- Health Conditions A-Z
- Health & Wellness
- Nutrition
- Fitness
- Health News
- Ayurveda
- Videos
- Medicine A-Z
- Parenting
- Web Stories
Most Common Vaginal Infection May Actually Be An STD, Study Finds
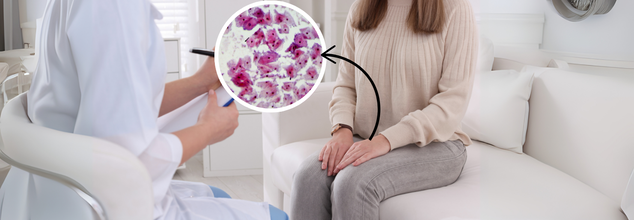
A common but misunderstood vaginal infection that occurs in almost one in three women worldwide is now being re-evaluated as a sexually transmitted disease (STD), according to a new research. Bacterial vaginosis (BV), previously classified as a women's health problem, is often treated in isolation—excluding male sexual partners. But new evidence indicates that not treating both partners could be the explanation for why BV recurs at frighteningly high levels.
Bacterial vaginosis occurs when the vaginal microbiome experiences an imbalance, with a decline in protective bacteria and an increase in harmful bacterial species. This disruption can lead to an unpleasant fishy odor, unusual vaginal discharge, itching, or a burning sensation—although many women experience no symptoms at all. BV is commonly waved off as a simple imbalance and not a real health problem, but it is associated with serious risks such as higher risk of sexually transmitted diseases (STIs), pelvic inflammatory disease, and pregnancy-related complications like premature delivery and low birth weight.
Historically, BV has not been categorized as an STI because its etiological bacteria arise from within the body and not from outside pathogens. But with growing evidence, it now appears that this knowledge was limited, and sexual transmission might be a vital factor in recurrence of BV.
Studies have repeatedly demonstrated that recurrence rates of BV are high—approximately 50% of women have a relapse in the first six months following antibiotic treatment. Reinfection by untreated male partners is a primary cause of these recurrences. Studies have found BV-associated bacteria in the penile skin and male urethra, which supports the theory that men can reinfect their female partners with such bacteria.
An Australian randomized clinical trial supplied strong evidence in favor of the theory. In the study, 164 heterosexual monogamous couples in which the woman had BV were tested. The volunteers were put into two groups: a group where the woman was treated only and a group where both partners were treated. The findings were dramatic—BV recurrence rates fell to 35% in the partner-treatment group versus 63% in the single-woman treatment group. This indicates that treating male partners has a significant impact on preventing BV recurrence.
Why Current BV Treatment Approaches Are Not Working?
Most prior efforts at treating male partners for BV have not demonstrated significant female recurrence rate improvements. But these trials used oral antibiotics only, which might not be enough to completely clear the bacteria from male partners. The new Australian trial was different in that it used a combination therapy: men were given an oral antibiotic and a clindamycin cream to put on the penis. This two-pronged approach seems much more effective, and it shows that there should be a new standard of treatment.
Even with this strong evidence, however, most healthcare providers continue to fail to acknowledge BV as an STI. Infectious disease experts Jack Sobel and Christina Muzny, who did not participate in the research, state that BV is still inaccurately classified as a sexually unrelated condition. This false assumption denies appropriate treatment options that would decrease rates of recurrence and enhance women's long-term health.
Health Risks of Untreated Bacterial vaginosis
Although BV itself is not dangerous, if left untreated, infections can be dangerous. The World Health Organization (WHO) alerts that BV makes a woman more likely to get HIV and other STIs, such as chlamydia and gonorrhea. BV may also cause pelvic inflammatory disease (PID), an infection of the uterus, ovaries, and fallopian tubes, leading to infertility. These risks make it important to adopt a more holistic approach to diagnosing and treating BV.
Considering BV an STI would be a major change in the approach to treating this infection by the medical field. If BV were actually considered an STI, physicians would be incentivized to treat both sexual partners at the same time, and recurrence rates would decrease dramatically, as well as patient outcomes. This change would also work to de-stigmatize BV, moving it from being regarded as a hygiene problem to being recognized as a valid medical condition that can be treated appropriately.
"This effective intervention is cheap and brief and has the potential for the first time to not only enhance BV cure in women, but offers exciting new prospects for BV prevention, and prevention of the severe complications of BV," said Dr. Catriona Bradshaw, a clinician scientist at Monash University and lead author of the research.
More studies are required to validate these results in larger and more diverse populations, but the findings are encouraging. If subsequent studies confirm the sexual transmission theory, international health guidelines may one day be revised to incorporate this new knowledge.
The medical profession is now presented with the task of informing both patients and clinicians of these implications. Greater awareness can lead to improved treatment options, empowering women to become more proactive about their reproductive health as well as engaging male partners in the treatment process.
"It's time to begin the conversation," write Sobel and Muzny. With the promise of preventing recurrence and safeguarding against long-term health consequences, treating BV as an STI could be the answer to dramatically improving women's health globally.
Bacterial vaginosis is the most prevalent vaginal infection, yet it is largely misunderstood. The most recent studies indicate that BV must be categorized and treated as an STI, with the inclusion of male partners in the treatment regimen. This conceptual shift would aid in decreasing rates of recurrence, reduce the risk of complications, and ultimately enhance the health and well-being of millions of women globally. As discussion regarding BV is ongoing, it is crucial that healthcare providers, policymakers, and patients alike become aware of the need for a more holistic and inclusive treatment.
Fact Check: Did Novo Nordisk Executive Faint In Oval Office? Here's What Actually Happened

Credits: X
While TrumpRx is making headlines for lowering the prices of popular weight loss drugs, something else has also grabbed attention of many. A video from the Oval Office from the Thursday Press Conference when President Donald Trump was announcing the deal with the drugmakers, a man had collapsed. Many claimed that the person who collapsed was Gordon Findlay, who is Novo Nordisk's executive. Dr Mehmet Oz, an American present and a physician was swift to check on the man who had collapsed. Independent journalist Eric Daugherty shared the video and wrote: "A man just passed out during President Trump's Oval Office announcement. Dr Oz Sprung into action and assisted him. Pray for him."
Also Read: TrumpRx: Will Trump’s New Website Make Prescription Drugs More Affordable?
Is The Man Gordon Findlay?
The reason why many have identified the man as Gordon Findlay because in the video, David Ricks, CEO of Eli Lily could be heard asking, "You okay? Gordon, you okay?" Upon this, the White House Press Secretary Karoline Leavitt said in the statement that "a representative with one of the companies fainted". However, no names were given.
Novo Nordisk later clarified the claims, and in a statement to Newsweek, the company said, "Please be aware that CEO Mike Doustdar and EVP, US operations, Dave More were the only two Novo Nordisk representatives in the Oval Office."
Dr Oz had previously also helped out at the Oval office in April, when a child fainted while he was being sworn in. A woman, who many media outlets claimed, appeared to be Oz's daughter, Daphne, escorted the girl who had fainted. Later, the White House official confirmed to Fox News Digital that the girl was family member of Oz and had recovered.
What To Do When Someone Collapses?
If someone collapses in front of you, the first need is for someone to try simple CPR or cardiopulmonary resuscitation, while medical help is on its way. What must one keep in mind if someone collapses?
Check for any danger around the person, and give the shoulders of the person who collapsed a shake. Ask them if they can hear you, notes BBC.
If there is no response, tilt their head back to ensure that the airway is clear. This may be enough for the person to again start breathing.
If they are not breathing, this is when CPR becomes important.
Also Read: Trump Strikes Agreement To Cut Costs of Popular Weight Loss Drugs: All You Need to Know
How To Do CPR The Right Way?
As per NHS, UK, there are two correct ways to practice CPR on adults:
Hands-only CPR
This is to be carry out as a chest compression
- Start with kneeling next to the person and place the heel of your hand on the breastbone at the centre of their chest. Place the palm of your other hand on top of the hand that is on their chest and interlock your fingers.
- Position yourself so your shoulders are directly above your hands.
- Using your body weight (not just your arms), press straight down by 5 to 6cm (2 to 2.5 inches) on their chest.
- Keeping your hands on their chest, release the compression and allow their chest to return to its original position.
- Repeat these compressions at a rate of 100 to 120 times a minute until an ambulance arrives or for as long as you can.
CPR with rescue breaths
- Place the heel of your hand on the center of the person's chest, then place the palm of your other hand on top and press down by 5 to 6cm (2 to 2.5 inches) at a steady rate of 100 to 120 compressions a minute.
- After every 30 chest compressions, give 2 rescue breaths.
- Tilt the person's head gently and lift the chin up with 2 fingers. Pinch the person's nose. Seal your mouth over their mouth and blow steadily and firmly into their mouth for about 1 second. Check that their chest rises. Give 2 rescue breaths.
- Continue with cycles of 30 chest compressions and 2 rescue breaths until they begin to recover or emergency help arrives.
TrumpRx Lowered Prices Of Popular Weight Loss Drugs; What More Does Trump's New Medical Website Offer?
Credits: AP and Canva
Ozempic is about to go on sale! With TrumpRx, a website announced by the US President Donald Trump will allow Americans to buy popular weight loss drugs at a cheaper rate. The drugmakers Eli Lilly and Novo Nordisk have agreed to match prices to the lowest paid in peer nations for all their drugs in Medicaid and for the list prices when their medications first hit the market. They will be offering primary care medicines that will reach to customers directly at a discounted price.
While popular weight loss drugs could be bought from the website at as lowest as $149 per month, what else does TrumpRx offer?
In his own words, "By taking this bold step, we are ending the era of global price gouging at the expense of American families."
Not just Novo Nordisk and Eli Lilly, in fact, it was Pfizer, which is the first US pharmaceutical group that signed up to the website. The company said that it would offer discounts of up to 85%. This is for the medicines for those not using health insurance policies to pay and for those on the government's low-cost insurance programme - Medicaid.
When Will TrumpRx Be Launched?
The plan is to launch the website in early 2026 from where consumers could buy prescribed medicines directly from pharmaceutical companies without having to go through insurance. This is also to aid those under the Medicaid programme, which is a federal government programme for adults and children from lower-income backgrounds. The beneficiaries will have access to the drugs at a discounted prices, which is closer to those paid by national health services in foreign countries, known as the "most favoured nation" prices.
What Does "Most Favoured Nation" Prices Mean?
"Most Favoured Nation" or MFN prices are those that the national health services in countries including Canada, France, Germany, Italy, Japan, the United Kingdom, Switzerland and Denmark pay the US pharmaceutical companies for prescribed drugs.
Since these medicines are exported in a bulk, the prices are lowered as the purchasing power is greater to demand of the ordinary consumers. This is why pharmaceutical companies tend to sell their drugs at a lower price outside than in their own country. Earlier this year in May, Trump, thus signed an executive order that aimed at reducing prescription drug prices in the US. He stated, "The United States will no longer subsidise the health care of foreign countries.”
How Does TrumpRx Play A Role?
Apart from the lower drug prices of popular weight loss drugs, Trump, in July had sent letters to CEOs of 17 pharmaceutical companies and ordered them to reduce their prices, based on certain promises from his end, which included:
Manufacturers will be provided with an avenue to cut out middlemen and sell medicines directly to patients
Manufacturers will be supported by trade policy in raising prices internationally
Trump had also announced new 100% tariffs on imported, branded pharmaceutical products, which will allow him to deliver the second promise.
How Will TrumpRx Benefit People?
As per a 2022 study commissioned by the Office of the Assistant Secretary for Planning and Evaluation, which is published on the US government website, the standard insulin prices in the US are 10 times higher than the prices in 33 OECD countries (Organisation for Economic Cooperation and Development). Lowering of the prices of drugs domestically, and removing the middle men could bring the prices down.
The study also found that the average gross prices in US were more than 10 times the price in France, and the United Kingdom. The prices further skyrocketed by nine times in Italy, eight times the prices in Japan, seven times the prices in Germany, and more than six times in Canada.
While many people who take insulin already pay a "net price", which is lower than the standard price, however, the net price is still 2.33 times the price paid in other countries.
TrumpRx, thus, could benefit anyone who buys drugs directly from the website. This is especially for those who do not have a health insurance in the US. As per a 2024 report from the US Census Bureau, around 8%, which makes 26 million of the US population, do not have a health insurance.
Which Medicines Will Be Sold Through TrumpRx?
Apart from Eli Lilly and Novo Nordisk's popular weight loss drugs like Zepbound, Ozempic and Wegovy, Pfizer too has shared a list of primary-care medicine, not limited to the following:
- Eucrisa: topical ointment for atomic dermatitis at an 80% discount
- Xeljanz: an oral medication for types of arthritis at a 40% discount
- Zavzpret: a drug to treat migraines at a 50% discount
- Duavee: to treat menopause symptoms at around an 85% discount.
- Toviaz: a drug for overactive bladder.
TrumpRx: Will Trump’s New Website Make Prescription Drugs More Affordable?

Credits: PTI
TrumpRx: US President Donald Trump had announced this week that his administration plans to roll out a new website, called TrumpRx, which will allow Americans to purchase prescription medications from pharmaceutical companies at discounted rates.
In a major step to address rising drug costs, the Trump administration also unveiled agreements with Eli Lilly and Novo Nordisk to reduce prices for popular GLP-1 medications like Ozempic, Wegovy, and Zepbound. These deals, part of the TrumpRx initiative, are expected to make the drugs more affordable for Medicare, Medicaid, and direct consumers starting in 2026.
Trump Annoucement Today: What Is TrumpRx?
TrumpRx is an online platform designed to let consumers buy prescription medicines directly from the manufacturers, bypassing insurance intermediaries. The website is scheduled to launch in early 2026. Users will be able to search for the specific drug they need and be directed to the drug’s manufacturer, according to USA Today. The platform will offer prices closer to what national health services pay in other countries, following the principle of “most favoured nation” pricing. Medicaid beneficiaries—federal insurance for low-income adults and children—will also have access to the platform.
Also Read: Trump Strikes Agreement To Cut Costs of Popular Weight Loss Drugs: All You Need to Know
TrumpRx: Will The New Website Slash Prescription Drug Prices?
The website is part of a broader effort by Trump to curb high prescription drug costs in the US. In July, he sent a letter to the CEOs of 17 pharmaceutical companies demanding lower prices.
In the letter, he outlined several key points:
- Manufacturers must provide MFN (most favoured nation) prices to all Medicaid patients.
- Companies must ensure that new drugs are not sold at lower prices in other developed nations than in the US.
- Manufacturers will have an option to sell directly to patients, cutting out middlemen, but prices cannot exceed the lowest rates in other developed countries.
- Trade policies will be leveraged to support higher international pricing, with any additional revenue abroad reinvested to reduce costs for American consumers and taxpayers.
TrumpRx: Who Will Benefit Most From This Platform?
Anyone looking to buy prescription drugs directly from manufacturers, rather than through insurance, could benefit. A 2024 US Census Bureau report noted that 8% of Americans (about 26 million people) lacked health insurance in 2023, meaning they could significantly benefit from lower prices. Medicaid may also benefit, as its deal with Pfizer offers better pricing terms. Details about how this part of the program will work are not fully clear yet. Since most Americans rely on insurance for healthcare, experts believe initial adoption of the site may be limited.
TrumpRx: Trump Announces Deal With Drugmakers to Lower Cost of Weight-Loss Drugs
On Thursday, President Trump announced deals with Novo Nordisk and Eli Lilly to cut costs for the lowest doses of their popular weight-loss drugs, lowering barriers for new patients seeking treatment. Beyond government programs, the same GLP-1 drugs will be available directly to consumers via TrumpRx.gov, launching in January 2026.
The starting doses of injectable Wegovy and Zepbound will cost $350 per month but are expected to trend down to $245 over two years. Oral versions, including Novo Nordisk’s upcoming semaglutide pill and Eli Lilly’s orforglipron, will start at $149 per month once approved.
© 2024 Bennett, Coleman & Company Limited

