- Health Conditions A-Z
- Health & Wellness
- Nutrition
- Fitness
- Health News
- Ayurveda
- Videos
- Medicine A-Z
- Parenting
- Web Stories
Parkinson’s Disease May Have A New Environmental Trigger- Can It Be Avoided?

When we consider health risks, we tend to look inward—diet, lifestyle, genetics but what if the biggest threats come from what’s around us? Environmental causes have increasingly been in the primary concern of health studies, with connections being found between pollution in the air and respiratory disease, industrial toxins and cancer, and now perhaps even our most idyllic, verdant neighborhoods. According to a new research, just being close to a golf course may be linked with a much greater risk of acquiring Parkinson's disease.
Yes, golf courses—those enormous, manicured landscapes we commonly think of as tranquility and recreational—might be more poisonous than they seem. The report, which appeared online in JAMA Network Open, sends significant concern about the long-term effects of environmental pesticide exposure on these greens, particularly for those who live nearby. Although far from definitive, the results add fuel to a growing controversy: Might our seemingly picture-perfect environments be quietly undermining brain function?
A research team headed by Brittany Krzyzanowski from the Barrow Neurological Institute investigated whether proximity to golf courses in one's neighborhood could potentially be associated with Parkinson's disease—a chronic neurological condition for which there is currently no cure. Based on a population-based case-control study comprising 419 patients with diagnosed Parkinson's and 5,113 healthy controls across different regions in the US, the researchers found something disturbing- Living in one mile of a golf course was linked with a 126% higher risk of Parkinson's disease compared to those residing more than six miles away.
Additionally, residents of areas where water services encompassed golf course areas had almost double the risk of Parkinson's versus those residing in golf-free areas. These correlations persisted even after controlling for neighborhood and demographic variables.
What Is It About Living Close to Golf Course That's a Red Flag for Your Health?
The research doesn't say golf courses cause Parkinson's directly—but it does propose a compelling hypothesis. The suspected perpetrators are pesticides, which are applied freely to keep golf courses looking nice. The chemicals, frequently airborne or leached into water, might end up being inhaled or ingested by nearby residents.
This hypothesis is not new. Past research has indicated a greater prevalence of Parkinson's in farmers, field workers, and residents of industrial areas. Some lab research has demonstrated that some pesticides and air pollutants are harmful to dopaminergic neurons, the very same cells that in Parkinson's disease.
The new evidence supports the hypothesis that long-term, low-dose exposure to neurotoxic chemicals—particularly by air and water—may play a causative role in causing the illness. But experts caution against overinterpretation.
Not everyone in the scientific community is convinced. Parkinson’s UK, a leading non-profit that supports neurological research, has expressed skepticism about the study's conclusions. Katherine Fletcher, a lead researcher with the organization, notes that while many studies have examined links between pesticide exposure and Parkinson’s, the evidence remains inconclusive.
"Effects have been inconsistent, but in general point toward pesticide exposure possibly elevating risk," Fletcher replies. "The evidence, though, is not as strong to conclude that exposure to pesticides is directly causing Parkinson's."
David Dexter, another Parkinson's UK expert, questions methodology. The study didn't check for true contamination of air or water around the golf courses. Nor did it take into account other possible sources of pollution, such as traffic emissions, that might have an effect on neurological health.
Why it is Important to Rethink Where We Live?
What's most unnerving is the way seemingly wholesome, affluent neighborhoods might harbor hidden health threats. Environmental exposure and disease clusters aren't new. But in contrast to industrial complexes, golf courses are frequently situated in upscale areas, promoted as serene and picturesque.
This paradox makes the new study more intriguing—and more contentious. Although it doesn't have answers, it raises an immediate question: Are we reconsidering the safety of our environment?
Can This Risk of Parkinson's Be Avoided?
For now, there’s no need to panic or sell your home next to the 18th hole. The findings call for further investigation, not alarm. Krzyzanowski and her team argue that public health policies aimed at reducing pesticide use on golf courses could be a step in the right direction. This could include:
- Switching to eco-friendly turf management practices
- Enforcing stricter groundwater monitoring regulations
- Increasing transparency around chemical use in residential areas
Finally, until more conclusive studies, prevention is paramount. If you're near a golf course—or anywhere with intensive pesticide application—it may be a good idea to take note of local water quality summaries and air quality indices.
This research is not the last word on Parkinson's and golf courses—but it begins an essential dialogue. As we swim through the rising tide of diseases caused by the environment, it's more and more apparent that health is not solely the result of genes and behaviors. It's also strongly connected to place.
Fat Loss Jabs No Longer Just About Weight Loss; They Could Also Help Asthma Symptoms in Obese People, Study Finds

Are you in awe of weight loss injections? Well, here is some news. They might be doing more than just helping you lose fat. According to a new study, the same drugs that are helping people drop kilos might also be calming their lungs, specifically in people who are both obese and asthmatic.
If you have heard of Ozempic or Mounjaro, you probably know they are part of a growing class of drugs originally designed for people with type 2 diabetes. These are called GLP-1 receptor agonists (GLP1-RAs), and they work by mimicking a gut hormone that controls blood sugar and, conveniently, appetite. What is new, though, is their potential to help with another major issue, breathing.
The Link Between Asthma and Obesity
According to the American Lung Association, people with a BMI of 30 or higher are much more likely to have asthma. It is not just because the extra weight makes it harder to breathe. Fat tissue itself releases inflammatory chemicals that can mess with lung function.
Meanwhile, asthma can make physical activity feel like a battle, and long-term steroid use can ramp up hunger, meaning it is all too easy to get stuck in a cycle where obesity and asthma fuel each other.
The Study: What They Found
Published in the journal Advances in Therapy, the study looked at health records from over 60,000 people. One group of 10,111 were prescribed GLP1-RAs, while the rest were not.
After a follow-up, the group on the jabs had lost more weight, but they also had better control over their asthma. And the average weight loss was just 0.9 kg over the year. So it was not just about shedding pounds. Something else was clearly at play.
Reportedly, GLP1s work on inflammatory responses in the airways in a different way to traditionally used steroids. In other words, the drug may be doing a direct job on the lungs, not just helping from the sidelines by shrinking waistlines.
Experts Weigh In
Prof Alan Kaplan, chairperson of the Family Physician Airways Group of Canada and the Observational and Pragmatic Research Institute, told The Sun: "Our findings suggest that GLP1-RAs have benefits on asthma control in people with obesity, and this information should contribute to the discussions around the decision to use these drugs."
Dr Erika Kennington from Asthma and Lung UK told the publication that this could be promising for people who feel stuck. "Although exercise can help people lose weight, for some people it can cause anxiety about becoming breathless or having an asthma attack, so people are stuck in a vicious cycle of not being able to lose weight and their asthma worsening."
However, she also sounded a note of caution. "Therefore, where exercise hasn't worked for someone these drugs that support weight loss could offer a promising alternative.
"It's too early to say whether these drugs would be effective for people with asthma more widely.
"More research is needed to understand how these drugs actually improve asthma control. Funding for lung health research is on life support, and urgent action is needed to increase investment."
A Possible Turning Point for Millions
Millions of people in the UK are living with asthma. At the same time, nearly two-thirds of adults in England are overweight or obese. For people stuck between breathlessness and weight gain, these jabs could be a literal breath of fresh air. Still, while the findings are exciting, no one is saying these jabs are a magic fix for everyone with asthma.
Hulk Hogan, The Wrestling Legend, Dies From Cardiac Arrest At 71
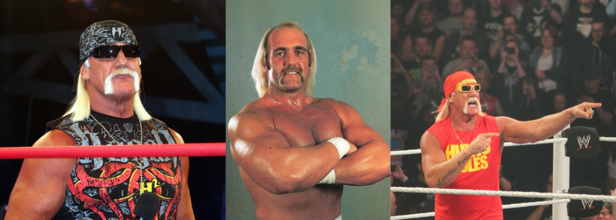
Credits: Wikimedia Commons
Hulk Hogan, the wrestling legend has passed away at the age of 71, according to a report by TMZ Sports. Emergency services were reportedly dispatched to his Florida residence following a 911 call for a suspected cardiac arrest.
TMZ also reported that a video outside Hogan's residence show that the responders had tried to desperately save him while he was being transported to an ambulance. The clip shows that several paramedics were, what it seems like, conducting compression as Hogan was being wheeled to the emergency vehicle.
Hogan's death comes just weeks after his wife publicly denied rumors that the WWE Hall of Famer was in a coma, reassuring fans that his heart was “strong” and that he was recovering well after multiple surgeries.
Widely credited with transforming professional wrestling into a mainstream global phenomenon, Hogan—born Terry Bollea—was more than just a wrestler. With his signature bandana, handlebar mustache, and larger-than-life personality, he became a household name in the 1980s and 1990s, helping to usher in an era when wrestling became part of pop culture.
What Happens During Cardiac Arrest?
Jonathan Chrispin, MD, from John Hopkins Medicine, writes, that a cardiac arrest, also known as a sudden cardiac arrest, in when the heart stops beating suddenly. The lack of blood flow to the brain and other organ can cause a person to lose consciousness, become disabled or die if not treated immediately.
Is cardiac arrest the same as a heart attack? The answer is no, as per the Heart Organization, a heart attack occurs when blood flow to the heart is blocked, whereas in a cardiac arrest, heart suddenly stops beating.
What Are The Symptoms Of A Cardiac Arrest?
In some cases of cardiac arrest, there may be no symptoms at all. You may experience these symptoms prior to cardiac arrest:
- Fatigue
- Dizziness
- Shortness of breath
- Nausea
- Chest pain
- Heart palpitations (fast or pounding heart beat)
- Loss of consciousness
What Causes A Cardiac Arrest?
Common Causes of Cardiac Arrest:
Arrhythmia and Ventricular Fibrillation
Arrhythmia refers to an irregular heartbeat caused by disrupted electrical signals in the heart. One of the most dangerous types is ventricular fibrillation—a rapid, chaotic heartbeat in the ventricles. Instead of pumping blood effectively, the heart quivers, leading to sudden cardiac arrest.
Enlarged Heart (Cardiomyopathy)
Cardiomyopathy occurs when the heart muscle becomes enlarged—either dilated or thickened—resulting in weak or abnormal heart contractions. This condition increases the risk of heart failure and cardiac arrest.
Coronary Artery Disease (CAD)
CAD is caused by plaque buildup that narrows and hardens the coronary arteries, restricting blood flow to the heart. If untreated, it can lead to arrhythmias or heart failure—both of which can trigger cardiac arrest.
Other Potential Causes of Cardiac Arrest
- Severe blood loss
- Valvular heart disease (damage or defects in the heart valves)
- Lack of oxygen (such as from drowning or choking)
- Electrolyte imbalances, particularly high levels of potassium or magnesium, which can disrupt heart rhythm and lead to arrhythmia
Early diagnosis and timely medical intervention are critical in preventing these conditions from progressing to cardiac arrest.
Teddi Mellencamp Health Update: Immunotherapy For Skin Cancer On Hold, Tumors In Lungs And Brain Also Shrink

Credits: Instagram
Teddi Mellencamp Cancer Update: Reality TV star and podcast host Teddi Mellencamp has revealed she is pausing her immunotherapy treatment as part of her ongoing battle with stage 4 cancer.
In an update during the July 24 episode of her podcast Two T’s in a Pod, Mellencamp shared that her body has been struggling to cope with the effects of the aggressive treatment, despite promising results in shrinking tumors.
The 44-year-old former Real Housewives of Beverly Hills cast member detailed that she had not been feeling well for nearly a month and had grown increasingly fatigued and disoriented. “It was kind of shocking to me, and I think mentally it did a lot to me,” she said. “I started asking myself, ‘Why do I feel like I can barely open my eyes or keep my words straight?’”
After undergoing emergency scans and consulting her doctors, Mellencamp was told that the sickness she was feeling wasn’t from the cancer itself, but from the very treatment designed to help her.
Immunotherapy on Hold for Now
Immunotherapy, a treatment that harnesses the body's immune system to fight cancer, has shown signs of success in Mellencamp’s case. Doctors confirmed that the tumors in her lungs and brain were shrinking. “They did a bunch of scans and everything’s looking good, everything’s shrinking,” she said on the podcast.
However, the toll on her body has forced a critical decision, take a break to recover strength.
“So we’re going to take a little break on the immunotherapy to get my body back feeling stronger,” she revealed, adding that she is now on steroids and other medications to stabilize her condition. “I’m doing everything I can to get back to feeling like I can do this.”
She added, “I’ve never once felt this way until recently. And it’s heartbreaking.”
A Long Battle with Skin Cancer
Teddi Mellencamp’s cancer journey began in October 2022 when she was first diagnosed with skin cancer. Over the next year, she underwent multiple biopsies and surgeries, eventually revealing in early 2024 that the cancer had progressed to stage 4 and spread to her brain and lungs.
In February, she underwent emergency surgery to remove several brain tumors. But by April, new tumors had appeared. Despite these setbacks, Mellencamp kept her spirits high. She has also been regularly updating her fans with health progress, including the encouraging news just two months ago that her tumors were visibly shrinking.
“And then today I had the scan where they checked my lungs, and they are shrinking, and one of them has shrunk so much you can barely even see it,” she had shared at the time.
What Is Skin Cancer?
Skin cancer is the abnormal growth of skin cells, most often caused by overexposure to the sun’s ultraviolet (UV) rays. The most common types are basal cell carcinoma, squamous cell carcinoma, and melanoma—the most aggressive form, which can spread to other organs if not detected early.
While treatable in early stages, late-stage skin cancer that metastasizes (spreads to other parts of the body) becomes significantly harder to control. Treatments often include surgery, radiation, chemotherapy, and newer therapies like immunotherapy. Mellencamp’s cancer appears to be an advanced form, as it is in Stage IV and has spread to other parts of her body, requiring constant monitoring and multidisciplinary care.
Despite filing for divorce in November 2024, Edwin Arroyave, her husband has remained by Mellencamp’s side throughout her cancer treatment. “He’s had to step in and help me because I, some days, can’t do it,” she admitted during the podcast. “Nothing’s changed in that other than that [we’re] on hold because of what’s happening to me medically.”
For now, Mellencamp is focusing on recovery and regaining enough strength to resume treatment. “I can do all the things,” she said hopefully. “Just not today—but maybe soon.”
© 2024 Bennett, Coleman & Company Limited



