- Health Conditions A-Z
- Health & Wellness
- Nutrition
- Fitness
- Health News
- Ayurveda
- Videos
- Medicine A-Z
- Parenting
- Web Stories
India’s Covid Surge Worsens With Active Cases Over 6100 And 6 Deaths Reported

Credits: Health and me
As of June 8, 2025, India is struggling to contain another alarming surge in COVID-19 cases. The active caseload of the country has also breached the 6,100 mark and stood at 6,133 as of then, as per the Ministry of Health and Family Welfare. With this increase came six more COVID-19 fatalities, causing waves of fear throughout public health systems and renewing questions over virus resurgence during a post-pandemic world.
Though this is hardly the crisis of the previous waves, infection trajectory and changing viral subvariants indicate a changed dynamic with the virus — no longer one of emergency but one that necessitates sustained vigilance.
At the lead of this fresh wave is Kerala, which reported 144 new cases within the last 24 hours, increasing its active caseload to 1,950 — roughly one-third of the country's total. West Bengal reported 71 new infections, and Delhi had 21, increasing their respective active cases to 693 and 686. Maharashtra, once a hotspot during previous waves, reported 18 new cases, taking its total to 595.
This regional spread points to how the virus, although diluted in public perception, still gets around quietly, usually erupting seasonally in predictable fashion especially in city and densely populated areas.
Emerging Subvariants and What We Know About Them
The recent surge of cases is attributed by recent updates from the Indian SARS-CoV-2 Genomics Consortium (INSACOG) and the Indian Council of Medical Research (ICMR) to several subvariants of the Omicron variant. These are JN.1, LF.7, XFG, and NB.1.8.1 — all classified under the "Variants Under Monitoring" category by the World Health Organization (WHO) up to May 2025.
Although not yet designated as "Variants of Concern" or "Variants of Interest," these subvariants have shown a slightly increased transmissibility. Of concern, symptoms have been predominantly mild, akin to those of the flu or common cold.
The prevalent subvariant, JN.1, covers 53% of infections in the nation today, while LF.7 and NB.1.8.1 are also starting to make their impact felt in states such as Gujarat and Tamil Nadu. Specialists have warned that even though these subvariants will not be a threat at high levels in the immediate future, their capacity for mutation and propagation in huge populations should not be underrated.
Doctors and virologists on all sides concur that COVID-19 is firmly established in its endemic stage within India and the world at large. Just like the flu, it should go around seasonally, along with other respiratory illnesses.
The ICMR observes that India has gained good "hybrid immunity" — a blend of natural infection and vaccine-provided protection — which is providing good defense against severe illness. Dr. Rajiv Bahl, ICMR Director General, emphasized that this rise in cases now does not warrant alarm or large-scale booster vaccination campaigns. Nevertheless, he urged doctors to evaluate patients on a case-by-case basis for booster requirements, particularly with comorbidities or weakened immunity.
In a nutshell, India is not technically in a medical emergency but is adjusting to a new type of long-term relationship with the virus — managing intermittent surges with forethought, not frenzy.
Are Vaccines Still Relevant in 2025?
India's vaccination campaign, launched in January 2021, has administered more than 2.2 billion doses so far — predominantly Covishield (AstraZeneca) and Covaxin (Bharat Biotech). Both vaccines provided substantial protection in previous waves and helped to flatten the curve.
Today, public health experts indicate that though the initial vaccines might have waning efficacy against newer subvariants of Omicron, they still provide essential protection against severe disease outcomes and hospitalization.
More recent nasal vaccines for Omicron-specific strains by Bharat Biotech and Indian Immunologicals were launched but experienced low public acceptance. Physicians blame this for both low risk perception and fatigue related to the pandemic. Despite this, vaccine equity and accessibility continue to be critical in preparing for any potential future variants that might gain more immune escape capacity.
Hospitalizations Are Low, But Public Vigilance Must Be Maintained
While hospitalization has not experienced a dramatic spike, experts caution that virus underestimation could have far-reaching effects. The virus's reproductive number (R0) is presently low, signaling minimal spread, but it can rapidly become high in the event of a more contagious strain or a decline in public health measures.
Dr. Bahl stressed, "COVID-19 is no longer an occasional phenomenon but a periodic challenge. We must approach it the way we approach seasonal flu — with wise habits and timely interventions."
Delhi High Court Urges Protocol Review
Having sensed the gradual but relentless rise, the Delhi High Court recently asked the Central government to submit an exhaustive report on sample collection and transport procedures. The focus is on the need to tighten India's Standard Operating Procedures (SOPs) in the light of changing viral dynamics.
This is a timely reminder: endemic COVID-19 management demands not only medical preparedness but administrative flexibility, popular awareness, and a robust surveillance system as well.
Public Health Guidance for Now and the Immediate Future
The present guidance from public health officials mirrors what the international community has collectively embraced as received wisdom:
- Keep practicing proper hand hygiene.
- Use masks in indoor, poorly ventilated, or congested settings.
- Self-isolate and get tested if having cold-like symptoms.
- Stay home and refrain from unnecessary social contacts if ill.
- Heed credible public health guidance and eschew disinformation.
Perhaps most importantly, maintaining a healthy immune system through regular exercise, balanced nutrition, adequate hydration, and mental well-being remains the best long-term defense against not just COVID-19, but a host of lifestyle-related illnesses.
COVID May Be Endemic, But It’s Not Over
India's June 2025 peak of more than 6,100 active cases and six reported fatalities might not be its alarum peaks of 2020 and 2021 but signals a key reality: COVID-19 is not going anywhere. As it continues to become a chronic, recurring sickness, public health infrastructure and people must now do their part to remain vigilant, behave responsibly, and maintain the hard-won lessons of the past five years.
Invasive Meningococcal Disease Confirmed In Maldives; What Are The Symptoms Of This Bacterial Infection?

Credits: Health and me
Health authorities in the Maldives have confirmed a case of invasive meningococcal disease, triggering immediate precautionary measures to prevent further spread and protect public health. With the Maldives Health Protection Agency's (HPA) announcement of a confirmed case of invasive meningococcal disease (IMD) on the night of June 7, prompt public health response was initiated. Contact tracing, prophylactic treatment, and increased surveillance are now in motion. The case signifies the need for heightened global awareness of the uncommon—but potentially fatal—bacterial infection.
Whereas meningococcal disease in the Maldives is rare and usually the result of travel outside the country, the case here is particularly concerning since it indicates local transmission. In the past, the archipelago has experienced only isolated cases and these have usually been traced to pilgrims who have come back from Hajj pilgrimages in Saudi Arabia.
Invasive meningococcal disease stems from the bacterium Neisseria meningitidis, a Gram-negative diplococcus that typically resides harmlessly in the nose and throat of up to 10% of people. Occasionally, it breaches the body’s defenses, causing:
Meningococcal meningitis – inflammation of the brain and spinal cord linings.
Meningococcal septicemia (meningococcemia) – a bloodstream infection that damages blood vessels and can result in hemorrhaging in skin and organs.
If not treated immediately, IMD is lethal within hours—a stark fact testified to by CDC information on fatality rates of 10–15%, with treatment, jumping to 18% in a few U.S. epidemics.
How Does Meningococcal Disease Spread?
Meningococcal bacteria are transmitted through respiratory droplets—by coughing, sneezing, kissing, or sharing food and drinks. The greatest risk occurs between people with extended, close contact, such as family members and sexual partners. Prolonged riding in enclosed vehicles—buses, planes—with the infected person also increases risk greatly.
CDC states that infants below one year, adolescents 16–23 years old, immunocompromised patients, and residents of communal environments are at greatest risk.
Early Symptoms of Meningococcal Disease
IMD at first presents a nonspecific viral illness but can worsen suddenly. Parents and caregivers must be aware of the following signs:
- Fever, headache, stiff neck – classic symptoms of meningitis
- Red spots or rash – typically seen as pinpricks or larger bruise-like patches, a sign of blood vessel involvement
- Nausea, vomiting, photophobia (light sensitivity)
- Confusion, lethargy, rapid breathing, seizures – signs of severe progression
- Neck stiffness and changed mental status, usually with fever
In the most severe cases, sepsis, exhaustion, coldness of extremities, and coma may ensue—all necessitating immediate medical intervention. Shockingly, worsening can happen within 6–12 hours of the onset of symptoms .
The HPA, falling under the Ministry of Health, immediately initiated tracing and gave prophylactic antibiotics—usually rifampin, ciprofloxacin, or ceftriaxone—to high-risk contacts This is in line with CDC recommendations to prevent nasopharyngeal carriage and interrupt further spread.
Relaying precise definitions of "close contact," the HPA's reach encompasses family members, travel mates, and those exposed to respiratory secretions of the patient.
Diagnosis and Treatment of Meningococcal Disease
The gold-standard diagnosis for invasive meningococcal disease involves a combination of blood cultures and cerebrospinal fluid (CSF) analysis obtained through lumbar puncture. However, in cases where increased intracranial pressure is suspected, performing a lumbar puncture may need to be delayed to avoid complications. Additionally, polymerase chain reaction (PCR) testing plays a crucial role in rapidly identifying the infection, particularly when prior antibiotic treatment may interfere with traditional culture results.
IMD survivors develop severe complications: hearing loss, neurological injury, kidney failure, or limb amputation by necrosis. Unfortunately, natural infection does not offer absolute lifelong immunity; recurrence, although infrequent, can occur, warranting immune deficiency assessments.
Is the Disease Preventable by Vaccination?
Vaccination is the best protection. Vaccines protect against several serogroups (A, B, C, W, Y, X) and are universally advised—particularly among adolescents, travelers, and those at risk.
In Maldives, HPA advises unvaccinated persons—particularly Hajj pilgrims who departed within 14 days of booster doses—to see health practitioners promptly.
Salmonella Outbreak Triggers Massive Egg Recall Across 7 States

Credits: Canva
A salmonella outbreak linked to a large egg recall has sickened dozens of people across seven U.S. states in the West and Midwest, federal health officials confirmed on Saturday.
Egg Recall Affects Over a Million Eggs
The August Egg Company has recalled approximately 1.7 million brown organic and brown cage-free eggs distributed to grocery stores between February and May. The recall was issued due to potential salmonella contamination, as stated in an announcement posted on the Food and Drug Administration’s (FDA) website on Friday.
States Impacted and Reported Cases
According to the U.S. Centers for Disease Control and Prevention (CDC), at least 79 people across seven states have been infected with a strain of salmonella traced back to the recalled eggs. Of these, 21 individuals have been hospitalized. The recall affects the following states: Arizona, California, Illinois, Indiana, Nebraska, New Mexico, Nevada, Washington, and Wyoming.
Consumers are advised to check the FDA and CDC websites for a full list of affected brands, plant codes, and Julian dates to identify whether the eggs they have purchased are part of the recall.
Recognizing Salmonella Symptoms
Salmonella infection can cause a range of symptoms, including diarrhea, fever, stomach cramps, severe vomiting, and dehydration. While most healthy individuals recover within a week without medical intervention, the illness can become more serious in certain groups.
High-Risk Groups Urged to Take Precaution
Young children, older adults, and individuals with weakened immune systems are at a higher risk of severe illness and may require hospitalization. Health officials urge anyone experiencing symptoms after consuming eggs to seek medical attention promptly.
Ongoing investigations are being conducted to determine the full scope of the outbreak and ensure contaminated products are removed from shelves.
Previous Outbreaks
The Health and Me has previously also reported on various Salmonella outbreaks happening in the US, including the outbreak caused by tomatoes, which has led to the US Food and Drug Administration (FDA) issue a Class I recall, also considered the highest warning label.
Class I recall means that there is a reasonable change that using the product could lead to "serious adverse health consequences or death".
Another outbreak was linked to Florida-grown cucumbers about which the CDC has also warned the population.
Very similar to what is happening now, another Salmonella outbreak was linked with backyard poultry and products like eggs, noted the CDC.
What Is Salmonella?
As per the US Food and Drugs Administration (FDA), Salmonella are a group of bacteria that can cause gastrointestinal illness and fever called salmonellosis. It can be spread by food handlers who do not wash their hands and/or the surfaces and tools they use between food preparation steps. It can also happen when people consume uncooked and raw food. Salmonella can also spread from animal to people.
FDA notes that people who have direct contact with certain animals, including poultry and reptiles can spread the bacteria from the animal to food if hand washing hygiene is not practiced.
Pets too could spread the bacteria within the home environment if they eat food contaminated with Salmonella.
World Brain Tumor Day 2025: Theme, History, And Significance
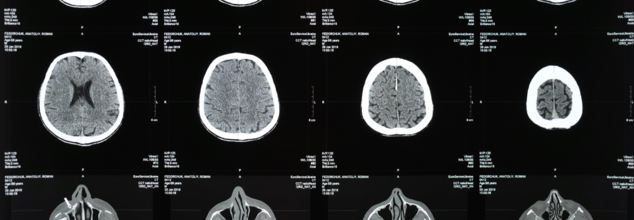
Credits: Canva
Every year, on June 8, World Brain Tumor Day is observed, which highlights the urgent need for research, awareness, and support for those living with the disease. It is also a day that gives us the chance to spread awareness about it, including the symptoms and the causes.
World Brain Tumor Day 2025 Theme:
Every year, a theme is decided in order to focus on the goals, and this year the theme for World Brain Tumor Day is 'Empowering Lives Though Brain Tumor Awareness'. This focuses more on diagnosis, support, and early assessment of the tumor. This theme also brings back the attention to the need for conversation that must be done around this.
History of World Brain Tumor Day
Deutsche Hirntumorhilfe e.V. (German Brain tumor Association) internationally established World Brain tumor Day on June 8, 2000, to honour and support brain tumor patients and their families globally. The association chose this date because on June 8, 1952, Professor Martin Lewis of University College London diagnosed the first recorded brain tumor case.
World Brain Tumor Day Significance:
Along with raising awareness, the day also aims to inform the community about its symptoms, diagnoses and treatment options. It also assists the brain patients and their families, fosters research and progress in brain tumor treatment methods. The day also aims to champion improved healthcare access and support for individuals impacted by brain tumors.
It also motivates early detection and intervention to enhance patient outcomes.
What Is Brain Tumor?
Before diving into the concept of a brain tumor, it is important to first understand what a tumor is. A tumor refers to an abnormal lump or mass that forms due to the uncontrolled growth of cells in the body.
tumors are broadly classified into two main categories:
- Benign
- Malignant
A benign tumor consists of normal cells that have grown excessively to form a lump. This overgrowth may result from something going wrong in the body, but the cells themselves are not cancerous. On the other hand, a malignant tumor is made up of abnormal cells that grow uncontrollably. These are cancerous cells, and their aggressive nature can lead to serious health issues.
A brain tumor is a condition in which abnormal cells develop within any part of the brain. Similar to tumors elsewhere in the body, brain tumors can also be benign (non-cancerous) or malignant (cancerous). The presence of a tumor in the brain can interfere with normal brain function, depending on its size, type, and location.
Our bodies possess a natural healing mechanism that is crucial for survival. This repair system is activated whenever there is damage from injury, radiation from the sun, or harmful chemicals in the environment. However, this process can occasionally go wrong. When it does, small clusters of cancerous cells may begin to form. In most cases, the immune system successfully detects and destroys these abnormal cells before they grow. But in rare instances, these cancerous cells evade immune detection and continue to grow, leading to the formation of tumors or cancers.
Such abnormal growths can occur anywhere in the body. When these growths are located in the brain or spinal cord, they are referred to as Central Nervous System (CNS) tumors.
Causes of Brain Cancer:
The exact cause of brain tumors remains unknown. However, several theories and contributing factors have been proposed. Many medical experts believe that prolonged exposure to radiation, such as frequent x-rays or radiation therapy, may increase the risk of developing a brain tumor. Additionally, there is a growing concern about the potential link between long-term use of electronic gadgets—like mobile phones—and an increased risk of various types of cancers, including brain tumors. However, no conclusive scientific evidence has confirmed this link so far.
Research in this area is still ongoing, and scientists continue to investigate the causes and risk factors associated with brain cancer to gain a better understanding and develop more effective treatments.
© 2024 Bennett, Coleman & Company Limited

