- Health Conditions A-Z
- Health & Wellness
- Nutrition
- Fitness
- Health News
- Ayurveda
- Videos
- Medicine A-Z
- Parenting
Lancet Study Reveals 'Two Factors' That Decide The Life Expectancy Of People in US
Credits: Canva
A new Lancet study titled Ten Americas: a systematic analysis of life expectancy disparities in the USA highlights alarming disparities in life expectancy across racial, ethnic, and geographic groups in the United States.
The study analyzed death records and population estimates from the year 2000 to 2021 and revealed that life expectancy can vary by more than 20 years depending on one's race, ethnicity and location.
What did The Study find?
The study found that life expectancy gaps have widened, despite the increase in health policies, screenings, and awareness. Looking at the first two years of the COVID-19 pandemic, also noted disparities and unequal distribution of resources and opportunities. Senior author Christopher JL Murray also pointed out that these inequalities have profound effects on the well-being and longevity, especially for the marginalized populations.
Life expectancy and the trend
The trend shows that life expectancy rates have gone down, and the gap between the lowest life expectancy group to the highest life expectancy group has only widened.
In 2000, life expectancy ranged from an average of 70.5 years for Americans in the lowest life expectancy group to 83.1 years for those who were in the highest life expectancy group. This means, in 2000, there was a difference of 12.6 years between the two groups. However, by 2010, the gap widened to 13.9 years, further widening to 18.9 years in 2020 and 20.4 years in 2021. The study also highlighted that life expectancy in the US is moving in the wrong direction and has been falling behind the countries with the same wealth and resources in the past two decades.
Who has the lowest life expectancy vs who has the highest?
The groups with the lowest life expectancy in 2000 included Black Americans living in non-metropolitan and low-income counties in the south, and some of those who lived in highly segregated urban areas. American Indians and Alaska Native individuals who lived in the West also had low expectancies.
However, Asian Americans had the highest average life expectancy during the same period. While over the decade, life expectancy increased for all groups, American Indians and Alaska Natives were left behind.
For the White and Latino population, the life expectancy varied based on their geographic location. White Americans in low-income regions like Appalachia and the Lower Mississippi Valley experienced lower life expectancies than those in the other areas.
When did the gap widen?
By the year 2021, the life expectancy disparities had grown, and the COVID-19 pandemic also worked as a catalyst for the cause. Asian Americans had an average life of 84 years, while American Indians or Alaska Natives had a lower average of 63.6 years. Non-Hispanic Black Americans also noted a sharp decline in their life expectancy, it dropped from 74.8 years in 2019 to 71.0 in 2021.
The study highlighted the economic effect of the COVID-19 pandemic on the marginalized population, which has led to catastrophic losses in life expectancy. These populations have been historically underserved and due to this were disproportionately affected by the pandemic. This resulted in widening health disparities, which made them unable to access healthcare due to a lack of resources.
Call To Action
Murray has called for policymakers to take collective action to address the root cause of these disparities. He also urged the US government to invest in healthcare as well as educate people on employment opportunities to break away from the systemic challenges that are contributing to these health inequities.
Western Australia Seniors To Get Free RSV Immunization

Credits: Canva
Western Australia (WA) Government's announcement of older Western Australians living in residential aged care to receive free RSV immunization through a new $2.6 million state-funded program has been welcomed by the Royal Australian College of GPs or the RACGP.
This is a first initiative where the Arexvy RSV vaccine that usually costs around $300 at private hospitals will be made available at no cost to Western Australians aged 65 and over residing in aged care facilities. As per the Depart of Health, there are about 15,000 aged care residents who will benefit by the vaccine this year.
Western Australia Seniors To Get Free RSV Immunization: What Is RSV?
Respiratory Syncytial Virus or RSV is a common, contagious virus that usually causes mild symptoms. In older adults, including those with certain underlying conditions, RSV could cause severe infection. RSV is not a new virus and could be a bigger health concern than many think due to it being highly contagious.
It is a type of respiratory virus that could cause infections of the lungs and the respiratory tracts, It is similar to other respiratory infections when it comes to spreading.
How Does RSV Spread?
It could spread through a cough, sneeze, or by exchange of saliva or using hand to cover a sneeze and not washing it. A person with RSV is typically contagious for three to eight days, for some people with weakened immune system, they could be contagious for four weeks even after they stop showing symptoms.
Western Australia Seniors To Get Free RSV Immunization: What Are The Symptoms?
Symptoms of RSV could appear in three to four days and last up to two weeks. It could range from mild to severe symptoms in older adults. The common symptoms include:
- Fever
- Cough
- Sore Throat
- Runny Nose
- Congestion
- Headache
- Tiredness
Western Australia Seniors To Get Free RSV Immunization: What Is The RSV Season?
The seasonality could vary based on geographic location, population density and even climate activity. However, majority of RSV cases follow the patter:
- Rise from mid September to mid November
- Peak from late December to mid February
- Decline from mid April to mid May
Western Australia Seniors To Get Free RSV Immunization: What Does The Data Say?
RSV is a major winter respiratory illness in Australia that results over 115,000 hospitalizations (2016 to 2019) as per the data presented by the National Centre for Immunisation Research and Surveillance (NCRIS), which is Australia's leading immunization organization. Its data notes that RSV is the leading cause of bronchiolitis and pneumonia in infants, with high rates in those under six months.
As per the official website of Government of Western Australia, in 2025, Western Australia reported 12,804 RSV cases and around a third were in people over 65 who became "very unwell" and required hospital admission. This year's initiative thus aims to lower this number and to protect the seniors form this contagious disease. The Premier of Western Australia Roger Cook said, "Our health system is seeing more patients who are older, sicker and have complex heath needs, reflecting the impact of an ageing population. The RSV immunization program will keep more Western Australians well over the winter months and ease the pressure on our emergency departments."
Lancet study shows experimental oral E coli vaccine can help prevent diarrhea in children

Credit: Canva
An experimental oral vaccine has proven to be safe and effective in generating immunity against the Enterotoxigenic Escherichia coli (ETEC), responsible for 75 million diarrhea episodes and over 40,000 deaths annually in children worldwide, according to a new study published in the journal The Lancet Infectious Diseases.
The vaccine ETVAX -- an oral whole-cell vaccine for ETEC -- consists of inactivated E coli bacteria and is designed to prevent bacterial colonization.
In the phase 2 trial, including nearly 5,000 Gambian children aged 6-18 months, ETVAX was well tolerated. There was no increase in the frequency or severity of adverse events, said an international team of researchers, including those from the London School of Hygiene & Tropical Medicine, in the paper.
"Using active and passive surveillance, we confirmed that ETVAX is safe and induces immune responses to colonisation factors and heat-labile toxins," they added.
Produced by ETEC, heat-labile toxins are sensitive to heat and cause watery diarrhea.
What did the study find?
ETVAX showed to be safe, immunogenic, and also offered protection against moderate-to-severe ETEC diarrhea in the presence of co-pathogens.
Importantly, the study provided the first evidence that ETVAX can significantly reduce the incidence of ETEC-positive and all-cause diarrhea, particularly when vaccination is initiated before age 9 months, and in children without concurrent enteroparasitic infections, the team said.
“This study provides the first demonstration of induction of protective efficacy by ETVAX in young children who are at risk,” the researchers said.
“These findings support progression to a large, multi-country, phase 3 trial to confirm ETVAX efficacy against ETEC disease in children and to support ETVAX introduction in high-burden settings,” they added.
These findings support advancing ETVAX to a pivotal phase 3 trial.
How was the study conducted?
The researchers enrolled children ages six to 18 months to receive ETVAX or a placebo at three timepoints (days 1, 15, and 90).
Serious adverse events occurred in 1.0 percent of the ETVAX group and 1.3 percent of the placebo group, with none related to the vaccine.
Among the 122 children in whom immunity was assessed, the ETVAX, developed by Scandinavian Biopharma, increased antibodies to ETEC colonization factors and heat-labile toxins.
What is ETEC?
Enterotoxigenic Escherichia coli (ETEC) is a pathogenic, toxin-producing strain of E. coli that specifically causes watery, non-bloody diarrhea, commonly known as traveler’s diarrhea.
While most E. coli are harmless gut flora, ETEC uses adhesins to colonize the small intestine and release toxins, whereas "generic" E. coli is usually beneficial or benign.
Annually, ETEC causes 220 million diarrhea episodes globally, with 75 million episodes and up to 42,000 deaths in children younger than 5 years, mainly occurring in low-income countries.
Even as climate models predict increased ETEC incidence under warming conditions, the researcher noted that "an ETEC vaccine could reduce illness and deaths, improve child growth, decrease health-care costs, and curb antimicrobial resistance".
Epstein Files Reveal The Doctors Who Helped Keep His Victims Healthy
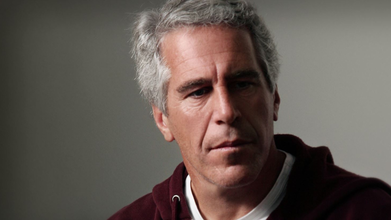
Credit: Canva
Newly released Department of Justice files have revealed that the convicted child sex offender Jeffrey Epstein and his associates kept a roster of doctors to make sure their victims were tested for STDs, prescribed birth-control pills and inoculated against HPV.
The American serial rapist regularly made payments to at least three New York City gynecologists, a dermatologist and his own personal physician. Apart from New York based doctors, physicians in West Palm Beach, New Mexico, and Ohio, all cities where Epstein had set up residences, have also been named in the Files.
The Epstein Files are over six million pages of documents, images and videos detailing the criminal activities of the financier and his social circle of public figures that included politicians and celebrities.
His co-conspirator Ghislaine Maxwell, who is also a convicted child sex trafficker and sometimes referred to as the "Lady of the House" is serving a 20-year prison sentence at a minimum-security prison camp in Texas.
Who Are The Doctors Named In The Epstein Files?
A December 12, 2012 email shows that an associate whose name is redacted but email address matches to Mark Epstein, Jeffrey’s brother, asks the latter, “Do you remember the name of the Gynocologist [sic] that you used to send your victims to?
“Many years ago you used to send them to a gyno in NY who once commented something to the effect that you were keeping him in business singlehandedly,” the sender continued.
Another 2015 email, when an unidentified person asks which gynecologists Epstein regularly uses for “the girls,” Epstein’s former staff member Bella Klein is seen to write back , “S. Yale and Romoff.” “S. Yale”.
According to The Cut, this may reference to the combined practice of Suzanne Yale, an OB/GYN who shared an office with fellow OB/GYN Adam Romoff in Manhattan for about 45 years. Documents show that Epstein made more than half a dozen direct payments to Romoff and Yale, with the last being on March 14, 2019, four months before he was arrested, for $375 check to Women’s Health of Manhattan, Romoff’s current practice.
Romoff, who still practices his profession, is cited in the emails as the physician for a number of the women associated with Epstein, including Karyna Shuliak, his longtime girlfriend and reported beneficiary of his $100 million fortune. His name shows up in the Epstein files 38 times, though he is never shown to be in direct communication with the abuser himself.
READ MORE: Epstein Files Reveal Secret Muffin Recipe: All You Need To Know
Alexander Shifrin, an OB/GYN and women’s integrative health specialist in Manhattan and Brooklyn is also repeatedly mentioned in the emails and text messages.
Dr Steven Victor, a New York City–based dermatologist has also been mentioned multiple times in the Files. According to a 2012 email revealed in the documents, an unnamed woman who was one of Epstein's "girls" discussed seeing Victor to treat her molloscum contagiosium, a viral skin infection that can be spread through sexual contact.
However, he denies knowing of Epstein's wrongdoings and told The Cut: "Most of the patients referred were adults. There were also some younger patients, including minors. In every such instance, they were accompanied by a legal adult guardian. No patient ever disclosed any inappropriate conduct by Mr. Epstein to me or to my staff. Had anyone done so, I would have immediately reported it to the authorities.
" I am appalled and heartbroken by what Mr. Epstein did to young women and children. My involvement with Mr. Epstein was limited to providing dermatologic care to him and patients referred to my practice. I did not participate in, enable, or have knowledge of any criminal conduct."
Epstein’s own physician, Bruce Moskowitz has also been accused of covering up his sexual activities in 2016. Texts between both men from the year show that Epstein had contracted gonorrhea, an STI transmitted through unprotected vaginal, anal, or oral sex., that year and placed on a rigorous antibiotic course.
In 2018, Epstein reached out to Bruce about two of his "friends" having the same STI. "Think to be safe my two friends should get shot by you tomorrow or send them somewhere close,” he wrote. Moskowitz agreed, proposing a location for him to treat them. “That way I do not have to report the cases to health department including contacts,” he wrote.
Are Any Doctors In The Epstein Files Being Investigated?
While it currently remains unclear whether the physicians were aware of Epstein’s criminal activity, Ohio State University head of gynecology is being investigated after being named in the files for allegedly receiving thousands of dollars in payments for consulting work.
The Files show that Mark Landon, a physician and professor at OSU and the chair of the obstetrics and gynecology department, received about $25,000 quarterly from Epstein in the early 2000s.
Additionally, he also received at least 10 separate payments from Epstein or his associates between June 28, 2001, and April 12, 2005. In an email between Epstein and an attorney he worked with, Darren Indyke, Epstein wrote that they were paying Landon $75,000 a year. The email didn't mention what they were paying Landon for.
In 2006, Indyke wrote to Epstein: "Are we still paying Mark Landon?... Eric was dealing with this, so I am not sure what was decided when the previous payment was made. Landon's agreement requires quarterly payments of $30k to be made to Landon on the 15th of January, April, July and October.
"The previous payment made to Landon was for $25,000 and not $30,000. The contract is terminable at will on 15 days' prior notice. Is NYSG to make payment to Landon by January 15th and if so for $25K or $30K? Please advise."
Records show that Epstein also spent over $200 mailing items to Landon’s Columbus home. It remains unclear what was being mailed to the expert.
READ MORE: Epstein Files Raise Questions About Trump’s Memory Decline
According to a Serena Smith, a spokesperson for OSU's Wexner Medical Center, Landon is cooperating with the investigation and had denied knowing Epstein's years of abuse.
"I did not provide any clinical care for Jeffrey Epstein or any of his victims. I was a paid consultant for the New York Strategy Group regarding potential biotech investments from 2001 to 2005. I had no knowledge of any criminal activities; I find them reprehensible and I feel terrible for Epstein’s victims," he said.
The New York Strategy Group was Epstein's money management firm, records show.
Smith added: "[Landon] has stated he had no knowledge of any criminal activities and his consulting work did not involve any patient care. We continue to review the situation and have received no information to date that contradicts Dr. Landon’s statement."
Except for Landon and Victor, no other doctor has commented on being named or being associated to the convicted assaulter.
© 2024 Bennett, Coleman & Company Limited

