to enhance quality of life in general, since patients are frequently able to resume normal activities following the procedure without the restrictions created by chest pain and other symptoms.
Flu Season Update: CDC Reports Declining Cases Across The US

Credits: Canva
Flu cases are starting to fall, yet experts caution that the United States still faces risks. In the week ending January 10, fifteen more children died from the flu, bringing the total pediatric deaths this season to 32, as per NBC News.
Flu Season: Latest CDC Data
On Friday, the Centers for Disease Control and Prevention (CDC) reported an 18% drop in confirmed flu cases compared with the previous week. Visits to doctors for respiratory illnesses decreased by more than 5%, and hospitalization rates fell by nearly 55%. Influenza-related deaths, however, rose by 2%.
So far this flu season, the CDC estimates that 18 million people have been infected, including 230,000 hospitalizations and 9,300 deaths.
“It seems like there is some cautious good news that cases are declining,” said Jennifer Nuzzo, director of the Pandemic Center at Brown University School of Public Health. “But I’m going to put a giant asterisk on this because that does not mean the worst is behind us.”
Last year, flu cases dipped around this time before climbing again in early February.
Flu Season: State-by-State Variation
CDC data reflect a national trend, but not all states have necessarily reached their peak. “We are not going to all experience this at the same time,” said Beth Carlton, a public health professor at the University of Colorado, as per NBC News. “Nationwide, the trend is downward, but different states and communities may see spikes as the virus spreads.”
Flu often appears first in densely populated areas like New York City before moving to rural regions, but the virus can behave unpredictably.
Flu Season: Impact on Schools
Although flu cases may be falling overall, other winter illnesses such as norovirus, Covid, and strep throat are still causing school closures in states including Arkansas, Kansas, Kentucky, Tennessee, and West Virginia.
High flu activity continues in Idaho, New Mexico, New York, and parts of Appalachia, while Montana, South Dakota, Vermont, and Wyoming report lower case numbers.
“The number of people hospitalized for influenza around New Year’s was extremely high—the second highest in the past decade, with last year being the highest,” Carlton said.
Flu Season: A Difficult Flu Season
This year’s severe flu season is driven by a heavily mutated strain of influenza A called H3N2 subclade K. Its mutations make it less similar to the strain used in this year’s vaccine. Influenza-like illnesses, including RSV and Covid, are also unusually high, Nuzzo said.
“Typically these viruses peak at different times, but this year they are peaking together, making the season particularly harsh,” she noted.
While there were concerns that the vaccine would be less effective against subclade K, recent research shows the current flu shot still offers protection, particularly against hospitalization. The vaccine covers three strains: H1N1, H3N2, and one B strain.
Flu Season: Pediatric Risk
As per NBC News, last year marked the deadliest flu season for children since the CDC began tracking pediatric deaths, with 289 children dying—more than during the 2009 H1N1 pandemic.
“That double peak last season clearly had consequences,” Nuzzo said. “Any decline this season is welcome, but we can’t assume the worst is over.”
Among children eligible for the flu shot whose vaccination status was known, 90% of pediatric deaths occurred in unvaccinated kids.
Following recent CDC guidance, flu shots are no longer recommended for all children, a change from the previous advice that everyone six months and older should be vaccinated annually.
Anktiva Approved In Saudi Arabia As World’s First Lung Cancer Therapy — All You Need to Know

Credits: Canva
The Saudi Arabian Food and Drug Authority has cleared Anktiva, an IL-15–based immunotherapy created by billionaire physician-scientist Patrick Soon-Shiong and his biotech firm ImmunityBio, for the treatment of bladder cancer and lung cancer. This marks the first time the therapy has received national regulatory approval outside the United States.
The move signals an important global step for Anktiva, which currently holds a limited approval from the U.S. Food and Drug Administration. In the U.S., the drug is authorised only for patients with BCG-unresponsive, non–muscle-invasive bladder cancer (NMIBC) that includes carcinoma in situ. American regulators have so far resisted expanding its use to other bladder cancer subtypes. Saudi regulators, however, have adopted a broader stance, approving Anktiva for two cancer types under their domestic regulatory system.
What Is Anktiva?
Anktiva is an interleukin-15 receptor agonist designed to stimulate the body’s own immune defences. It works by activating and expanding natural killer (NK) cells and memory CD8⁺ T cells, which play a key role in immune surveillance. Unlike chemotherapy or gene-based treatments, Anktiva does not attack tumour cells directly. Instead, it boosts existing immune pathways to help the body recognise and destroy cancer cells.
ImmunityBio describes Anktiva as “the first FDA-approved immunotherapy that activates what’s called a natural killer cell to target and kill non-muscle-invasive bladder cancer cells.” In clinical practice, the drug is used alongside BCG (Bacillus Calmette-Guérin) in patients whose NMIBC has not responded to BCG alone. It is administered directly into the bladder through a catheter, followed by a structured maintenance schedule
Clinical Evidence Supporting FDA Approval in NMIBC
The FDA’s approval, issued on April 22, 2024, was based on results from a single-arm clinical study involving 77 patients with BCG-unresponsive stage 0 NMIBC. Participants received intravesical Anktiva combined with BCG, with maintenance therapy continuing for as long as 37 months.
The main efficacy results were as follows:
- Complete response rate: 62%
Durability:
- 58% of patients who responded remained disease-free for at least 12 months
- 40% stayed disease-free for 24 months or longer
For patients facing the prospect of radical cystectomy as the only curative option, these results were considered clinically significant. Still, the absence of a randomised control group has remained a point of contention among regulators and experts.
Regulatory Tension in the United States
Although the FDA approved Anktiva for NMIBC cases involving carcinoma in situ, it declined to extend the indication to patients with papillary-only disease. ImmunityBio pushed back against the decision, arguing that the same clinical data had already been deemed sufficient to support approval in a closely related patient group.
Rachel Sherman, MD, former principal deputy commissioner of the FDA, publicly criticised the agency’s stance, saying: “it is incomprehensible to me that the FDA refuses to file a supplemental BLA, stating the study is not sufficient to support a regulatory review, when it has already approved a product based on that very same study in essentially the same indication and population.”
The FDA has also expressed concerns about how the drug has been marketed. It issued a warning letter to ImmunityBio over promotional materials that cited survival benefits and cystectomy-avoidance rates not supported by robust evidence.
Saudi regulators, by contrast, have taken a more permissive view, approving Anktiva for both bladder and lung cancer and highlighting a willingness to act in areas of high unmet medical need.
With this decision, Saudi Arabia becomes the first country to approve Anktiva beyond NMIBC, potentially placing itself at the forefront of evaluating the therapy’s wider role across multiple cancer types.
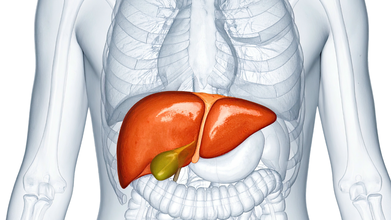
India Ranks Third in Non Alcoholic Fatty Liver Disease Cases, Study Finds
Credit: Canva
Once a rare condition, non-alcoholic fatty liver disease (NAFLD) now affects one in three Indians, scientists say.
NAFLD, now called as metabolic dysfunction-associated steatotic liver disease (MASLD), is when excess fat builds up in the liver, unrelated to heavy alcohol use, due to obesity, Type 2 diabetes, high blood pressure and cholesterol.
It ranges from simple fat accumulation to inflammation and damage, which can progress to fibrosis, cirrhosis or liver cancer, The disease often has no symptoms and is managed with lifestyle changes such as diet and weight loss.
A JAMA study has now found that about 40 percent of the global population is now suffering from NAFLD, with abdominal obesity identified as its single biggest risk factor. Between 2010 and 2021, India recorded a 13.2 percent increase in age-standardized prevalence, ranking just behind China at 16.9 percent and Sudan at 13.3 percent.
What Did The Study Find?
Researchers found that nearly 70 percent of people with Type 2 diabetes and about 80 percent of those with obesity are affected by NAFLD. They also discovered that NAFLD prevalence is higher in men than in women, with rates of 15,731 per 100,000 population in men compared with 14,310 in women.
Additionally, the disease peaks earlier in men, between 45 and 49 years of age, while women show the highest prevalence between 50 and 54 years.
Why Is NAFLD on the rise?
Poor diets (high carbs/sugar), sedentary habits and rising obesity are some of the key reasons why an uptick in NAFLD cases has been seen pan-India. Increased intake of refined carbs, sugary drinks, processed foods and unhealthy fats can increase the risk of obesity, diabetes, hypertension and high cholesterol which can pave the way for this liver disease.Experts also note that working long hours at desks without any proper physical activity can lead to weight gain and fat accumulation in the liver.
According to the Union health ministry, the prevalence of the condition could be in the range of 9-53 percent. Multiple other health studies also suggest nearly 40 percent of urban Indians may have some form of fatty liver disease
Hepatologist Dr Cyriac Abby Philips, popularly known as LiverDoc on social media, noted on X that many patients do not realize that timely lifestyle changes can completely reverse the condition. “All it takes is being in charge of your body and health. No shortcuts—go slow and steady,” he wrote.
If left untreated, NAFLD can progress to Non-Alcoholic Steatohepatitis (NASH), where liver inflammation begins. Over time, this inflammation can lead to scarring of the liver, known as fibrosis. Advanced fibrosis results in cirrhosis, which severely affects liver function.
NAFLD can also increase the risk of chronic liver disease, liver failure and hepatocellular carcinoma. Many patients diagnosed with liver cancer have a history of untreated fatty liver.
© 2024 Bennett, Coleman & Company Limited

